Pilocytic Astrocytoma Located in Medulla Oblongata in Pediatric Age
Paulino I*, Jellal S, Domiciano BNM, Kessi Eric MC, Madina Rabileh Y, El Mandour G, Chat PR, Allali PR and Addad PR
Department of radiology, Pediatric hospital, UHC IBN Sina Mohamed V University Rabat, Morocco
Received Date: 09/03/2024; Published Date: 25/07/2024
*Corresponding author: Paulino Insumbo, Department of radiology, Pediatric hospital, UHC IBN Sina Mohamed V University, Rabat, Morocco
Abstract
PA, of the bulbe is extremely rare and a very gloomy prognosis are the most common benign brain tumour in children and adolescents. Represents about 30% of all posterior cerebral fosse. Clinical data accompanied by Magnetic Resonance Imaging (MRI) and scanner combined with an intravenous contrast agent is particularly suitable for visualizing pilocytic astrocytoma and differentiating them from surrounding healthy brain tissue but currently been introduced diagnostic based on morphology, immunohistochemistry and the presence of key genetic alterations [1]. The treatment is always surgical with resection may provide reasonable prolongation of survival. This article is to show the circumscribed and rare forms of pilocytic astrocytoma located in the bulb.
Keyword: Astrocytoma pilocytic centered on medulla oblongata
Clinical Image
Imaging techniques play a key role in the diagnosis of pilocytic astrocytoma. Magnetic resonance imaging (MRI) and scanner combined with an intravenous contrast agent is particularly suitable for visualizing pilocytic astrocytoma and differentiating them from surrounding healthy brain tissue. This is 5-year-old patient wilh a private history, who was brought to the radiology services of the pediatric hospital, by his family members, who presented two months ago with diplopia, headache, accompanied by vomiting, vertigo ataxic gait, etc., oculomotor paralysis.
Pilocytic Astrocytoma (PA) Amount the most common primary benign tumors, they are low-grade tumors according to the classification of the world cerebral tumor [2]. A PA develops from certain star-shaped brain cells called astrocytes. Astrocytes and similar cells form tissue that surrounds and protects other nerve cells found within the brain and spinal cord, tumor. Symptoms of a PA will vary depending upon the size and also of location of the tumor. Symptoms resulting from this pathology we can mention increased pressure on the brain and include headaches, nausea, vomiting, balance problems and vision abnormalities [3,4]. The tumor is most often located in the cerebellar hemisphere, but in our case, it’s a expansive process of BCF, centered on the bulb, with dual tissue (Figure 2), component in hypersignal T2 and FLAIR, heterogeneously enhanced after injection of PC and a cystic component in hypersignal T2, hyposignal T1 and diffusion b 1000, intermediate signal in FLAIR, enhanced in the periphery after injection of PC. It is surrounded by a discrete perilesional edema in hypersignal T2 and FLAIR and exerts a mass effect on the lower part of the V4 which is collabée, as well as on the cerebellar tonsils, pushed back. It is responsible for an erasure of the peribulbar cisterns, with filling of the occipital hole. MRS shows a moderate reversal of the choline/NAA ratio, with the presence of inositol peaks and short-echo lactates. Absence of ventricular sus tentorial dilatation. Absence of intraparenchymal signal abnormalities in addition to tentorial. The centreline structures are in place.

Figure 1: Axial(a), sagittal (b) and coronal (c) ; TDM sans injection, montrant processus lésionnel circonscrit centré sur bulbe rachidien à double composant tissulaire et kystique, avec discret refoule de 4 eme ventricule sans signe de hydrocéphalie.
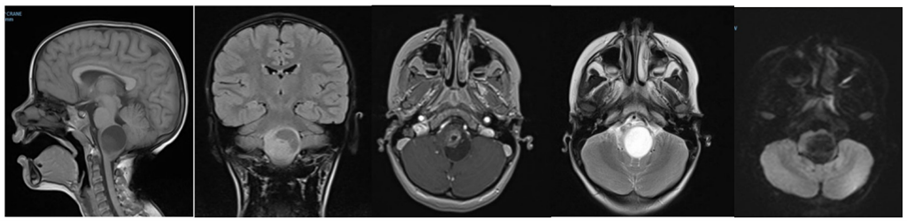
Figure 2: Sagittal section (a) lesion centered on the bulb with dual tissue.
References
- Alice Métais, andrey Rousseau. Histomolecular diagnosis of glial and glioneuronal tumors, department of pathology, 2021; 12: 137-153. doi: 10.1016/j.annpat.2020.12.008
- levin Hani. Astrocytome pilocytique- Philippe Schucht.
- Yong Jiang, Liang Lv, Senlin Yin, Peizhi Zhou, Shu Jiang. Primary spinal pilocytic astrocytoma: clinical study with long-term fallow-up in 16 patients and a literature review, Neurosurg Rev, 2020; 43(2): 719-727. doi: 10.1007/s10143-019-01109-0.
- Astrocytoma tumors are primary central nervous system and are mainly located in cerebellum.

