Atypical Case of Cardiorenal Syndrome
Abshiro H Mayow1,*, Samer Kholoki2
1George’s University School of Medicine, Grenada
2Department of Internal Medicine, Community First Medical Center, USA
Received Date: 20/02/2024; Published Date: 26/06/2024
*Corresponding author: Abshiro H Mayow, George’s University School of Medicine, Grenada
Abstract
Cardiorenal Syndrome (CRS) is a disease of the heart and kidneys where abnormalities in one organ may have adverse consequences on the other. A combination of cardiovascular and renal abnormalities requires a unique diagnostic approach and immediate intervention to reduce morbidity and mortality rates. Delays in treatment are associated with hemodynamic instability, hospitalizations, and permanent disability in patients with CRS.
We present a case of an 83-year-old male who presented in the emergency room with altered mental status due to acute kidney injury and multiple comorbidities, including hypertension, chronic obstructive pulmonary disease, stroke, carotid atherosclerosis, and coronary artery disease. ECG showed atrial fibrillation. Labs showed hyperkalemia, increased serum creatinine level, increased serum urea level, and decreased bicarbonate level. The patient also had acute non-ST elevation myocardial infarction indicated by increased troponin levels. An imaging study revealed carotid calcifications, 70 percent stenosis in the bulb, hazy perihilar opacities, bilateral pleural effusions, severely abnormal left ventricular function, left hydronephrosis, and benign renal cysts. Cardiac angiography revealed a stenosis in the distal right coronary artery. In addition to emergent dialysis, rocephin was used for urinary tract infections, and a left ureteral stent was placed. The patient's condition improved significantly despite the do-not-resuscitate order, and he was discharged to a skilled nursing facility for further rehabilitation. Thus, this unique case illustrates both the challenges and the success of managing a complex CRS while following ethical principles and taking immediate action to save the patient.
Introduction
Cardiorenal syndrome is characterized by a progressive cardiac malfunction that results in acute kidney injury and hemodynamic instability. There are five types of CRS, including acute and chronic cardiorenal syndrome (Types 1 and 2), acute renocardiac syndrome (Type 3), chronic renocardiac syndrome (Type 4), and secondary cardiorenal syndrome (Type 5) [1].
The signs and symptoms of CRS vary depending on the type and severity of the syndrome. Common symptoms include shortness of breath, fatigue, edema, decreased urine output, and hypertension [1]. The epidemiology of CRS in the USA is not well established, but it is estimated that approximately 30% of patients with heart failure have concomitant renal dysfunction. The diagnosis of CRS is based on clinical presentation, laboratory tests, and imaging studies. Laboratory tests may include serum creatinine, blood urea nitrogen, and electrolyte levels.[2] Imaging studies such as echocardiography and renal ultrasound may also be used to evaluate cardiac and renal function. The treatment of CRS depends on the underlying cause and type of the syndrome. Treatment may include medications such as diuretics, angiotensin-converting enzyme inhibitors, and beta-blockers. In severe cases, dialysis or renal replacement therapy may be necessary. In addition, lifestyle modifications such as weight loss, exercise, and dietary changes may also be recommended [1].
This report explores the case of an 83-year-old male patient with a significant medical history of cardiovascular and cerebrovascular disease, presenting with a complicated Type 1 Cardiorenal Syndrome. This patient has a history of NSTEMI which was concluded with CT angiography revealing arterial stenosis and elevated cardiac Troponins. It was imperative that the medical team find a balance between saving the patient's life and adhering to his ethical rights despite the available medical management for such conditions. In this case, some interventions were impeded by the patient's partial DO Not Resuscitate (DNR). The medical team, however, developed a unique method for optimizing patients' health without breaching ethical guidelines.
Case Presentation
An 83-year-old male was brought to the emergency department with altered mental status for the past 3–4 days and was observed to have stool incontinence. In the emergency department, the patient was noted to be anemic with hemoglobin at 7 g/dL, but he had no history of hematochezia or melena. His medical history included chronic obstructive pulmonary disease, hypertension, stroke, and coronary artery disease, but no reported renal disease. The patient had coronary artery angioplasty of the left anterior descending and circumflex arteries four years prior to presentation. EKG showed atrial fibrillation with a rapid ventricular response. Intravenous diltiazem was administered, which resulted in an improvement in heart rate.
Initial workup showed an elevated troponin level of 12 ng/mL (normal range: 0–0.44 ng/mL), potassium levels of 5.8 mEq/L (normal range: 3.5 to 5.2 mEq/L), creatinine level of 14 mg/dL (normal range: 0.7 to 1.3 mg/dL), blood urea nitrogen level of 195 mg/dL (normal range: 7 to 20 mg/dL) and a low bicarbonate level of 9 mEq/L (normal range: 22-29 mEq/L). Subsequently, the patient was diagnosed with acute kidney injury, severe metabolic encephalopathy, and acute non-ST elevation myocardial infarction. The patient was started on rocephin for a urinary tract infection, and urgent, emergent dialysis was done for 2.5 hours by placing a central line. For further investigation, a CT scan of the neck and head was performed, which showed prominent calcifications at the left carotid bulb, along with a 70% short segment stenosis at the bulb and the proximal-most internal carotid artery on the left side and a 30% right carotid stenosis. There was also moderate atherosclerotic irregularity observed in the cavernous and clinoid segments of the intracranial left internal carotid artery. The imaging was negative for further rate-limiting stenosis, and there was no evidence of intracranial occlusive disease. The CSF spaces were found to have moderate generalized atrophy, and no hemorrhage or mass was found.
A CT scan of the abdomen and pelvis revealed moderate hydronephrosis in the left kidney with a prominent hydroureter on the left, which was dilated down to a stone in the left mid-ureter measuring 5.7 x 6.9 cm, and large benign cysts in both kidneys. Additionally, the patient had stenosis in the lower lumbar spine. A portable chest X-ray revealed mild pulmonary vascular congestion, hazy perihilar opacities at the right base, and a mildly enlarged heart. The abdominal X-ray showed a non-obstructive bowel gas pattern. Figure 1 shows an abdominal X-ray.
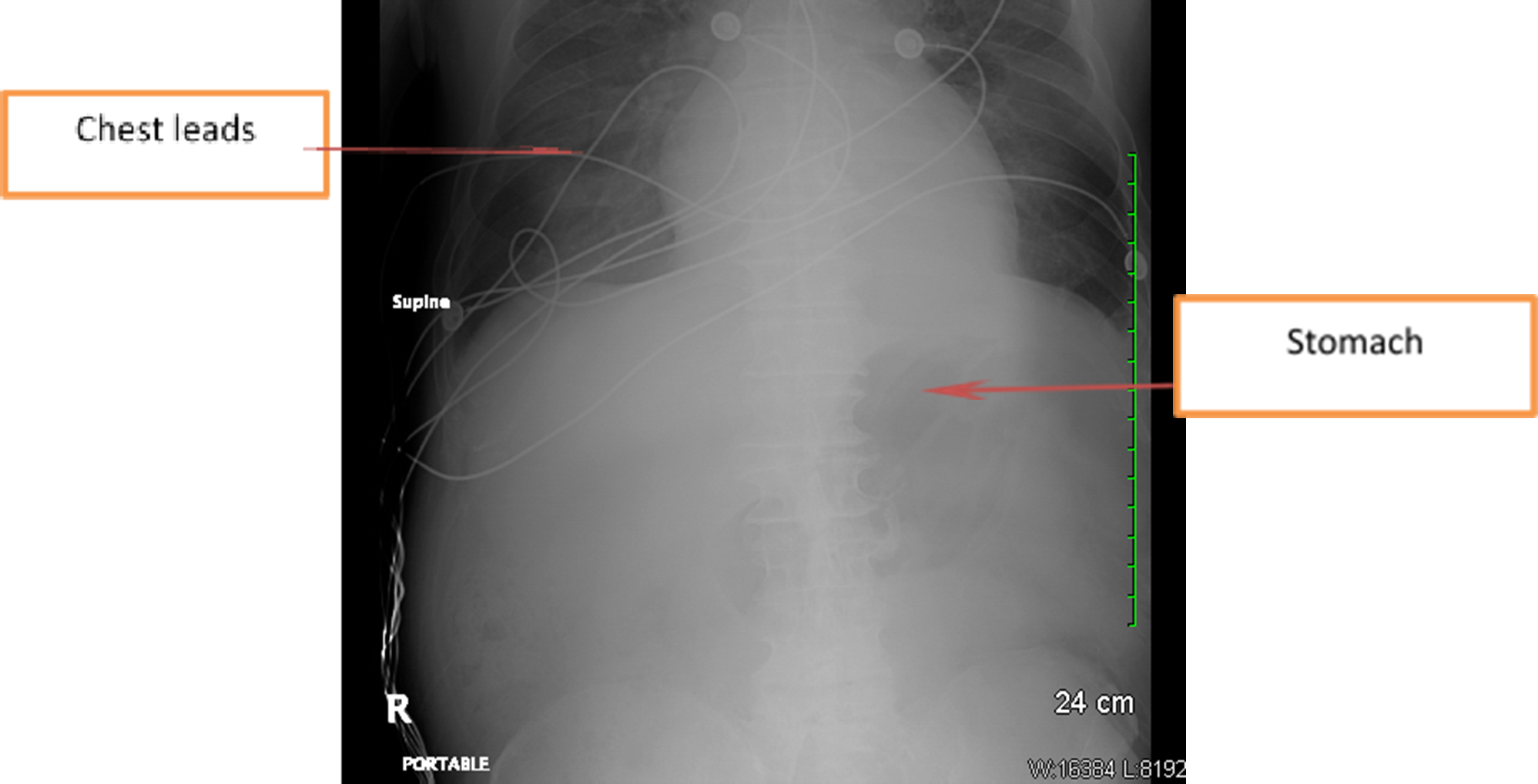
Figure 1: Abdominal X-ray showing non-obstructive bowel gas pattern.
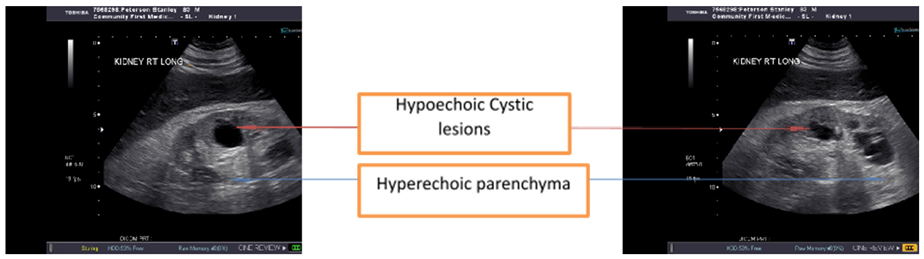
Figure 2: Right renal ultrasound showing hypoechoic cystic appearing space-occupying structures and hyperechoic parenchyma.
On targeted bilateral renal ultrasound, increased cortical echogenicity was noted in both kidneys. Pelviectasis and caliectasis were found in the left kidney, which was consistent with underlying hydronephrosis. Figure 2 shows the right renal ultrasound images.
The transthoracic echocardiography showed severely abnormal left ventricular function and bilateral pleural effusions. Based on the available clinical information, the patient's condition suggested a simultaneous occurrence of acute myocardial infarction and pulmonary edema, possibly resulting from renal failure and congestive heart failure. The procedure of permacath placement was performed under fluoroscopic guidance.
CT angiography of the heart revealed a lesion with a 60% stenosis on the distal right coronary artery, while the left main coronary artery was normal. For left hydronephrosis, the patient underwent cystoscopy with the successful insertion of a stent in the left ureter measuring 6F x 26 cm. The contrast was injected, revealing a stone in the mid-ureteral region with associated hydronephrosis. A 16F Foley catheter was also placed. Postoperatively, the same diagnosis was confirmed, and it was noted that there was no Benign Prostatic Hyperplasia (BPH)
obstruction present following transurethral resection of the prostate (TURP), and the patient had mild cystitis. The patient was transferred to the post-anesthesia care unit (PACU) and was found to be in good condition upon disposition. This was a challenging case as the patient had a do-not-resuscitate (DNR) order, and invasive procedures were declined by the patient's power of attorney (son-in-law), who refused any invasive procedures. Nevertheless, due to the extensive management efforts of the internal medicine team, the patient went from AOX0 to AOX3 within one month. Upon discharge, the patient was in a hemodynamically stable condition; however, he required rehabilitation and was thus discharged to a skilled nursing facility (SNF) with onsite hemodialysis.
Discussion
The coexistence of either acute or chronic heart or kidney dysfunction, known as cardiorenal syndrome (CRS), triggers a series of negative feedback mechanisms that harm both organs [3]. The activation of systems that modulate bidirectional and dynamic pathways links kidney function and heart performance. The pathophysiology of CRS is more complex and includes poor renal perfusion, increased venous pressure, and increased intraabdominal pressure, despite the fact that excessive use of diuretics is frequently to blame [3], [4]. So, it is usually referred to as a complex pathophysiological condition of the heart and kidneys wherein acute or persistent dysfunction in one organ can lead to acute or persistent dysfunction in the other [4].
A study revealed that, in patients with acute kidney injury (AKI), sepsis was the leading cause of death, with cardiovascular disease coming in second [5]. Another study found that patients with AKI that required dialysis had higher long-term risks of coronary events and all-cause mortality, regardless of whether their condition later progressed to chronic kidney disease (CKD) [6]. This finding demonstrated the independent relationship between AKI and long-term cardiovascular risk. Due to cardiovascular involvement, this condition is linked to higher rates of long-term mortality, rehospitalization, and in-hospital mortality [7]. According to a study by Bock and Gottlieb, patients with severe aortic stenosis (AS) may develop a cardiorenal syndrome that is resistant to medical intervention, along with acute decompensated heart failure. Compared to the effects of either disease alone, heart failure and renal failure have synergistic effects that increase the negative outcomes [8]. Similar circumstances of CRS requiring urgent transcatheter aortic valve replacement have also been documented [9]. When used in the clinical setting of CRS, biomarkers of cardiac and renal injury may offer useful information by serving to identify early cardiac or renal injury, the healing process, and long-term consequences [10].
Mandal et al. reported a case of cardiorenal syndrome that was successfully treated with ultrafiltration therapy [11]. It is being researched to use vasopressin antagonists [12], adenosine antagonists [13], and ultrafiltration as new therapeutic approaches [14]. At this time, the prudent application of mechanical circulatory support with left ventricular assist devices is the only effective treatment for heart failure with progressive cardiorenal syndrome. It is reported to improve renal dysfunction and to restore hemodynamically [15]. However, due to worries about device-related morbidity and poor durability, the use of such therapy in less severe cases of heart failure is still limited [14].
This is a case of an 83-year-old male who presented with altered mental status. He had a past medical history of chronic obstructive pulmonary disease, hypertension, coronary artery disease, stroke, and coronary artery angioplasty of the left anterior descending and circumflex arteries. Investigations revealed elevated troponin, potassium, creatinine, and blood urea nitrogen levels on blood workup and atrial fibrillation on EKG.[11] He was diagnosed with acute kidney injury with severe metabolic encephalopathy and acute non-ST elevation myocardial infarction.[16] He was also found to have hydroureter, hydronephrosis, and mild pulmonary vascular congestion. He was diagnosed with a simultaneous occurrence of acute myocardial infarction, pulmonary edema, possibly resulting from renal failure and congestive heart failure.[17] He was started on dialysis, and he underwent a cystoscopy for hydronephrosis. His condition improved, and he was shifted to a nursing facility. This is a case presentation of a complex cardiorenal syndrome that was treated successfully [18].
Conclusion
The aim of this report is to investigate Cardiorenal Syndrome (CRS), a condition that results from an interaction between cardiac and renal problems. This patient had comorbidities, including acute kidney injury, atrial fibrillation, and acute non-ST elevation myocardial infarction. He was treated with medical management, urgent dialysis, antibiotic therapy, and ureteral stent implantation in order to achieve a good outcome despite his advanced age and resistance to invasive procedures. Our multidisciplinary approach, close supervision, and adherence to ethical principles led to a substantial improvement in the patient's clinical condition. Therefore, this study contributes to the existing literature about the importance of prompt and thorough intervention for CRS patients to minimize the risk of deteriorating renal and cardiac function, hemodynamic instability, multiorgan failure, and death.
References
- Di Lullo L, Bellasi A, Barbera V, Russo D, Russo L, Di Iorio B, et al. Pathophysiology of the cardio-renal syndromes types 1-5: An uptodate. Indian Heart Journal, 2017; 69(2): 255–265. doi: 10.1016/j.ihj.2017.01.005
- Tasić D, Radenkovic S, Stojanovic D, Milojkovic M, Stojanovic M, Ilic MD, et al. Crosstalk of various biomarkers that might provide prompt identification of acute or chronic cardiorenal syndromes. Cardiorenal Medicine, 2016; 6(2): 99–107. doi:10.1159/000437309
- Rangaswami J, Bhalla V, Blair JEA, Chang TI, Costa S, Lentine American Heart Association Council on the Kidney in Cardiovascular Disease and Council on Clinical Cardiology. Cardiorenal syndrome: Classification, pathophysiology, diagnosis, and treatment strategies: A scientific statement from the American heart association. Circulation, 2019; 139(16): e840–e878. doi:10.1161/CIR.0000000000000664
- Lee SA, Cozzi M, Bush EL, Rabb Distant organ dysfunction in acute kidney injury: A review. American Journal of Kidney Diseases: The Official Journal of the National Kidney Foundation, 2018; 72(6): 846–856. doi: 10.1053/j.ajkd.2018.03.028.
- Tang WHW, Mullens Cardiorenal syndrome in decompensated heart failure. Heart (British Cardiac Society), 2010; 96(4): 255–260. doi:10.1136/hrt.2009.166256
- Ronco C, Haapio M, House AA, Anavekar N, Bellomo Cardiorenal syndrome. Journal of the American College of Cardiology, 2008; 52(19): 1527–1539. doi: 10.1016/j.jacc.2008.07.051
- Uchino S. Acute renal failure in critically ill PatientsA multinational, multicenter JAMA: The Journal of the American Medical Association, 2005; 294(7): 813. doi: 10.1001/jama.294.7.813
- Wu V-C, Wu C-H, Huang T-M, Wang C-Y, Lai C-F, Shiao C-C, et al. Long-term risk of coronary events after Journal of the American Society of Nephrology: JASN, 2014; 25(3): 595–605. doi: 10.1681/asn.2013060610
- Lanfear DE, Peterson EL, Campbell J, Phatak H, Wu D, Wells K, et al. Relation of worsened renal function during hospitalization for heart failure to long-term outcomes and rehospitalization. The American Journal of Cardiology, 2011; 107(1): 74–78. doi: 10.1016/j.amjcard.2010.08.045.
- Bock JS, Gottlieb SS. Cardiorenal syndrome: new perspectives. Circulation, 2010; 121(23): 2592–2600. doi: 10.1161/CIRCULATIONAHA.109.886473
- Kim H, Lee J-H. Emergency transcatheter aortic valve replacement for a patient with decompensated severe aortic stenosis accompanied by cardiorenal syndrome: a case BMC Cardiovascular Disorders, 2018; 18(1). doi: 10.1186/s12872-018-0791-7
- Husain-Syed F, McCullough PA, Birk H-W, Renker M, Brocca A, Seeger W, et al. Cardio-pulmonary-renal interactions. Journal of the American College of Cardiology, 2015; 65(22): 2433–2448. doi: 10.1016/j.jacc.2015.04.024
- Mandal G, Elraiyah T, Nandra C, Greco R, Schirger A case of acute decompensated heart failure complicated by cardiorenal syndrome treated with ultrafiltration. Cureus, 2022. doi: 10.7759/cureus.29013
- Konstam Effects of oral tolvaptan in patients hospitalized for worsening heart FailureThe EVEREST outcome trial. JAMA: The Journal of the American Medical Association, 2007; 297(12): 1319. doi: 10.1001/jama.297.12.1319
- Givertz MM, Massie BM, Fields TK, Pearson LL, Dittrich The effects of KW-3902, an adenosine A1-receptor antagonist,on diuresis and renal function in patients with acute decompensated heart failure and renal impairment or diuretic resistance. Journal of the American College of Cardiology, 2007; 50(16): 1551–1560. doi: 10.1016/j.jacc.2007.07.019
- Brown JR, Uber PA, Mehra The progressive cardiorenal syndrome in heart failure: Mechanisms and therapeutic insights. Current Treatment Options in Cardiovascular Medicine, 2008; 10(4): 342–348. doi: 10.1007/s11936-008-0054-5
- Butler J, Geisberg C, Howser R, Portner PM, Rogers JG, Deng MC, et al. Relationship between renal function and left ventricular assist device use. The Annals of Thoracic Surgery, 2006; 81(5): 1745–1751. doi: 10.1016/j.athoracsur.2005.11.061.
- Mehra Ventricular assist devices: Destination therapy or just another stop on the road? Current Heart Failure Reports, 2004; 1(1): 36–40. doi: 10.1007/s11897-004-0015-6.

