Brugada Type 2 ECG with Syncope the Importance of Pattern Recognition and Serial ECG
Zhong Xhen Khor* and Pairan, Shakirin
Department of Medicine, Hospital Segamat, Johor, Malaysia
Received Date: 09/03/2024; Published Date: 23/07/2024
*Corresponding author: Zhong Xhen Khor, MBBS, MRCPI, Department of Medicine, Hospital Segamat, Johor, Malaysia
Abstract
Brugada Syndrome is a recognized condition that may cause sudden cardiac death. This diagnosis can occasionally be missed due to the transient nature of the typical Electrocardiogram (ECG). Clinicians might be familiar with type 1 brugada pattern, but not type 2 brugada ECG. A 58-year-old lady presented to our center after a fall. She experienced a sudden loss of consciousness while she was cooking. This episode was described as a sudden blackout. She regained consciousness almost immediately. Upon arrival, physical examination was unremarkable, except for soft tissue injury over the lower lip. ECG was performed in the emergency department and was read as normal (but was Brugada type 2). Serial ECGs throughout admission were significant for Brugada Type 1 and 2 patterns. This realization of the Brugada type 1 pattern prompted further history, which revealed a sudden cardiac death in her otherwise healthy 20 years old son, who passed away unexpectedly in his sleep. Her echocardiography and blood investigations were otherwise unremarkable. Fulfilling both ECG and clinical criteria for Brugada Syndrome, she was subsequently referred to cardiology for further evaluation. An ICD was eventually implanted.
Keywords: Death; Sudden; Cardiac; ICD; Arrhythmia; ECG; Brugada
Introduction
Brugada Syndrome is a rare entity that can cause sudden cardiac death via spontaneous ventricular tachyarrhythmias [1]. It is typically under diagnosed or unrecognized in day-to-day clinical practice due to a lack of familiarity. The dynamic, transient nature of the ECG changes might also be unrevealing [2]. Brugada Type 1 pattern (classically described as a shark fin ST elevation over the right precordial leads) is well known, but little is often reported about Brugada Type 2 ECG.
Case Summary
A lady in her 50s with no known medical illness presented to our setting post-fall. This occurred suddenly while she was cooking and was described as a sudden blackout. She regained composure within a few seconds without any recollection of events. No tonic-clonic movements or prodromal cardiovascular symptoms were experienced. Upon arrival, she was well. Physical examination revealed only a soft tissue injury over her lip while vital signs and cardiovascular and neurological examination findings were normal. A non-contrasted CT Brain did not reveal any evidence of stroke. ECG on admission (Figure 1) was read as normal.
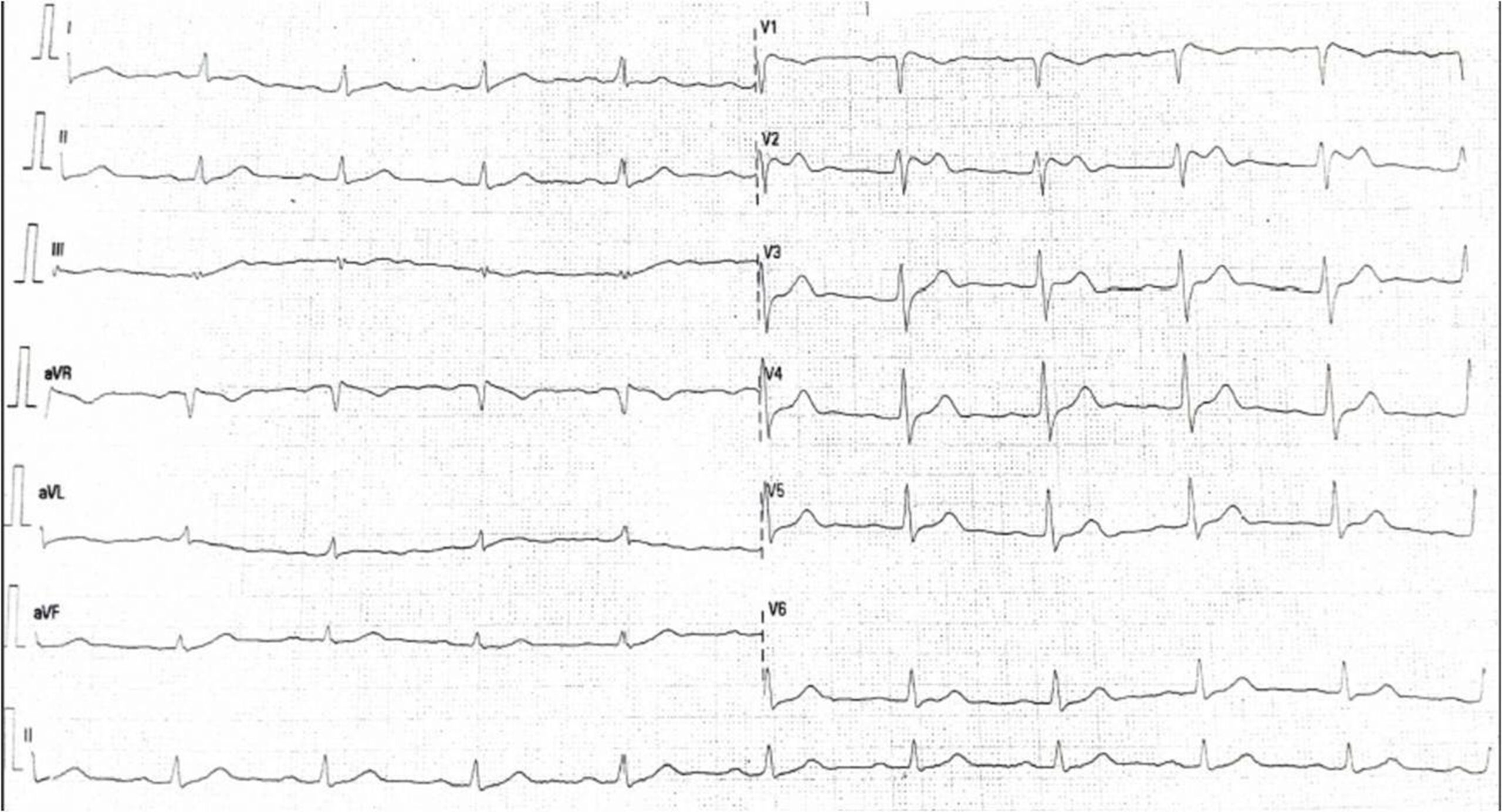
Figure 1: ECG on day 1 of admission (Saddle ST elevation indicative of Brugada Type 2 pattern was noted but read as normal sinus rhythm).
ECG on the day 2 of admission (Figure 2) however, captured coved-shaped ST elevation which was typical of Brugada Type 1 (shark fin appearance).
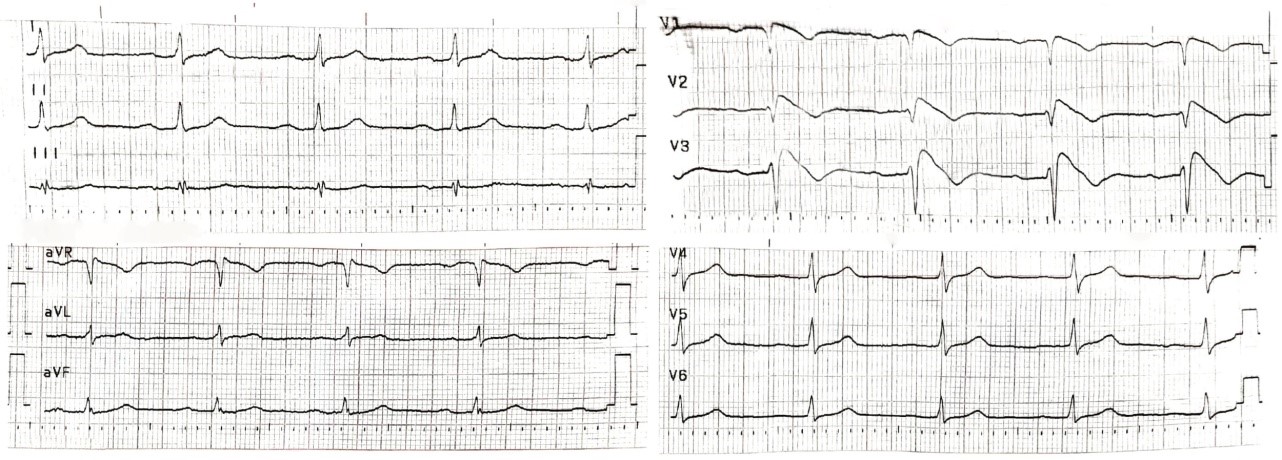
Figure 2: ECG on day 2 of admission (Coved Shaped ST elevation noted over the V1-V3; typical for Brugada Type 1 Pattern).
Suspecting Brugada Syndrome, further history was sought and a positive sudden cardiac death in her family was noted: her young son, otherwise fit and well in his 20s, a naval officer, passed away unexpectedly in his sleep. No foul play was suspected, nor was he known to abuse any substances. A revision of her ECG on admission (Figure 1) was realized to be a Brugada Type 2 pattern, which was not recognized. Serial ECGs revealed a persistent Brugada Type 2 pattern while echocardiography demonstrated good left ventricular ejection fraction without any wall motion abnormalities. She was briefed regarding the diagnosis and its implications and was referred to the National Heart Centre for further evaluation. A transvenous ICD was eventually implanted (Figure 3).
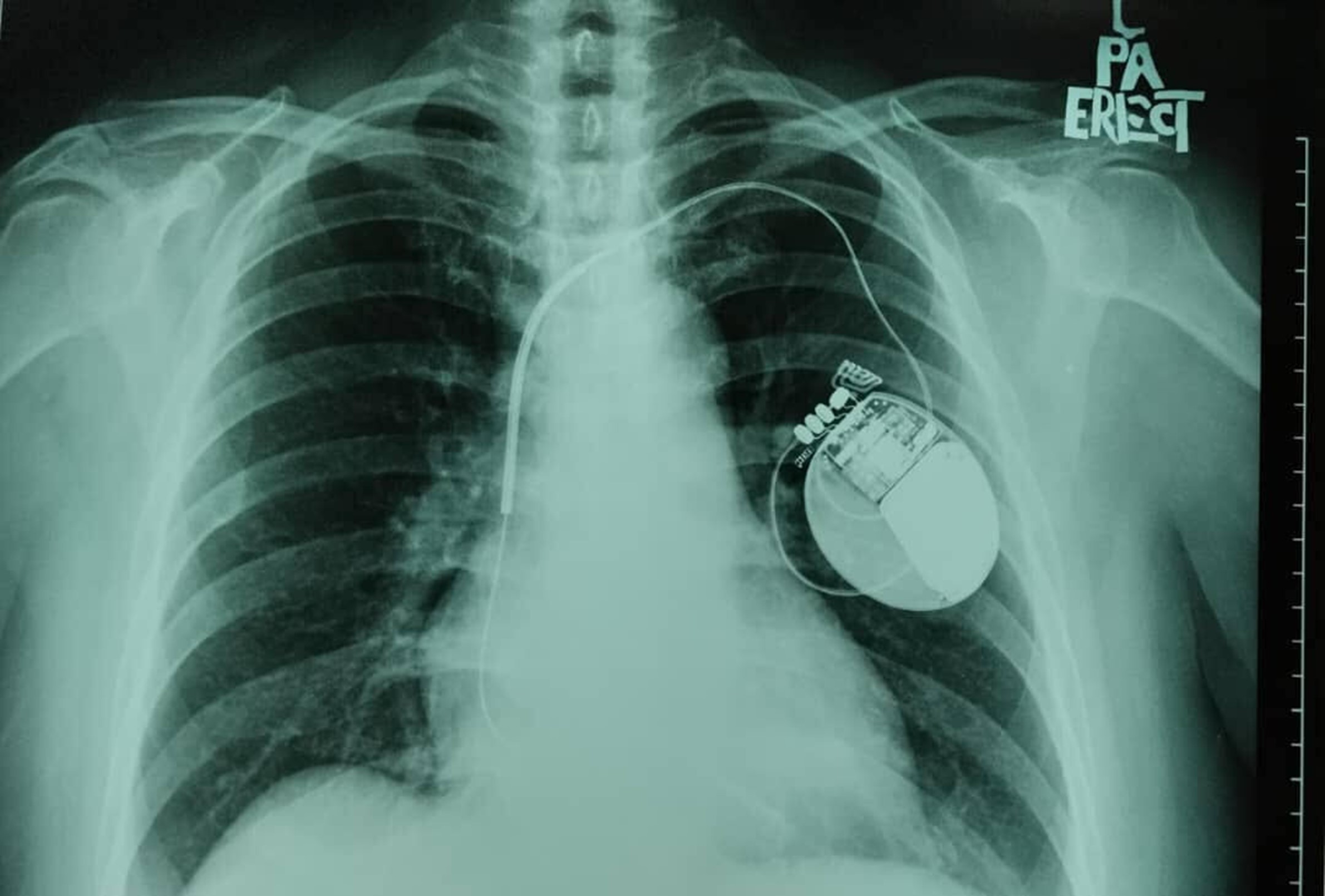
Figure 3: Post transvenous ICD insertion.
Discussion
Recognition of Brugada type 2 ECG is important as it can be the initial manifestation found in post-Cardiac Arrest / VF [3,4] or Syncope [2]. It can also be an incidental finding [5]. When Type 2 Brugada pattern ECG is present, challenge with sodium channel blockers is recommended to elicit Type 1 pattern (the eponymous criteria required for diagnosis). This was unnecessary in our patient as her ECG converted spontaneously.
Contrary to other inherited arrhythmia syndromes, such as Hypertrophic Cardiomyopathy or Catecholaminergic Polymorphic Ventricular Tachycardia which are often accentuated by exertion or catecholamines; Brugada-induced ventricular tachyarrhythmia is often provoked by an increase in vagal activity (sleep, bradycardia) or fever, that enhance the J-point. When present in young Asian males, Type 1 ECG is more malignant. Given the unexpected circumstances and the ECG seen in our patient, it is likely our patient’s son has Brugada Syndrome and succumbed during his sleep [1].
Our consultant opted for ICD implantation as our patient has a spontaneous type 1 Brugada ECG, a positive family history of sudden cardiac death, and a presentation of syncope that is likely arrhythmic (occurring unexpectedly, resolving fairly quickly, without any prodromal symptoms and triggers). They believe she exhibits a high-risk phenotype with likely future recurrence as the frequency of cardiac arrest in Brugada Syndrome is reported to increase with age [6]. Furthermore, during evaluation, she was found to have multiple episodes of bradycardia, a risk factor for ventricular tachyarrhythmias in patients with Brugada type ECG. In a patient with conventional presentation and risk factors, watchful waiting for absolute indications of ICD such as a witnessed cardiac arrest or ventricular tachyarrhythmia might be harmful [1]. Furthermore, the patient has previously experienced the loss of a loved one and is accepting of procedural risks.
Regardless of ICD, patients with Brugada-type ECG should be followed up to monitor for clinical manifestation of ventricular tachyarrhythmia as well as co-existence of other arrhythmias, such as Atrial Fibrillation, which will increase the risk for further lethal arrhythmic events. Patients should also be wary of alcohol and various drugs, as some may precipitate tachyarrhythmia. Fever also should be treated aggressively [1]. We did not recommend any genetic studies to our patient or her family as it is expensive. Moreover, the gene implicated (SCN5A) is only found in 10 % of patients, with poor genotype-phenotype mismatches and would not otherwise influence clinical management [7].
Conclusion
Brugada Syndrome is an important consideration whenever patients present with falls or syncope. History taking is paramount as it may uncover the clinical events behind syncope as well as a family history of sudden cardiac death. Clinicians should bear in mind and recognize type 2 Brugada Pattern on ECG, as it may be the initial presenting ECG of Brugada Syndrome. When present, serial ECG might uncover an underlying Typical 1 Brugada Pattern (the eponymous criteria for diagnosis).
Declarations
Authorship statement: ZX Khor was involved in the conception, design, and drafting of the article, as well as proofreading and gave final approval. P Shakirin was involved in proofreading and gave final approval.
Ethical Approval: Not Applicable
Funding Statement: This paper is not funded by any organization
Availability of data and materials: Not Applicable
Conflict of Interest: This study has no conflict of interest.
Acknowledgements: The authors would like to thank the patient for her permission to publish this paper.
References
- Priori SG, Wilde AA, Horie M, Cho Y, Behr ER, Berul C, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm, 2013; 10(12): 1932–1963.
- Yuasa H, Kitaura A, Kitayama C, Fuyuta M, Mino T, Okamoto K, et al. A 32-year-old man diagnosed with type II Brugada syndrome on preoperative electrocardiogram 1 week before elective tympanoplasty. Am J Case Rep, 2021; 22: e927756.
- Fuyuta M, Nakao S, Takai N, et al. Sudden cardiac arrest during general anesthesia in an undiagnosed Brugada patient. J Cardiothorac Vasc Anesth, 2013; 27: 1334-1336.
- Sattar Y, Ullah W, Zaidi SR, Almas T, Alraies MC. Brugada pattern type 2 diagnosis unmasked by aspiration pneumonia. Cureus, 2020; 12(5): e8331.
- Blotner M, Betageri O, Miles W, Xiang K. Workup for suspected Brugada syndrome: Two case reports for the general practitioner. Cureus, 2022; 14(2): e21921.
- Olde Nordkamp LR, Vink AS, Wilde AA, de Lange FJ, de Jong JS, Wieling W, et al. Syncope in Brugada syndrome: prevalence, clinical significance, and clues from history taking to distinguish arrhythmic from nonarrhythmic causes. Heart Rhythm, 2015; 12(2): 367-375. doi: 10.1016/j.hrthm.2014.10.014.
- Batchvarov VN. The Brugada Syndrome - Diagnosis, Clinical Implications and Risk Stratification. Eur Cardiol, 2014; 9(2): 82-87. doi: 10.15420/ecr.2014.9.2.82.

