Isolated Sigmoid Colon Perforation Secondary to Blunt Abdominal Trauma
Shariful Islam1,2,*, Aneela Shah1, Avidesh Mahabir1,2, Vijay Naraynsingh2,3 and Patrick Harnarayan1,2
1Department of General Surgery, Breast Unit, San Fernando General Hospital, San Fernando, Trinidad & Tobago
2Department of Clinical Surgical Sciences, University of the West Indies, St. Augustine, Trinidad & Tobago
3Medical Associates Hospital, St. Joseph, Trinidad & Tobago
Received Date: 28/02/2024; Published Date: 01/04/2024
*Corresponding author: Shariful Islam, MBBS, DM, FACS, FASBrS, FCCS, Specialist Breast Surgeon, Breast Clinic, San Fernando General Hospital, Trinidad & Tobago; Associate Lecturer, Department of Clinical Surgical Sciences, University of the West Indies, St. Augustine, Trinidad & Tobago
Abstract
Seat-belt syndrome describes the presence of a seat-belt sign in addition to vertebral fractures and intra-abdominal visceral injury during motor vehicular accidents. However, isolated sigmoid colon injury as part of this phenomenon is rare and it can be challenging to detect such injuries in a timely manner due to a paucity of definitive diagnostic modalities. We present a 20-year-old male patient who presented with a seatbelt sign being involved in a motor vehicular collision. He was initially considered haemodynamically stable with lower abdominal pain and non-specific radiological signs. He eventually required emergency laparotomy when he developed peritonitis and was found to have an isolated injury to the sigmoid colon. This case report seeks to highlight the incidence of isolated colonic injuries in blunt abdominal trauma and the high level of clinical suspicion required to avoid missed injuries and catastrophic complications.
Keywords: Blunt trauma; Delayed colonic perforation; Isolated sigmoid colonic perforation; Seatbelt sign
Introduction
The three-point seatbelt, introduced in the 1970s, has helped to decreased fatalities from road traffic accidents by up to 60 %. However, the use of these protective restraints has been associated with a specific pattern of vertebral and intra-abdominal injuries in high energy impact collisions [1], known as seatbelt syndrome.
In this syndrome, the incidence of blunt abdominal trauma is approximately 12%, with most injuries involving solid viscera like the spleen or liver, then parts of the intestine that are fixed in the abdomen [2]. A patient with intestinal injury presenting with peritonitis or radiological findings identifying hard signs of such, urgent surgical intervention is warranted. However, intestinal injuries may not always declare themselves early in a patient’s admission. As a result, patients with a seatbelt sign should be monitored closely with a high index of suspicion for underlying intestinal trauma.
Isolated sigmoid colon injuries in blunt trauma are rarely reported and are thought to be a result of its relatively safe location in the pelvis. This low incidence of sigmoid colon injury in blunt trauma and the lack of definitive signs in some cases can cause delays in diagnosis and treatment, contributing to significant morbidity and mortality rates [3].
Case
A twenty-year old male presented to the Accident and Emergency Department, having been involved in a motor vehicular accident on the previous night. He was the restrained front seat passenger in a head-on collision with another vehicle and presented with left sided chest and abdominal pain.
The patient reported no loss of consciousness or other acute symptoms. He had no comorbidities or allergies, was a non-smoker and consumed alcohol occasionally.
At arrival to the Emergency room, the patient was alert and oriented, with a GCS of 15/15. He had no signs of external injury apart from a seatbelt sign, with bruising mostly over the left chest and left lower quadrant (Figure 1). His vital signs were within normal limits, apart from a mild tachycardia of 102 beats per minute. Examination revealed tenderness over the left chest wall and left lower quadrant, with guarding but no signs of peritonitis.
Laboratory investigations were within normal limits, with hemoglobin of 16g/dL and a white blood cell count of 9 x109 /L. Erect chest x-ray revealed no abnormalities (Figure 2). Contrast-enhanced computed tomography (CT) of the abdomen demonstrated a small amount of hyper dense fluid in the pelvis and left paracolic gutter, likely blood. There was no extra-luminal free air or signs of contrast extravasation to suggest active bleeding (Figure 3).
The patient was admitted for observation, serial abdominal examinations and serial hemoglobin checks. The patient remained haemodynamically stable, with no significant change in abdominal examination. Approximately forty hours post-incident, the patient’s pulse rose to 120 beats per minute. He looked unwell and was peritonitic on abdominal examination. His hemoglobin level remained unchanged since admission and a decision was made for emergency laparotomy with a high suspicion for intra-abdominal visceral injury.
At laparotomy, 400ml of blood was evacuated from the abdomen and a grade three sigmoid colon injury was identified, with feculent peritonitis (Figure 4). Due to the patient’s hemodynamic status and the need for intraoperative inotropic support, a Hartmann’s procedure was performed and the patient was taken to the Intensive Care Unit (ICU) for postoperative recovery. Inotropic support was weaned off by day two post-surgery and he was transferred to the surgical ward where he had an uneventful recovery and was discharged a week later. Reversal of his colostomy is planned for six weeks post-surgery.

Figure 1: image showing seatbelt sign (taken post-surgery).
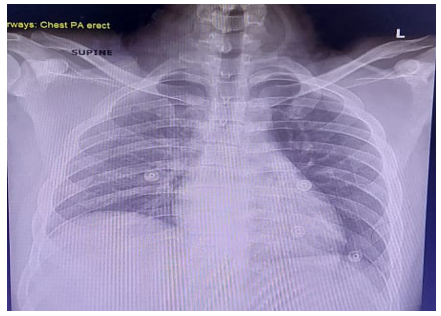
Figure 2: Erect chest x-ray showing no penumo-peritoneum.
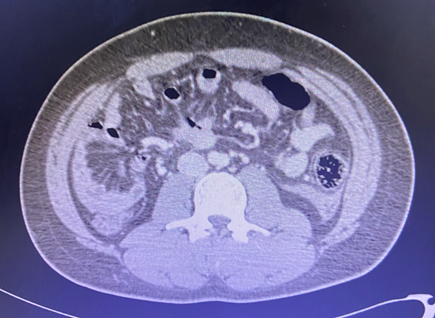
Figure 3: Axial CT images showing small amount of blood in left paracolic gutter.
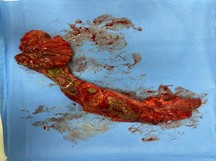
Figure 4: Image showing grade 3 sigmoid colon injuries post-resection.
Discussion
A seat-belt sign describes bruising of the abdomen of an individual wearing a seatbelt and involved in a motor vehicle accident. The presence of this sign generally serves as an indication of the force of impact sustained during collision. The mechanism of this injury involves compressive and shearing forces when the torso propels forward and hyper flexes against the fixed seatbelt (fulcrum), with a sudden increase in intra-abdominal pressure [5].
This results in lacerations or transections of the bowel wall, mural and mesenteric hematomas and de-vascularization [1,4].
Colon injuries are rarely encountered from blunt abdominal trauma, with the reported incidence around 0.1% to 1.1% [1,3,4]. The most common cause is motor vehicle accidents with assault, occupational trauma and falls also reported in the literature [3-5].
The transverse colon is considered relatively vulnerable in blunt trauma because of its mobile intra-peritoneal location. The sigmoid colon is relatively less vulnerable, thought to be because of its protected position within the pelvis [4].
Most colonic injuries are partial thickness, with a documented 3% of laparotomy cases having full thickness injuries) [1]. Additionally, colonic injuries in blunt trauma are typically associated with other visceral injuries, particularly solid organs and the small intestine.
Isolated colon injury, however, is a very rarely encountered condition [5]. Therefore, the presence of a seatbelt sign should always alert the surgeon to the possibility of intra-abdominal injury.
Abdominal tenderness, guarding, distension, abdominal wall contusions and blood on digital rectal examination are important findings to suspect colonic injury from blunt trauma [5].
In these patients, the time interval between admission to hospital and definitive surgical management is extremely important and the rate of complications is significantly higher if this interval extends beyond 24 hours [5].
Documented studies highlight the value of serial physical examinations and close observation of patients with a seatbelt sign and suspicion for intra-abdominal injuries. Signs of peritonitis are said to occur within the first 6 hours of presentation and should be identified during serial assessments [3].
No one specific radiological modality is considered accurate enough to diagnose an isolated colonic injury from blunt trauma. Plain X-rays, performed routinely in trauma, don’t give much information. Ultrasound can identify free fluid in the abdomen but rarely any finding specific to bowel injury. Computed Tomography (CT) scans can provide more information regarding the intra-abdominal viscera and may be considered the most appropriate imaging in abdominal trauma. However, the diagnosis of colonic injury may still be missed because the injury is usually initially subtle in a stable patient [4,5]. In the majority of cases, like ours, intra-peritoneal fluid may be the only finding of a significant colonic injury at initial CT evaluation.
On the other hand, there are some pathognomonic signs: the presence of extra-luminal gas, contrast or intestinal content or discontinuity of the bowel wall suggests overt injuries to the colon itself. Mesenteric injuries can also progress to devascularisation of the bowel, suggested by ischemic changes and active bleeding (suggested by contrast blush) [1,6].
Hefny et al reported that repeated CT done eight hours post-injury may identify colonic injuries early. Some reports suggest repeating abdominal CT if the condition of an initially stable patient fails to improve or deteriorates after 8-12 hours. Also, exploratory laparotomy should be considered early for patients with high clinical suspicion for colonic injury, even if repeat CT scans are non-specific and accepting a documented negative laparotomy rate of 40% [5,6].
Colonic injuries are graded based on their severity, identified at the time of surgery. Flint et al. introduced a grading scale, but the American Association for the Surgery of Trauma (AAST) developed the more commonly referenced Colon Injury Scale (Table 1).
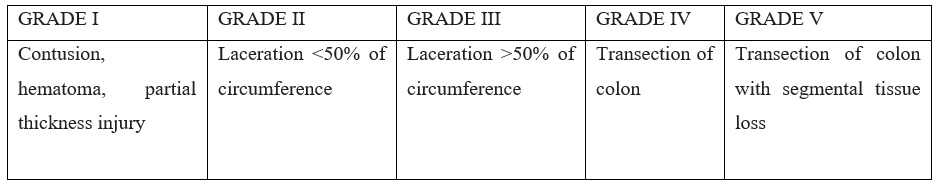
Non-destructive colonic injuries (CIS 1-3) are considered amenable to attempts at primary repair. The management of more severe injuries, however, is less clear. These patients traditionally would have undergone faecal diverting procedures. In 2001, Demetriades et al. prospectively compared the outcomes between primary repair and faecal diversion in patients with various degrees of colonic injuries from any trauma, with no significant difference [1]. Thus, contemporary literature favours primary repair/anastomosis. When ostomy is recommended, it is usually reserved for patients in shock/extremis, or with significant comorbidities [4]. In our case, a decision was made for faecal diversion due to the patient’s instability and need for inotropic support during surgery.
More recently, the concept of ‘acute care laparoscopy’ is emerging, with the intention of bringing the advantages of minimally invasive surgery to acutely ill patients: the only real contraindication being hemodynamic instability/ shock [1]. While available at our centre, laparoscopy was not considered for this case, as our patient was considered unstable due to intra-abdominal sepsis.
Conclusion
Isolated colon injuries are rare after blunt abdominal trauma. This low incidence and a lack of definitive diagnostic methods can lead to delays in diagnosis and management and contribute to high morbidity and mortality. This case report aims to raise clinical suspicion for delayed colonic injury from blunt trauma and its effect on surgical decision making, as there is no standard algorithm for management in these cases.
The presence of a seat-belt sign on the abdomen must be followed with intensive monitoring and repeat examination. If persistent or worsening symptoms, repeat CT or emergent surgery must be considered.
References
- Vailas MG, Moris D, Orfanos S, Vergadis C, Papalampros A. Seatbelt sign in a case of blunt abdominal trauma; what lies beaneath it? BMC Surg, 2015; 15: 121.
- Kopperundevi V, Vimala G, Vyashnavi S, Kannan R. A rare case of isolated sigmoid colon injury in blunt trauma abdomen: A case report. International Surgery Journal, 2022; 9(3): 759-762.
- Biswas S, Adileh M, Almogy G, Bala M. Abdominal injury patterns in patients with seatbelt signs requiring laparotomy. J Emerg Trauma Shock, 2014; 7(4): 295-300.
- Al Shareef B, Al Jurushi R, Al Saleh N. Delayed presentation of an isolated sigmoid Colon injury following blunt abdominal trauma: A case report with review of literature. Int J Surg Case Rep, 2021; 83.
- Ho TH, Chang SW, Yeh HW, Yeh CB. Occult perforation with circumferential ischaemic injury of the sigmoid colon following seat-belt trauma: a case report. Hong Kong Journal of Emergency Medicine, 2017; 24(2): 100-103.
- Ammar AS, Khalid R, Saeed S, Naqi SA. A Rare Case of Isolated Sigmoid Colon Perforation in Patient with Blunt Trauma Abdomen. J Emerg Med Trauma Surg Care, 2020; 7: 053.

