Lymphome Non-Hodgkin De Burkitt Ileocecal a Children After Two Evagination
Paulino Insumbo*, Kessi E, Sqalli Houssani Y, Domiciano BN Mango, Papys Mendes, Rabileh YMM, El Haddad S, Allali N and Chat L
Department of radiology, Pediatric hospital, UHC IBN Sina Mohamed V University Rabat, Morocco
Received Date: 09/03/2024; Published Date: 29/07/2024
*Corresponding author: Paulino Insumbo, Department of radiology, Pediatric hospital, UHC IBN Sina Mohamed V University, Rabat, Morocco
Abstract
Non-Hodgkin’s lymphoma is a heterogeneous group of tumors linked to a blocked differentiation and malignant proliferation of B, T, or NK limphocytes precursors [1]. Burkitt lymphoma is the third cause of cancer in children, represent approximately 10 à 15% of pediatric cancer [3]. It is a rare disease with an estimated incidence of 1 case per 40,000 children. Recognized risk factors are congenital or acquired immune deficiencies. Boys are more affected than girls. The diagnosis is made by pathological anatomie study through biopsy, but imaging plays a very important role for the location and size of the tumors, the prognosis is following favorable and the tumor is chimiosensitive. The purpose of this manuscript was to report a case of small mass neglected by surgeons in case of suspiected invagination in children [5].
Clinical Image
Burkitt’s lymphome represents a heterogeneous cluster of lymphoid proliferation of malignant type B cells, in particular, primary intestinal lymphomas represent about 15-20% of gastrointestinal lymphomas [2]. Burkitt lymphoma is a rare and aggressive non-Hodgkin lymphoma with three types, we present a case of sporadic burkitt locate in the ileocecal abdomen [4]. This is a 3-year-old and 3 mounths, child who was brought by family members to the surgical emergency. Department of the peditric hospital in rabat with abdominal pain, paralysis of materials and gauze, accompanied by food vomiting, on physical examination, a masse in the FID, with a history of two episodes of invagination, when he was two years old and the last time, he underwent surgery appendectomy and visualization of a small nodule at the level of the serosa of last ileal loop, tha was not withdrawn. Abdominal ultrasound was requested, echographiic scanning a voluminous abdominal mass on the right, roughly oval, well limited, with lobulated contours, heterogeneous echoes, contain hyperchoic zones ganerating a posterieor cone of shadow, vasclarization with color doppler, (Figure 1).
Ultrasound figures
On the same day an TAP scanner was made that shows significant thickening of the ileocaecal intestinal wall, obstructing the lumen of the ascending colon, giving the appearance of a bulky intra-abdominal mass lterality on the right, well-defined oval, heterogeneous enhancement after injection of the contrast product, (Figure 2) with presence of solitary adenopathy, and absence of lesion at the level of the blow passing for thoracic, absence of effusion nor lesion hepatic.
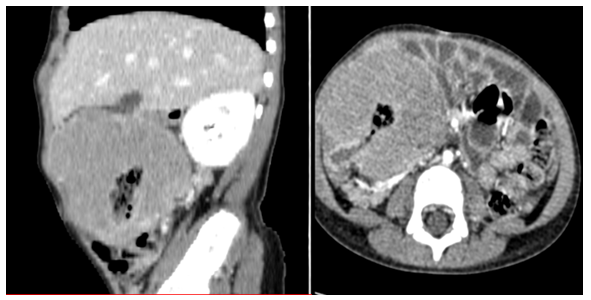
Figure 1: Sagittal Bulky mass exerting mass effect on the inferior vena cava, which remains permeable, in contact with the psoas muscle, the ascending colon, in intimate contact with the lower pole of the liver and the abdominal wall.
After three chemotherapy sessions, the child presented for the ultrasound control a little physically tired with the persistence of thickening of the ileo-caecal wll, creating a bulky mass but easily enhanced after injection of the contrast product (Figure 2).
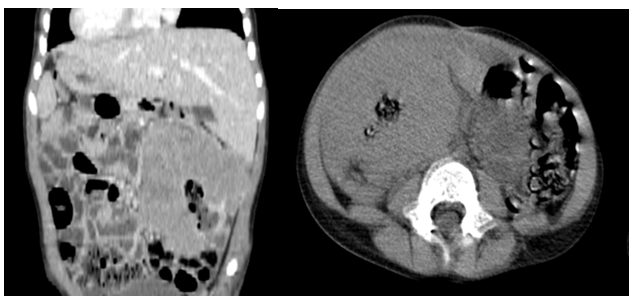
Figure 2: Post-chemotherapy ultrasound.
Conclusion
Lymphomas of the gastrointestinal tract are the most common type of primary extranidal lymphoma, accounting for 5% to 10% of all non-Hodgkin lymphomas. In particular, primary intestinal lymphomas account for approximately 15-20% of gastrointestinal lymphomas. The Burkitt lymphoma is highly chemo sensitive. New multimodal therapeutic approaches have improved the prognosis of this once-deadly disease.
References
- Hans Peter Wagner. Malignant non-Hodgkin lymphomas in children, 2007.
- Alison C Harris, Kelly A MacLean, Gilat L Grunau, Silvia D Chang, Nancy Martin. Imaging Intra-abdominal Burkitt’s Lymphoma: From Discrete Bowel Wall Thickening to Diffuse Soft Tissue Infiltration. Sage Journals, 2016; 68(3). https://doi.org/10.1016/j.carj.2016.08.007.
- John T Sandlund. Childhood lymphoma. Info cancer. Non-hodgkin lymphoma in children.
- Suheil Albert Atallah-Yunes, Dermant J Murphy, Ariela Noy. HIV- associated Burkitt lymphoma. Lancet Haematol, 2020; 7(8): e594-e600. doi: 10.1016/S2352-3026(20)30126-5.
- Brichon P, Bertrand Y, Plantaz D. Lymphome de Burkitt révélé par une invagination intestinale aiguë chez l’enfant, 2001; 126(N°7): P. 613-723.

