Anencephaly in Dichorionic Diamniotic Twin Pregnancy
Insumbo P, EL Mabrouk F, Nacocam MDB, Bidanmone EKC, Ferreira BI, Haddad S EL, Allali N and Chat L
Department of radiology, Pediatric hospital, UHC IBN Sina Mohamed V University Rabat, Morocco
Received Date: 10/03/2024; Published Date: 30/07/2024
*Corresponding author: Paulino Insumbo, Department of radiology, Pediatric hospital, UHC IBN Sina Mohamed V University, Rabat, Morocco
Abstract
Neural Tube Defects (NTDs) are birth defects caused by failure of the neural tube to close completely, resulting in incomplete formation of the brain or spinal cord (Botto et al., 1999; Mitchell et al., 2004). The two most common types of NTDs are anencephaly and spina bifida.
Anencephaly or cranium bifida also referred as acrania is a characterized by absence of the conception of the skull, scalp and the brain. This defect can be diagnosed during antenatal period during ultrasound morphological routine test. In our case, it's an unattended twin pregnancy in a multiparous patient who came for a usual ultrasound morphological test. The sonographic scan finds out an uncomplete cranial neural tube with a totally absent brain and skull, type anencephaly.
Keywords: Anencephaly; Ultrasounds diagnosis; Dichorionic twin pregnancy
Introduction
Anencephaly is a neural tube defect with an estimated prevalence around 3 per 10,000 births, depending on different geographic regions, ethnic groups, and environmental exposures [1].
It is defined as a complete or a partial agenesis of the cranium.
In fact, the cerebrum, cerebellum, and basal ganglia are absent but the brainstem remains.
The bony structures of skull are absent and basal bones of the face and facial features are preserved[2].
This affection is not compatible with survival after birth and sonography is an excellent exam to diagnosing it in fetal period during the first and second trimesters of pregnancy at 100%[3].
Case Presentation
A 45-year-old woman with no coexisting diseases, who gave birth to 4 children by vaginal delivery without complications. She reports no previous malformations. She has no consanguineous marriages and uses no contraception.
Also, the interrogation did not reveal any drug addiction, active smoking or alcoholism.
The patient was referred to our department for fetal morphology ultrasound as part of a routine prenatal check-up, as the date of her last menstrual period was unclear.
Ultrasound scan revealed a dichorionic diamniotic twin pregnancy, with normal placental insertion.
The large cistern was measured at 6mm, showing sufficient amniotic fluid. The Cord insertion was correct, with 2 arteries and one vein. Biometric measurements of the first fetus (GA) enabled us to estimate the gestation of the pregnancy at 21 weeks (Figure 1). It showed harmonious development and satisfactory growth compatible with term. Organ evaluation of the first male fetus showed satisfactory development and normal cardiac activity measured at 131 bmps. No abnormalities or malformations were observed.
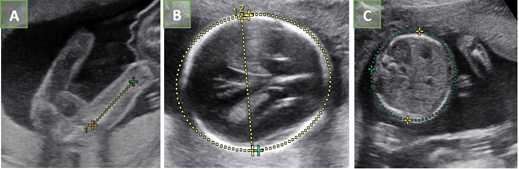
Figure 1: Sonogram of the first fetus (GA) showing its normal mensuration of the femur (A) the cranial perimeter (B) and the abdominal perimeter (C).
The second fetus (GB) showed growth retardation compared to the first one. The body and four members were found. There was no abdominal wall defect.
However, the head presented an unusual irregular head morphology. The coronal image shows no ossified calvarium, no front bone also the cerebral and cerebellar hemispheres weren’t visualized beyond the area of the forehead. The sagittal plane of the face shows the remain of the brainstem floating with moderate echogenicity, limiting the top of the head which is directly covered with skin. This aspect is called “area cerebrovasculosa”.
In contrast with the brain agenesis, the facial structures were respected. The normal appearing orbits with the minimal skull volume reveal protruded eyeballs reminding “the bulging eyes” aspect.
No spinal cord malformations were associated.
Femur diaphysis length was 25mm and abdominal circumference 180mm, compatible with a sonographic estimate of 18 menstrual weeks.
The amniotic fluid volume was increased.
Pathologically, this fetus showed features typical of anencephaly with no rachischisis in a dichorionic pregnancy.
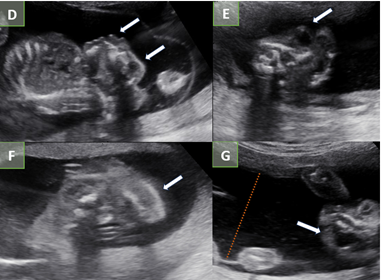
Figure 2: Ultrasound scans showing the second anencephalic fetus (GB) with excessive amniotic fluid.
D Sagittal plan showing the facial structures the arrows are pointing the nose and the eyes.
E and G are coronal plans showing prominent eyes in front of the “area cerebrovasculosa” with hydramnios (G).
F is showing a short femur of the (GB) comparing to (GA).
Discussion
Anencephaly is the most common neural tube defects spectrum that are detectable at 100% prenatally during second and third trimester [4]. It can be detected around the 11th week of pregnancy but confirmed after the 16th week. Sonographic scan is largely satisfying to confirm anencephaly and no need to investigate more unlike other neural defects or cerebral malformations which are best characterized by MRI. Also, amniocentesis is recommended in order to detect chromosomic and genetic abnormalities which can be avoided in ulterior pregnancies.
This defect happens during the third to fourth weeks of development, leading usually to neonatal death[5]. It is a multifactorial pattern of transmission, with interaction of multiple genes such as methylenetetrahydrofolate reductase (MTHFR) that seems to be associated with the risk of NTDs, chromosomal abnormality or environmental factors such as Folate antimetabolites, maternal diabetes specially type 1, obesity and hyperthermia.
It also can be related to defects or disruption of the amniotic membrane associated with complex protein gene called VANGL1 [6].
Acrania is a serious developmental defect of the central nervous system in which the structures derived from the forebrain and skull are grossly malformed. There is no ossification of the calvarium. Sonography scan shows that the forebrain and the cerebellum are absent and replaced by rudimentary mass of connective and vascular tissue (including choroid plexus) with floating neural elements called angiomatous stroma or the area cerebrovasculosa corresponding to the brainstem which is less severely involved. Diencephalon can be affected to various degrees.
The facial bones and skull base above are nearly normal [7]. The eyes and orbital plates are preserved and appear prominent on sonograms drawing an “eyes frog” image called bulging eyes [8].
Furthermore, hydramnios occurs frequently in anencephaly pregnancy because of the absence of the hypothalamic hypophyseal pathway which controls the fluid and electrolytic balance and exchange.
Also, a Belgian study gathered all published anterior studies and case reports between January 1987 and January 2007 and found that anencephaly’s incidence is higher in monochorionic twins than in dichorionic twins [9].
Folic acid has been shown to be an efficacious preventive agent and reduce anencephaly’s incidence event. Its’ supplementation during future pregnancies is recommended mainly with multiparity mother. The U.S. Public Health Service recommends that women capable of becoming pregnant consume 400 µg of folic acid per day for NTD prevention [10,11].
Conclusion
Anencephaly is a fatal malformation incompatible with life due to cranial neural tube defect. It can be associated or not with spina bifida which both are most common NTDs. Sonography is the best investigation to diagnose it and confirm it at the second trimester. It is less frequent in dichorionic twin pregnancy and may be complicated by hydramnios implicating a continuous control. Actually, it’s a multifactorial malformation which can be prevented by the supplementation of folic acid during pregnancy.
References
- Williams J, Mai CT, Mulinare J, et al. Updated estimates of neural tube defects prevented by mandatory folic acid fortification - United States, 1995-2011.
- Ana Monteagudo. Society for Maternal-Fetal Medicine. Exencephaly-anencephaly Sequence-SMFM. SMFM Anomalies Consult Series #3. Am J Obstet Gynecol, 2020. doi: 1016/j.ajog.2020.08.041
- Edwards L, Hui L. First and second trimester screening for fetal structural anomalies. Semin Fetal Neonat Med, 2018; 23: 102–111. doi: 1016/j.siny.2017.11.005
- Rossi AC, Prefumo F. Accuracy of ultrasonography at 11e14 weeks of gestation for detection of fetal structural anomalies: a systematic review. Obstet Gynecol, 2013; 122: 1160e7. doi:1097/AOG.0000000000000015
- Russell SA, McHugo JM, Pilling D. Cranial abnormalities. Twining P, McHugo JM, Piling D. Textbook of Fetal Anomalies. 2nd ed. Churchill Livingstone Elsevier, 2007; 95-141.
- Kibar Z, Torban E, McDearmid JR, Reynolds A, Berghout J, Mathieu M. Mutations in VANGL1 associated with neural-tube defects. N Engl J Med, 2007; 356(14): 1432. doi:1056/NEJMoa060651
- Ruth B Goldstein, Roy A Filly, Peter W. Callen. Sonography of anencephaly: Pitfalls in Early Diagnosis. J Clin Ultrasound, 1989; 17: 397-402. doi:1002/jcu.1870170603
- Virapongse C, Sarwar M, Bhimani S, et al. Computed tomography in the study of the development of the skull base. 2. Anencephaly, the aberrant skull form. J Comput Assist Tomogr, 1985; 9: 95-102. doi: 1097/00004728-198501000-00019.
- Saga HJ, Desa DJ. The relationship between hydramnios and some characteristics of the infant in pregnancies complicated by fetal anencephaly. The Journal of’ Obsterrics and Gynaecology of the British Commonwealth, 1973; 80: pp. 429-432.
- Annelies Lust, Luc De Catte, Liesbeth Lewi, Jan Deprest, Philippe Loquet, Roland Devlieger. Monochorionic and dichorionic twin pregnancies discordant for fetal anencephaly: a systematic review of prenatal management options. prenatal diagnosis Prenat Diagn, 2008; 28: 275–279. doi: 1002/pd.1967.10.1002/pd.1967
- Cordero AM, Crider KS, Rogers LM, Cannon MJ, Berry RJ. Optimal serum and red blood cell folate concentrations in women of reproductive age for prevention of neural tube defects: World Health Organization guidelines. MMWR Morb Mortal Wkly Rep, 2015; 64(15): 421-423.

