Disseminated Koch’s as Granulomatous Nephropathy and Solitary Anterior Mediastinal Mass Mimicking a Lymphoma in an Immunocompetent Individual
Ravanasamudram Hariharan Lakshmi1, Riya Kataria2,* and Jayanty Venkata Balasubramaniyan3
1Physician, Department of Internal Medicine (Diabetology), Hariharan Institute of Diabetes, Chennai, Tamil Nadu, India
2Resident Medical Officer, MBBS, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India
3Associate Professor, Department of Cardiology, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India
Received Date: 28/03/2024; Published Date: 20/08/2024
*Corresponding author: Riya Kataria, Resident Medical Officer, MBBS, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India
Summary
An anterior mediastinal mass and granulomatous interstitial nephritis due to disseminated tuberculosis are two rare entities. The causal association between the two is not yet well established in the literature, however, in Southeast Asia where prevalence of tuberculosis is high, it becomes important to consider it as a common aetiology even in healthy individuals. We report a female in her early twenties presenting with hypertensive nephropathy and subnephrotic proteinuria along with an isolated mediastinal mass. On histopathological examination and Gene Xpert, she was diagnosed with disseminated tuberculosis causing granulomatous interstitial nephritis. She was then started on standard antitubercular treatment and showed significant improvement in her symptoms.
Keywords: Cervical adenitis; Granulomatous nephropathy; Miliary tuberculosis; Mediastinal widening; Asymptomatic disseminated tuberculosis
Background/ Introduction
It is usually difficult to diagnose a mediastinal mass considering a wide range of differential diagnoses. Similarly, Granulomatous Interstitial Nephritis (GIN) is a rare entity that can occur as a manifestation of numerous causes. Tuberculosis (TB) is known to have protean manifestations, however, presenting as an isolated mediastinal mass without any parenchymal lesion is extremely rare in an immunocompetent individual [1,2]. We describe here a case of a healthy female in her twenties who presented with an anterior mediastinal mass and active cervical adenitis with GIN due to disseminated TB. She was then treated with Antitubercular Treatment (ATT) under Directly Observed Treatment, Short course (DOTS) and antihypertensives.
Case Presentation
A south-Asian female in her early twenties with no known co-morbidities presented to the emergency with severe headache and progressive exertional dyspnoea for 3 days. She also reported puffiness of face for past 15 days but without any skin rash, joint pain, vomiting, and incomplete emptying of the bladder or frequent micturition. She provided no other history suggestive of any cardiological, respiratory, gastrointestinal, endocrinological, neurological or psychiatric illness. No history of any other drug intake or significant family history was noted. On examination, she was afebrile with a pulse rate of 96 beats per minute. The blood pressure measured in right upper limb in the supine position was 180/110mmHg with an increased respiratory rate. Physical examination revealed periorbital oedema, pallor and bilateral pedal oedema with no lymph nodes palpable. Systemic examination was unremarkable. Ophthalmology evaluation revealed grade I hypertensive retinopathy.
Investigations
Routine laboratory investigations including complete blood count, blood glucose, HbA1c, serum electrolytes and liver parameters were within normal limits. Serum creatinine was elevated to 1.4mg/dL while estimated glomerular filtration rate was reduced to 54mL/min. Serum uric acid, calcium and inorganic phosphorus values were normal. Lipid profile showed abnormally high total cholesterol levels to 323mg/dL, triglycerides at 215mg/dL, and low-density lipid (LDL) cholesterol at 269mg/dL with near normal high-density lipid (HDL) cholesterol. Urine analysis revealed proteinuria with total protein excretion of 2.75g/day and urine creatinine levels decreased to 30mg/day.
Ultrasonography revealed regular sized kidneys with normal corticomedullary differentiation. Doppler of renal vessels was unremarkable. Chest X-ray showed an unexpected mediastinal widening of 10cm, suggestive of a mediastinal tumour (Figure 1) Computed tomography (CT) scan was done which revealed a lobulated minimally enhancing soft tissue lesion of size 7 x 6.3 x 4.7 cm, in the pretracheal and right paratracheal region abutting the superior vena cava, arch of aorta and trachea. A similar lesion of size 5.2 x 4.8 x 3.8 cm was noted in the sub-carinal region of posterior mediastinum. The radiological evidence was suggestive of a lymphoma. Additionally, lactate dehydrogenase levels were elevated to 968 U/L (220-450 U/L). In view of suspected lymphoma, peripheral smear was done which was reported as normal. Serology and autoimmune markers along with serum angiotensin converting enzyme (ACE) levels were unremarkable.
The patient was then subjected to a whole-body positron emission tomography (PET) scan, which showed metabolically active level IV cervical nodes on the right side along with enlarged and conglomerate mediastinal and right hilar nodes. (Figure 2) The nodes mentioned were homogenous with no evidence of calcifications. Furthermore, bulky bilateral kidneys with heterogenous hyperintensities were noted in T2- weighted sequence (T2W1) in the medulla. Diffusely increased parenchymal metabolic activity was seen in both the kidneys, suggestive of infiltrative lesions.
Finally, a CT-guided biopsy of the mediastinal lymph node was done which showed granulomatous necrotizing inflammation, further confirmed by CBNAAT (Gene Xpert) that was positive for Mycobacterium tuberculosis. Ultrasound-guided percutaneous renal biopsy was performed that was indicative of membranous nephropathy with positive IgG and C3 along with granulomatous interstitial nephritis.
Outcome and Follow-Up
She was diagnosed with Disseminated Kochs with membranous and granulomatous nephropathy with secondary hypertension. ATT along with maintenance antihypertensives were started on the patient. She had an uneventful recovery and was advised ATT for 6 months under DOTS and antihypertensives till the resolution of symptoms. The patient is currently well after 1 year of recovery.
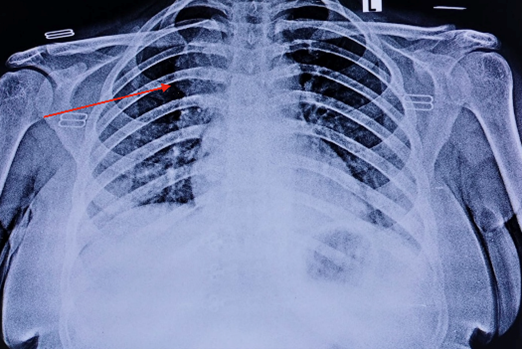
Figure 1: Antero-posterior projection of the chest X-ray showing a widening (arrow) of about 10cm in the mediastinum.
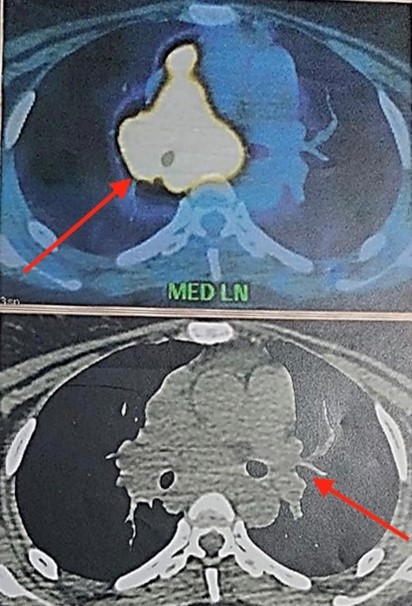
Figure 2: PET scan showing metabolically active and enlarged homogenous mediastinal lymph nodes (arrows) with an absence of calcifications.
Discussion
Tuberculosis (TB) is caused by Mycobacterium tuberculosis when the bacilli laden droplets are inhaled, ingested or enters the human body through the skin (aberration or local trauma) or the mucous membranes, with the most common pathway being the respiratory tract (70%-80% cases) [3,4].
The course of the disease is mainly directed by the interaction between the host response and the virulence of the bacilli. In an immunocompetent host, the organism is initially subjected to fierce resistance from the body’s immune system, making the TB bacilli dormant, also known as latent TB. The vital host defence mechanism against the organism is cell-mediated immunity that is influenced primarily by means of macrophages and T-lymphocytes [3-5]. Once the organism overpowers the defence mechanism of the host, usually in an immunocompromised state, TB can reactivate causing widespread damage either locally or affect other parts of the body after spreading via lymphatics or bloodstream [6-8].
The incidence of isolated tuberculous mediastinal lymphadenopathy declines with increasing age and is scarcely seen in adults [9]. Ayed et al. also reported the occurrence rate of intrathoracic tuberculous lymphadenitis to be as 2% out of 1700 new cases of TB over a period of 4 years. [10] The differential diagnoses of anterior mediastinal mass include thymoma, lymphoma, teratomatous neoplasms, thyroid mass, vascular masses, lymphadenopathy due to metastasis or TB, and pleuropericardial and bronchogenic cysts. Nevertheless, in younger individuals like our patient, lymphoma and germ cell tumours are more common [11].
Genitourinary TB (GUTB) is the second most common form of extrapulmonary TB after lymphadenopathy and accounts for almost 27% of nonpulmonary cases worldwide [12]. The few reported types of glomerulonephritis due to TB include immune complex glomerulonephritis complication of miliary TB and pulmonary TB, membranoproliferative glomerulonephritis in the course of disseminated TB, membranous nephropathy associated with TB, IgA nephropathy associated with pulmonary TB and collapsing glomerulopathy with pulmonary TB. [13-20] In all these reports, there was some degree of lung lesions and clinical and radiological evidence of pulmonary infection unlike in our patient who remained asymptomatic.
Moreover, data on GIN as the only manifestation of renal TB is limited in the literature. GIN is an infrequent diagnosis encountered in less than 1% of all renal biopsies performed. [21,22] Recently, Colvin et al. reported only 34 cases of GIN from a total of 10,383 renal biopsies, with the commonest aetiology of GIN as drug allergy closely followed by sarcoidosis and only one case of TB [21]. On the contrary, reports from Southeast Asia reveal TB as an important cause of GIN [23]
Another interesting consideration is the clinical presentation of hypertension, facial oedema and subnephrotic range of proteinuria mimicking a glomerular disease. Similar presentation of GIN with membranous nephropathy has been reported only twice in the literature [24,25]. In our case, detailed evaluation of other aetiologies like infection, autoimmune disorders and systemic conditions such as sarcoidosis revealed negative results.
Previously, a few cases of GIN associated with pulmonary or peritoneal foci have been reported, albeit rare, but active cervical adenitis with GIN due to TB has been reported only once to the best of our knowledge. [26] It can be hypothesized that our patient had a primary infection involving the cervical and mediastinal lymph nodes and kidneys.
As a part of the initial evaluation, a detailed history along with physical examination is pertinent to look for any thyroid pathologies, testicular/ovarian masses, or evidence of immunosuppression. Usually, patients with a mediastinal mass would remain asymptomatic unless they develop mass effects like chest pain, dyspnoea or cough. It can be very perplexing to diagnose a mediastinal mass radiologically. [3] Gene Xpert analysis is another well-recognized modality in rapid diagnosis of tuberculosis and should be considered in the work up of a mediastinal mass. Contrast enhanced CT of the thorax is useful to further characterize a mediastinal mass [27]. Since TB tends to mimic malignancy mainly radiologically, it is imperative to confirm the diagnosis by histopathology before any therapeutic interventions [27].
In our case a lymphoproliferative disorder was suspected initially along with systemic severe hypertension leading to hypertensive nephropathy. The final diagnosis was of TB was only made after the histopathological examination of mediastinal lymph node biopsy which was finally confirmed by a positive response to ATT. Furthermore, renal survival in GIN is determined by the degree of renal dysfunction at presentation. [28] It is often difficult to diagnose, and non-specific symptoms of genitourinary TB can lead to a delayed diagnosis and rapid progression to a non-functioning kidney.
Conclusion
- Despite a wide range of differential diagnoses for both mediastinal lymphadenopathy and GIN, TB should be considered as a possible aetiology in an immunocompetent adult even with an absent parenchymal involvement especially in countries like India.
- The discordance between the clinical presentation and investigative evidence of TB can at times interfere with an accurate diagnosis. Histopathology complemented by Gene Xpert analysis can help in rendering the diagnosis and preventing various complications.
- Early diagnosis followed by prompt treatment is essential to prevent progression of GIN to complete renal failure.
Authors’ contribution: RK contributed towards literature search, data collection, and drafting of the article while RHL and JVB contributed towards data collection, important content writing and final editing of the article. Final approval of the article was done by JVB.
Ethical clearance was not needed.
No external funding taken.
References
- Kim HY, Song KS, Goo JM, Lee JS, Lee KS, Lim TH. Thoracic sequelae and complications of tuberculosis. Radiographics, 2001; 21(4): 839-858.
- Hadlock FP, Park SK, Awe RJ, Rivera M. Unusual radiographic findings in adult pulmonary tuberculosis. American Journal of Roentgenology, 1980; 134(5): 1015-1018.
- Webb WR, Higgins CB. Thoracic imaging: pulmonary and cardiovascular radiology. Lippincott Williams & Wilkins, 2011.
- Webb WR, Muller NL, Naidich DP. High-resolution CT of the lung. Lippincott Williams & Wilkins, 2014.
- Ellner JJ. The immune response in human tuberculosis: implications for tuberculosis control. The Journal of infectious diseases, 1997; 176(5): 1351-1359.
- Boonsarngsuk V, Saengsri S, Santanirand P. Endobronchial ultrasound-guided transbronchial needle aspiration rinse fluid polymerase chain reaction in the diagnosis of intrathoracic tuberculous lymphadenitis. Infectious Diseases, 2017; 49(3): 193-199.
- Miller WT, Miller Jr WT. Tuberculosis in the normal host: radiological findings. In Seminars in roentgenology. WB Saunders, 1993; 28(2): pp. 109-118.
- Aljohaney AA. Utility and safety of endobronchial ultrasound-guided transbronchial needle aspiration in patients with mediastinal and hilar lymphadenopathy: Western region experience. Annals of Thoracic Medicine, 2018; 13(2): 92.
- Singh S, Pandey D, Ahmad Z, Bhargava R, Hameed I, Mehfooz N. Unusual presentation of tuberculosis. Tropical doctor, 2009; 39(3): 183-184.
- Ayed AK, Behbehani NA. Diagnosis and treatment of isolated tuberculous mediastinal lymphadenopathy in adults. The European journal of surgery, 2001; 167(5): 334-338.
- Strollo DC, de Christenson ML, Jett JR. Primary mediastinal tumors. Part 1*: tumors of the anterior mediastinum. Chest, 1997; 112(2): 511-522.
- Corbishley CM, Crange JM. Tuberculosis and the kidney. J Am Soc Nephrol, 2001; 12(6): 1307-1314.
- Shribman JH, Eastwood JB, Uff J. Immune complex nephritis complicating miliary tuberculosis. British Medical Journal (Clinical research ed.), 1983; 287(6405): 1593.
- O’Brien AA, Kelly P, Gaffney EF, Clancy L, Keogh JA, Brian Keogh JA. Immune complex glomerulonephritis secondary to tuberculosis. Irish Journal of Medical Science, 1990; 159: 187.
- Meyrier A, Valensi P, Sebaoun J. Mesangio-capillary glomerulonephritis and the nephrotic syndrome in the course of disseminated tuberculosis. Nephron, 1988; 49(4): 341-342.
- Pecchini F, Bufano G, Ghiringhelli P. Membranoproliferative glomerulonephritis secondary to tuberculosis. Clinical nephrology, 1997; 47(1): 63-64.
- Rodriguez-Garcia JL, Fraile G, Mampaso F, Teruel JL. Pulmonary tuberculosis associated with membranous nephropathy. Nephron, 1990; 55(2): 218-219.
- Cohen AJ, Rosenstein ED. IgA nephropathy associated with disseminated tuberculosis. Archives of internal medicine, 1985; 145(3): 554-556.
- Keven K, Ulger FA, Oztas E, Ergün I, Ekmekci Y, Ensari A, et al. A case of pulmonary tuberculosis associated with IgA nephropathy. The international journal of tuberculosis and lung disease: the official journal of the International Union against Tuberculosis and Lung Disease, 2004; 8(10): 1274-1275.
- Coventry S, Shoemaker LR. Collapsing glomerulopathy in a 16-year-old girl with pulmonary tuberculosis: the role of systemic inflammatory mediators. Pediatric and Developmental Pathology, 2004; 7(2): 166-170.
- Colvin RB, Traum AZ, Taheri D, Jafari M, Dolatkhah S. Granulomatous interstitial nephritis as a manifestation of Crohn disease. Archives of Pathology and Laboratory Medicine, 2014; 138(1): 125-127.
- Joss N, Morris S, Young B, Geddes C. Granulomatous interstitial nephritis. Clinical Journal of the American Society of Nephrology, 2007; 2(2): 222-230.
- Naidu GD, Ram R, Swarnalatha G, Uppin M, Prayaga AK, Dakshinamurty KV. Granulomatous interstitial nephritis: our experience of 14 patients. Indian Journal of Nephrology, 2013; 23(6): 415.
- Suzuki Y, Hasegawa H, Ushiyama E, Inomata A, Satoh H, Ogino S, et al. A case of nephrotic syndrome with membranous nephropathy and renal tuberculous granuloma. Nihon Naika Gakkai zasshi. The Journal of the Japanese Society of Internal Medicine, 1989; 78(8): 1181-1186.
- Ram R, Swarnalatha G, Desai M, Rakesh Y, Uppin M, Prayaga A, et al. Membranous nephropathy and granulomatous interstitial nephritis due to tuberculosis. Clinical nephrology, 2011; 76(6): 487.
- Kaul AK, Sharma R, Krishnasamy J, Ruhela V, Kumari N. Rapidly progressive renal failure—a rare presentation of granulomatous interstitial nephritis due to tuberculosis—case report and review of literature. Nephrology Dialysis Transplantation Plus, 2011; 4(6): 383-385.
- Maguire S, Chotirmall SH, Parihar V, Cormican L, Ryan C, O’Keane C, et al. Isolated anterior mediastinal tuberculosis in an immunocompetent patient. BMC Pulmonary Medicine, 2016; 16: 1-4.
- Agrawal V, Kaul A, Prasad N, Sharma K, Agarwal V. Etiological diagnosis of granulomatous tubulointerstitial nephritis in the tropics. Clinical kidney journal, 2015; 8(5): 524-530.

