A Rare Case of Papillary Fibroelastoma of the Aortic Valve Causing both an Embolic Ischemic Stroke and a Retinal Artery Branch Occlusion
Houda Brarou1,*, Manal Bouggar1, Soukaina Laaouina1, Taoufik Abdellaoui2, Soundouss Sebbata1, Samah Sadiki1, Nermine Belayachi3, Mohamed Boukssim1, Aissam Fiqhi1, Yassine Mouzari1 and Abdelbare Oubaaz1
1Ophtalmology department, Military hospital Mohammed-V, Mohammed V University -Rabat, Morocco
2Cardiology department, Military hospital Mohammed-V, Mohammed V University -Rabat, Morocco
3Sidi Mohamed ben Abdellah University, Fes, Morocco
Received Date: 01/03/2024; Published Date: 10/07/2024
*Corresponding author: Houda Brarou, Ophtalmology department, Military hospital Mohammed-V, Mohammed V University -Rabat, Morocco
Abstract
Purpose: We present a novel case of a papillary fibroelastoma causing a brain stroke and a branch retinal arterial occlusion in a young male patient.
Methods: A 37-year-old man who presentend with a stroke in the right frontal lobe followed the next day by a partial painless loss of vision in his left eye. Visual acuity in the LE was 20/70. Diagnosis required transesophageal echocardiography to localize the lesion.
Results: Aortic valve papillary fibroelastoma was successfully treated with tumor resection.
Conclusion: Although fibroelastoma is a histologically benign tumor, its evolution can be marked by severe complications such as rerinal artery occlusion, systemic embolisms as it is the case with our patient, and sudden death.
Keywords: Retinal artery occlusion; Stroke; Papillary fibroelastoma; Tumor
Introduction
Papillary fibroelastomas (PFEs) are the second most common primary cardiac tumors after myxomas [1-3]. PFEs are benign but highly friable in nature. Their prompt detection is of great importance as they are the potential causes of systemic emboli, stroke, myocardial infarction, and sudden death. We present a novel case of a PFE causing a brain stroke and a branch retinal arterial occlusion, reminding us of the importance of keeping this as an important differential diagnosis when determining the cause of the embolic incident.
Case Report
The patient was a 37-year-old male with no past medical nor ocular history. He denied smoking, alcohol intake, or illicit-drug use. He presented to the emergency department with sudden onset aphasia and left hemiparesis.
Magnetic resonance imaging of brain showed multiple small areas of High signal on T2/FLAIR in the right frontal lobe. The patient was immediately started on systemic anticoagulation.
As part of the workup to determine the cause of his embolic stroke, the patient was sent for a Transesophageal Echocardiogram (TEE). The TEE showed no evidence of thrombus in the left atrial appendage. Also, the bubble study did not show any evidence of atrial septal defect or patent foramen ovale. However, an 8mm echogenic and highly mobile mass on the posterior cusp of the tricuspid aortic valve was seen, suggestive of a fibroelastoma (Figures 1).
There was no cardiac dysfunction. Blood tests were normal. Serial ECG and ECG Holter showed sinus rhythm.
On the second hospital day, the patient presented with a partial painless loss of vision in his left eye on awakening. The loss was sudden in onset. One hour after the initial event, he regained the upper half of his vision.
Ophthalmologic examination showed Visual acuity of R.E.: 20/20 and L.E.: 20/70. The intraocular pressure was 15 mm Hg in each eye. An afferent pupillary defect was observed in the left eye. The anterior chamber was deep and quiet in both eyes. Furthermore, there was no neovascularization of the iris in both eyes, and the lenses were clear in both eyes. On fundus examination, the right eye showed a normal retina with a dry macula and a healthy disk. In the left eye, there was focal area of retinal whitening superior to the optic nerve, superior to the fovea along the distribution of the superotemporal branch retinal artery indicating edema. There was no evidence of disc swelling or haemorrhages. Optical Coherence Tomography (OCT) was performed and showed thickening of the outer part of the superior hemiretina with a shadowing effect, indicating edema (Figure 2).
Additionally, OCT-angiography revealed a lack of capillary blood flow in the affected area (Figure 3) and a normal study in the other eye.
A multidisciplinary team decided on surgical treatment of the intracardiac masses by scheduled surgical excision 2 weeks after the ischemic stroke. Simple excision of the tumor was performed.with no need for valve replacement.. No major surgical complications were reported. Pathologic examination of the surgically removed pieces confirmed the diagnosis of PFE (Figure 4).

Figure 1 : A papillary fibroelastoma measuring 8 mm attached the posterior cusp of the tricuspid aortic valve, as seen by TEE in the midesophageal short-axis.

Figure 2 :
A: Color fundus photo of the left eye with superior branch retinal artery occlusion. Retinal whitening surrounding the occluded artery is noted.
B: Red-free photograph of the left eye with superior branch retinal artery occlusion. The red-free photograph greatly accentuates the retinal whitening surrounding the occluded artery.
C: Optical coherence tomography (OCT) of the left eye with superior branch retinal artery occlusion. Cross-section goes through superior retina to inferior retina, capturing the abnormally thickened retina associated with intracellular edema.
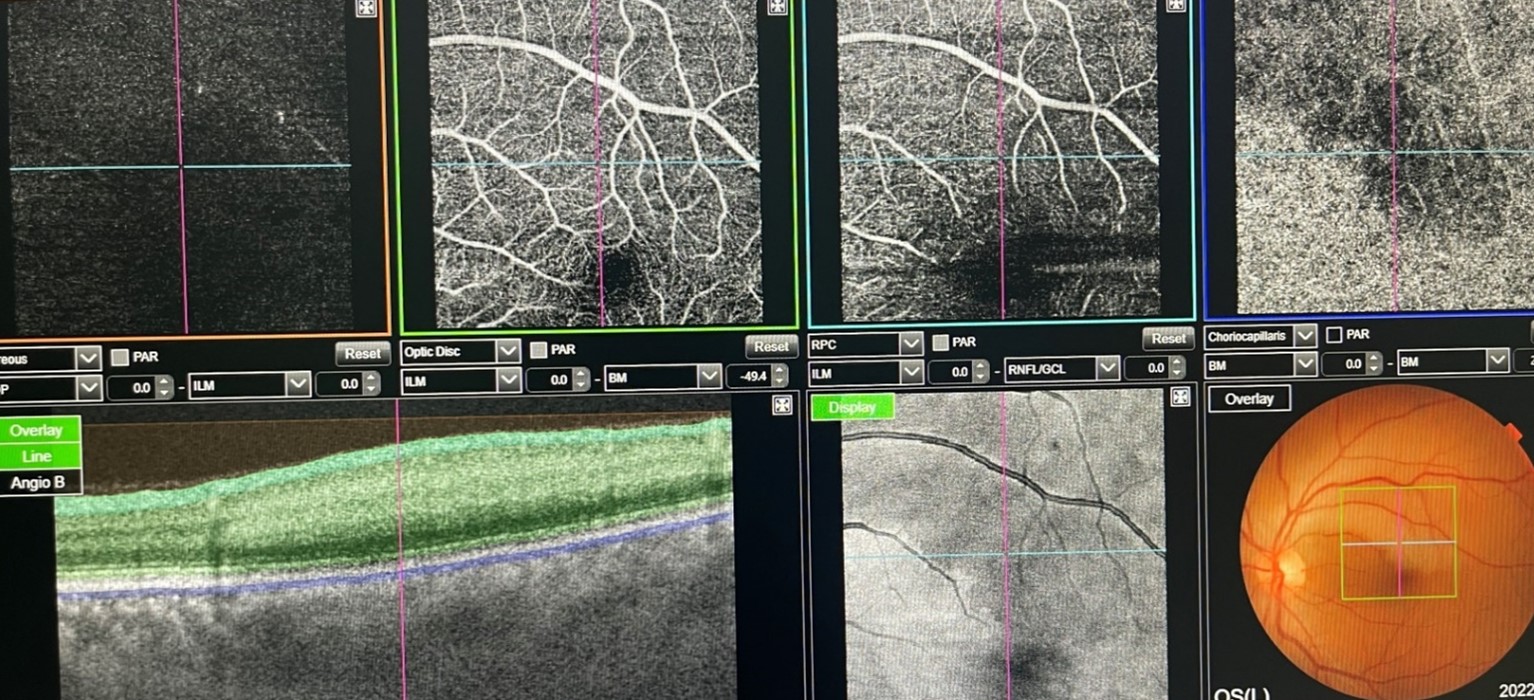
Figure 3 : OCT-angiography of the left eye revealing a lack of capillary blood flow in the affected area.
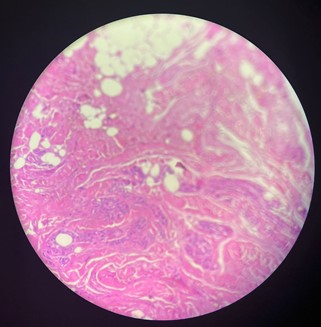
Figure 4: Papillary hyalinized hypocellular stroma with endocardial lining.
Discussion
The frequency of primary cardiac tumors is very low (0.02%) [4,5]; Hence, a primary cardiac tumor embolization is a very rare entity. Cardiac PFE are the second most common primary cardiac tumors (10%) [4,6] after myxomas [4,5,7].
The majority of patients with CPF are asymptomatic, however, CPF may present with cerebrovascular events, angina, myocardial infarction, sudden cardiac death, heart failure, syncope, pulmonary embolism, peripheral embolism, or vision loss as in our case [5,7].
Echocardiogram usually demonstrates a small (≤1 cm) mobile mass arising from the mitral valve (less frequently from the aortic or tricuspid valve or auricular or ventricular surface), with a frayed pattern near the edges, correlated with the papillary projections of the tumor [3,4]. Pathologic examination of the surgical piece confirms the diagnosis [4], as it did in our case. The definitive and curative treatment for symptomatic PFE is surgical excision of the tumor, performed as soon as possible to diminish the risk of early recurrences [3-8]. Prognosis after surgical removal is excellent [3].
In reality, an embolic cerebral stroke in a young patient with no evidence of cerebrovascular disease, particularly in the presence of sinus rhythm, should prompt investigation into the presence of a cardiac tumor along with infective endocarditis and mitral valve prolapse [11].
Retinal artery occlusion is an indication that the patient is at risk of vascular occlusion elsewhere in the body and therefore requires prompt investigation.
Declaration: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding: The authors received no specific funding for this work.
References
- Grinda JM, Couetil JP, Chauvaud S, D’Attellis N, Berrebi A, Fabiani JN, et al. Cardiac valve papillary fibroelastoma: surgical excision for revealed or potential embolization. J Thorac Cardiovasc Surg, 1999; 117: 106-110.
- Law KB, Phillips KRB, Cusimano RJ, Butany J. Multifocal “tapete” papillary fibroelastoma. J Clin Pathol, 2009; 62: 1066-1070.
- Bicer M, Cikirikcioglu M, Pektok E, Muller H, Dettwiler S, Kalangos A. Papillary fibroelastoma of the left atrial wall: a case report. Journal of Cardiothoracic Surgery, 2009; 4: 28.
- Capotosto L, Elena G, Massoni F, et al. Cardiac tumors: echocardiographic diagnosis and forensic correlations. Am J Forensic Med Pathol, 2016; 37: 306–316.
- Gowda RM, Khan IA, Nair CK, Mehta NJ, Vasavada BC, Sacchi TJ. Cardiac papillary fibroelastoma: a comprehensive analysis of 725 cases. Am Heart J,2003; 146: 404–410.
- Sastre-Garriga J, Molina C, Montaner J, et al. Mitral papillary fibroelastoma as a cause of cardiogenic embolic stroke: report of two cases and review of the literature. Eur J Neurol,2000; 7: 449–453.
- Yandrapalli S, Mehta B, Mondal P, et al. Cardiac papillary fibroelastoma: the need for a timely diagnosis. World J Clin Cases,2017; 5: 9–13.
- Roeltgen D, Kidwell CS. Neurologic complications of cardiac tumors. Handb Clin Neurol,2014; 119: 209–222.
- Gowda RM, Khan IA, Nair CK, et al. Cardiac papillary fibroelastoma: A comprehensive analysis of 725 cases. Am Heart J, 2003; 146: 404–410.
- Zamora RL, Adelberg DA, Berger AS, et al: Branch retinal artery occlusion caused by a mitral valve papillary fibroelastoma. Am J Ophthalmol, 1995; 119: 325–329.
- Lopez-Sanchez E, Munoz EF, Martinez JAA, et al: Central retinal artery occlusion as the initial sign of aortic valve papillary fibroelastoma. Am J Ophthalmol, 2001; 131: 667–669.

