Scrub Typhus: A Great Mimic of Severe Dengue
Zhong Xhen Khor*, Dr. Valliappan Muthuraman and Dr. Vishnu Prashad A/L (Bhakthaval Salan)
Department of Medicine, Hospital Segamat, Johor, Malaysia
Received Date: 09/03/2024; Published Date: 24/07/2024
*Corresponding author: Zhong Xhen Khor, MBBS, MRCPI, Department of Medicine, Hospital Segamat, Johor, Malaysia
Abstract
A gentleman in his 60s presented to our center with fever, chills, loose stools and lethargy for 1 week. He was intubated on arrival for respiratory distress. Initial physical examination was unremarkable. Bloods on admission revealed bicytopenia and acute kidney injury. He was initially treated as severe dengue due to positive dengue IgM on point of care testing. IV Meropenem was started to cover for superimposed bacterial infection. The following day (day 8 of illness), he had persistent spiking temperature. A blanchable generalized maculopapular rash was noted, which was atypical for dengue. He was then started on oral Doxycycline to cover for atypical infection. His temperature settled within 24 hours and he was extubated on day 3 of admission; His general condition & laboratory results improved gradually throughout admission. Retrospectively, his blood cultures and dengue PCR were negative but rickettsial serology returned positive for Orientia Tsusugamushi (> 1:800), suggestive of active scrub typhus infection.
Keywords: Typhus; Tropics; Infection; Fever; Rash
Introduction
Dengue is often considered to be a prevalent illness in the South East Asia setting. Scrub Typhus is a close mimic but index of suspicion is relatively low [1]. To complicate matters, both illnesses present with non specific symptoms such as fever, myalgia, arthralgia, vomiting, diarrhea & headache, coupled with similar biochemical abnormalities such as leucopenia, thrombocytopenia, and transaminitis [2]. Severe illness in both may manifest as septic shock, acute kidney injury, disseminated intravascular coagulation [1]. As dengue is typically managed conservatively; potential consequences may arise in the delayed diagnosis in scrub typhus, an infection that necessitates antibiotics. An elderly gentleman presented to our setting with an acute febrile illness and exanthem; he was initially diagnosed with dengue, but eventually proved to be scrub typhus.
Case Summary
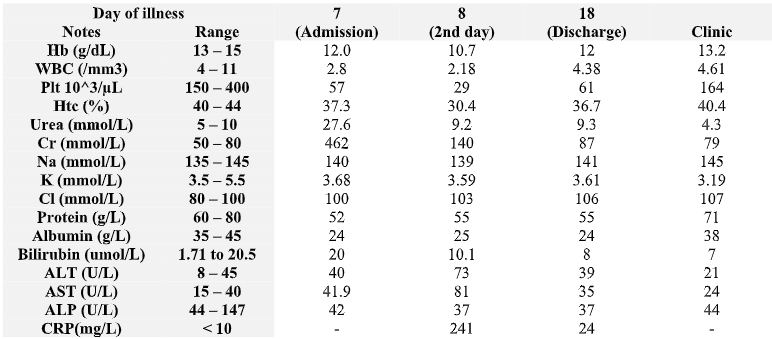
A man in his 60s with no known medical illness presented with fever, chills, loose stools, arthralgia, myalgia and lethargy for 1 week prior to admission. He also complained of a dry cough and shortness of breath, which progressively worsened, prompting medical attention. No ill contacts or travel history was noted. He works in his durian orchard with frequent exposure to insects & mosquitoes. He is unable to recall any tick bites. Upon arrival, he was noted to be febrile, drowsy and in respiratory distress. He was tachycardic with a heart rate of 120 beats per minute, blood pressure of 138/65 mmHg and oxygen saturation was noted to be 90% under room air. He was also febrile to touch (temperature 39 – 40 degrees Celsius). Fearing further respiratory compromise, he was intubated. Systemic examination was otherwise unremarkable for any lymphadenopathy or hepatosplenomegaly. No rash or eschar was initially noted. Auscultation revealed clear lungs and no murmurs were heard. Full blood count was significant for leucopenia & thrombocytopenia (Table 1). Dengue Rapid Test Kit revealed positive IgM but negative dengue NS1 antigen & IgG. He was thus treated as severe Dengue and admitted to ICU for close observation. Suspecting also secondary bacterial infection, he was started on IV Meropenem and blood cultures, C - reactive protein (CRP) taken CXR is otherwise clear.

Figure 1: General maculopapular rash seen on patient’s trunk.
On day 2 of admission, a generalized blanchable maculopapular rash was noted throughout the trunk (Figure 1). This was unusual for dengue as despite day 7 of illness, he was still acutely febrile (39 - 40 degrees Celsius). Suspecting secondary atypical infection, blood film for Malaria Parasite (BFMP), Leptospira IgM, HIV, Hepatitis B, Hepatitis C serology & Rickettsia serology were sent. Oral Doxycycline was then added. As per local protocols, confirmatory dengue PCR was sent to identify dengue subtype. Dengue serology is not repeated as suspicion now turned to atypical infections. He subsequently responded to the doxycycline and his temperature promptly settled by day 3 of admission (day 10 of illness), with improving CRP, leucopenia and thrombocytopenia (Table 1). No pathogens were isolated on Blood Cultures. He was eventually extubated and discharged after 1 week of hospitalization. Outpatient review a month later revealed negative dengue PCR but a positive Rickettsia serology (Orientia tsutsugamushi IgG > 1: 800).
Table 1: Blood investigations trend of patient from admission till discharge and outpatient visit.
Discussion
Scrub Typhus is often not considered as a differential of acute febrile illness. Historically, this is attributed to a lack of interest in rickettsial diseases after the discovery of Chloramphenicol in 1940, despite extensive research during World War 2. The non-specific presentation of rickettsial infections, coupled with difficulty in lab diagnosis are among cited factors that discourage clinicians from considering scrub typhus as a differential [3]. Moreover, acute dengue fever is given more prominence and often associated with a deep public stigma in endemic areas, further dissuading considerations of Scrub Typhus [4].
The consequences of a missed diagnosis are significant as 20% of rickettsial patients may present with a qSOFA score > 2, with a corresponding 10% mortality rate. As a result, scrub typhus is now considered a neglected tropical disease that is gradually making a comeback [3]. A local paper has since described its prevalence 8% when studied in the context of acute febrile illness, with increased incidence during rainy seasons [2].
In clinical practice, apt suspicion is important as serological confirmation is time consuming: a raised IgG level on immunofluorescent assay takes 2 weeks, which is not practical when dealing with acutely ill patients in whom diagnosis is suspected [5]. PCR is a useful tool for diagnosis, allowing for early and sensitive detection of bacteremia before antibody responses become detectable [2]. However, in resource limited setting such as ours, cost of transportation of samples to a tertiary center with PCR facilities posits an issue and, in many places, PCR testing might be available at all. Eschar, while traditionally attributed to scrub typhus, is absent in areas with high typhus endemicity due to acquired immunity from previous exposure [1]. Besides complicating the diagnostic process, its absence signifies a lack of biopsy samples for molecular diagnostics for scrub typhus, which often results if 100% specificity [6]. A therapeutic trial with Doxycycline PO with resolution of fever within 48 hours is expected. A failure to respond should prompt clinicians to consider other forms of tick infections, treatment resistance or other diagnosis. Alternatives for pregnant ladies or children include PO Azithromycin or Rifampicin [1].
To differentiate between dengue & scrub typhus, the Clinical Score to Differentiate Scrub Typhus and Dengue (CSSD score) may be utilized. This simple scoring system incorporates mental status, pulse oximetry, hemoglobin level, white cell count, SGOT (Alanine transferase) and serum bilirubin level. Our patient's CSSD score is 16, favoring dengue. This combined with a positive Dengue IgM, most certainly alludes to the diagnosis. However, the timing of rash, as well as respiratory complains generally points against this [4].
In dengue, fever is typically resolved as the patient enters the critical phase, most commonly around the 5th day of illness. The classical rash, typically described as ‘isles of white in a sea of red’ does not blanch with pressure [3]. Patients with typhus, regardless of severity, typically present with a blanchable maculopapular rash that coincides with the presence of fever, originating at the trunk (Image 1), that spreads to the axilla, sparing the face, palms, and soles [1]. Furthermore, respiratory complaints are a noteworthy manifestation that is more specific to scrub typhus. Cough is present in 40% of patients, in contrast with Dengue (19%). Interstitial pneumonitis and acute respiratory distress syndrome (ARDS) are manifestation more inclined towards scrub typhus [2]. These clinical features were seen in our patient. As such, CSSD scoring, while helpful needs to be interpreted with regards to the patient’s overall presentation. Additionally, the role of Dengue IgM has recently been called into question as it is known to persist for at least 60 days and caution must be utilized in interpretation [8].
Conclusion
Scrub Typhus is an important consideration in the differential of acute febrile illness in the tropical setting. Although presentation of scrub typhus & dengue are similar, the presence of a maculopapular rash in the setting of fever, should raise suspicion of Scrub Typhus, particularly if associated with significant respiratory symptoms. A therapeutic trial of Doxycycline for Scrub Typhus may be recommended as serological or PCR confirmation might be time and resource consuming and not feasible in acute presentations. CSSD score, while a helpful tool in differentiating scrub typhus and dengue fever, it has to be used with caution as illustrated in our case.
Declarations
Authorship statement: ZX Khor was involved in the conception, design, and drafting of the article, as well as proofreading and gave final approval. V Muthuraman, Vishnu Prasad was involved in proofreading and gave final approval.
Ethical Approval: Not Applicable
Funding Statement: This paper is not funded by any organization
Availability of data and materials: Not Applicable
Conflict of Interest: This study has no conflict of interest
Acknowledgements: The authors would like to thank the patient’s daughter for her permission to publish this paper
References
- Singh OB, Panda PK. Scrub Typhus. StatPearls Publishing; 2022.
- Yuhana MY, Hanboonkunupakarn B, Tanganuchitcharnchai A, Sujariyakul P, Sonthayanon P, Chotivanich K, et al. Rickettsial infections are neglected causes of acute febrile illness in Teluk Intan, Peninsular Malaysia. Trop Med Infect Dis, 2022; 7(5): 77.
- Bonell A, Lubell Y, Newton PN, Crump JA, Paris DH. Estimating the burden of scrub typhus: A systematic review. PLoS Neglected Tropical Diseases, 2017; 11(9): e0005838.
- Abhilash KP, Mitra S, Gautam I, Jambugulam M, Jayaseeelan V. Clinical score to differentiate scrub typhus and dengue: A tool to differentiate scrub typhus and dengue. J Glob Infect Dis, 2017; 9(1): 12.
- Stewart AG, Stewart AGA. An Update on the Laboratory Diagnosis of Rickettsia spp. Infection. Pathogens, 2021; 10(10): 1319.
- Rungrojn A, Batty EM, Perrone C, Abdad MY, Wangrangsimakul T, Brummaier T, et al. Molecular diagnosis and genotyping of Orientia tsutsugamushi in Maesot and Chiangrai, Thailand. Frontiers in Tropical Diseases, 2023; 4.
- Ministry of Health Malaysia; Academy of Medicine Malaysia. Clinical practice guidelines: management of dengue infection in adults revised 2nd ed. Putrajaya: Ministry of Health Malaysia, 2010.
- Chien YW, Liu ZH, Tseng FC, Ho TC, Guo HR, Ko NY, et al. Prolonged persistence of IgM against dengue virus detected by commonly used commercial assays. BMC Infectious Diseases, 2018; 18(1).

