Femoral Hernia Containing Urinary Bladder
Bachar Amine, Essaidi Zakaria, El Azhari Ilias*, Elabbassi Taoufik and Lefriyekh Mohamed Rachid
Department of General Surgery, Faculty of Medicine and Pharmacy, Ibn Rochd University Hospital Center, University of Hassan II, Casablanca, Morocco
Received Date: 18/01/2024; Published Date: 01/07/2024
*Corresponding author: El Azhari Ilias, Department of General Surgery, Faculty of Medicine and Pharmacy, Ibn Rochd University Hospital Center, University of Hassan II, Casablanca, Morocco
Abstract
Introduction: Inguinal bladder hernia (IBH) is a rare clinical condition, despite the proximity of the bladder to the inguinal canal. Femoral bladder hernias (FBH) are more prevalent in females than males and less common than inguinal bladder hernias. The majority of patients with bladder hernias are asymptomatic, and diagnosis is made intraoperatively. We report a rare case of a femoral bladder hernia which the diagnosis was made intraoperatively.
Presentation of Case: A 54 years-old female was admitted to our department with a history of left inguinal swelling that was gradually increasing in size. Physical exam revealed painless and reducible femoral hernia, skin above the hernia was without signs of inflammation. A contrast enhanced abdominal computed tomography showed a right femoral hernia with fluid content. Ultrasound (US) revealed an Amyand hernia with fluid content raising suspicion to mucocele of the appendix. The patient was operated the left inguinal canal’s exploration revealed a portion of the urinary bladder inside the femoral hernia. The femoral hernia and defect were fixed with a polypropylene mesh via the Rives technique. The patient recovered well and was discharged one day after surgery.
Discussion and Conclusion: Femoral bladder hernias are extremely uncommon, with the vast majority being diagnosed intraoperatively.
Risk factors include male gender, advanced age, intravesical obstruction and benign prostatic hypertrophy. Most bladder hernias are asymptomatic. Radiographic imaging is not routinely performed in the workup of inguinal or femoral hernias. The standard treatment of inguinal bladder hernias is an open inguinal incision or in less cases with a laparoscopic approach, it involves a bladder reduction or on rare occasion partial resection, FBH remains a constant trap for the surgeon before the diagnosis, during herniorrhaphy, and even in the postoperative period.
Keywords: Femoral bladder hernias, urinary bladder
Introduction
Inguinal bladder hernia (IBH) is a rare clinical condition, despite the proximity of the bladder to the inguinal canal. Urinary bladder is found in 1–5% of inguinal hernias (IH) [1]. Femoral bladder hernias are more prevalent in females than males and less common than inguinal bladder hernias [2].
The majority of patients with bladder hernias are asymptomatic, and diagnosis is made intraoperatively [3].
We report a rare case of a femoral bladder hernia which the diagnosis was made intraoperatively. This work has been reported in line with the SCARE criteria [4].
Case Presentation
A 54 years-old female was admitted to our department with a history of left inguinal swelling that was gradually increasing in size. Her past medical history includes hypertension and ulcerative colitis. She had no past surgical history or smoking history, she denied vomiting, hematuria or dysuria. Physical exam revealed painless and reducible femoral hernia, skin above the hernia was without signs of inflammation.A contrast enhanced abdominal computed tomography showed a right Femoral hernia with fluid content (Figure 1). Ultrasound (US) revealed an Amyand hernia with fluid content raising suspicion to mucocele of the appendix.The patient was operated after a Foley catheter was inserted into the bladder without difficulties. The left inguinal incision was made and the left inguinal canal’s exploration revealed a portion of the urinary bladder inside the femoral hernia (Figure 2), The femoral hernia sac was initially difficult to differentiate from the bladder due to its thickness, The bladder was distended with saline solution via the urinary catheter confirming the bladder herniation, then it was reduced, unopened to the extraperitoneal space. Inside the hernia sac a normal appendix was found. The femoral hernia and the defect were fixed with a polypropylene mesh via the Rives technique. The patient recovered well and was discharged one day after surgery.
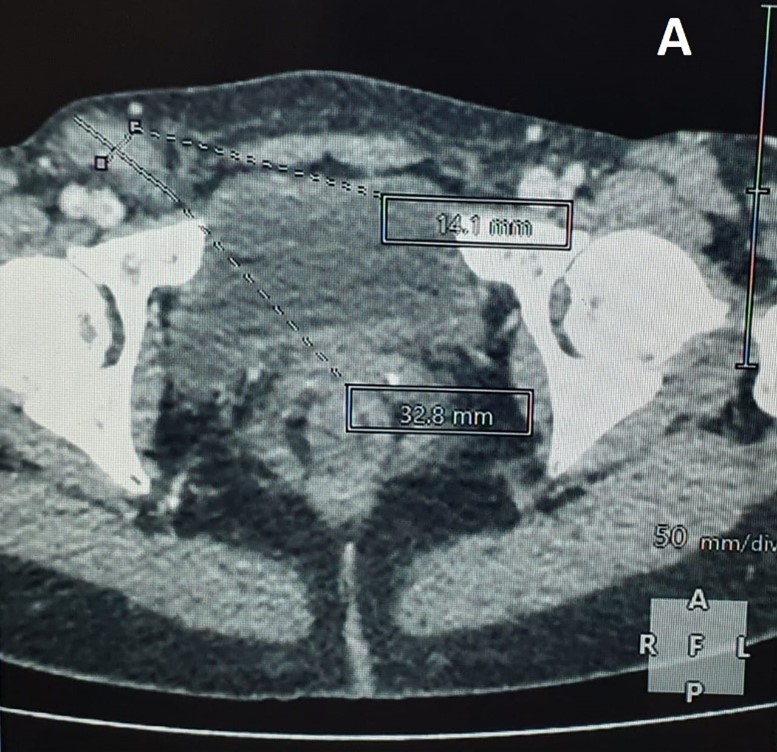

Figure 1 (A, B): CT scan of the abdomen (axial: A and sagittal: B planes) revealing a femoral hernia with fluid content.
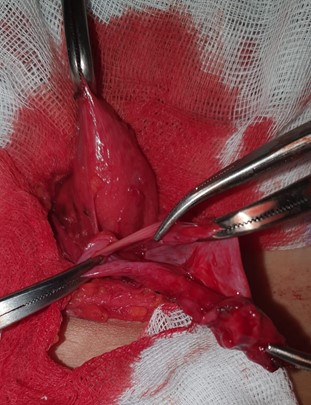
Figure 2: Intraoperative photograph showing the femoral hernia sac and the distended bladder after catheter was being filled with sterile saline.
Discussion
Femoral bladder hernias are extremely uncommon, bladder hernia accounts only for 0.4–3% of adult inguinal hernia cases [5].
only 7% of inguinal bladder hernias are diagnosed prior to surgery, with the vast majority being diagnosed intraoperatively and 16% diagnosed postoperatively due to complications including bladder injury and leakage [6].
Risk factors include male gender, advanced age, intravesical obstruction and benign prostatic hypertrophy [7] in our case the patient was a 54 years-old female.
Most bladder hernias are asymptomatic, usually discovered intraoperatively or during imaging studies performed for other purposes, however they may have nonspecific symptoms including nocturia, urinary frequency, urgency hematuria and two-stage micturition acute renal failure in some rare massive bladder herniation [8].
Radiographic imaging is not routinely performed in the workup of inguinal or femoral hernias but ultrasonography, cystography, and CT have all been utilized to confirm the diagnosis of the bladder hernia [3].
The standard treatment of inguinal bladder hernias is an open inguinal incision and in certain cases a laparoscopic approach, it involves bladder reduction or on rare occasion partial resection, bladder resection is recommended only in cases with bladder wall necrosis, true herniated bladder diverticulum, a tight hernia neck, or tumor in the herniated bladder followed by hernia repair that can be performed with or without the use of a mesh to prevent recurrence [9].
Conclusion
FBH remains a constant trap for the surgeon before the diagnosis, during herniorrhaphy, and even in the postoperative period [10]. Careful history and physical examination are the key in establishing a preliminary diagnosis
We present a case report of femoral bladder hernia in a middle-aged woman that presented as left lower quadrant pain, groin pain, and dysuria. Diagnosis was confirmed intraoperatively. The hernia was surgically reduced and the defect repaired without complications.
Acknowledgements: None.
Conflicts of Interest: All the authors have no personal or financial conflicts of interest regard this case report
Funding: No sources of funding to declare.
Consent: Written informed consent was obtained from the patient for publication of this case report and accompanying image
References
- Inage K, Mizusawa H, Mimura Y, Shimizu F. Patient with inguinal hernia containing the urinary bladder complicated by bladder stones. IJU Case Reports, 2019; 2(5): 276‑278.
- Biswas S, Morel EM, Petersen K, McCrae A. Incarcerated Bladder Diverticulum in a Femoral Hernia Presenting as Recurrent Hematuria. Cureus, 2020.
- Taskovska M, Janež J. Inguinal hernia containing urinary bladder-A case report. International Journal of Surgery Case Reports, 2017; 40: 36‑38.
- Agha RA, Fowler AJ, Saeta A, Barai I, Rajmohan S, Orgill DP, et al. The SCARE Statement: Consensus-based surgical case report guidelines. International Journal of Surgery, 2016; 34: 180‑186.
- Omari AH, Alghazo MA. Urinary bladder diverticulum as a content of femoral hernia: a case report and review of literature. World J Emerg Surg, 2013; 8(1): 20.
- Sarr A, Ondo CZ, Sow Y, Fall B, Thiam A, sine B, et al. Hernie inguinale de la vessie: à propos de 8 cas. Pan Afr Med J, 2015.
- Elkbuli A, Narvel RI, McKenney M, Boneva D. Inguinal bladder hernia: A case report and literature review. International Journal of Surgery Case Reports, 2019; 58: 208‑211.
- El Anzaoui J, El Harrech Y, Abbaka N, Touiti D, Lahkim M, Fihri JF, et al. Hernie inguinale ou vésicale? CUAJ, 2013; 7(11‑12): 837.
- Rachiwong L, Wiboonkhwan N ak, Cheewatanakornkul S. Advantages of minimally invasive approach for inguinal bladder hernia repair: case report and literature review. Laparosc Surg, 2022; 6: 8-18.
- Moufid K, Touiti D, Mohamed L. Inguinal Bladder Hernia: Four Case Analyses.

