Saddle Pulmonary Embolism: A Rare Case of Proximal Pulmonary Embolism
Hamissou Ibrahim*, Nacocan Domiciano, Amri Rachida, Cherti Mohammed
Department of Cardiology ibn Sina Health Care Center, University Mohammed-V of Rabat, Morocco
Received Date: 14/02/2024; Published Date: 25/06/2024
*Corresponding author: Hamissou Ibrahim, Department of Cardiology ibn Sina Health Care Center, University Mohammed-V of Rabat, Morocco
Abstract
Saddle pulmonary embolism is defined as the presence of a visible thrombus located at the bifurcation of the pulmonary artery trunk showing an aspect of “saddle” on a chest contrasted tomography scan. This is a rare case occurring in only 5.2% of patients with pulmonary embolism [1].
We report the case of a 93-year-old female patient who had no thrombo-embolic past medical history, she had got the gall bladder operation 25 years ago. The patient was admitted for a dyspnea associated with a chest pain and desaturation related to a pulmonary embolism confirmed on a chest contrasted tomography scan that has shown a typical aspect of “saddle pulmonary embolism”. Our patient was stable on hemodynamic state and had a high intermediate prognostic risk score. She was managed at the cardiac intensive care unit with anticoagulation that improved her clinically.
Past Medical History
This is a 93-year-old patient, with high blood pression well managed, who had no thrombo-embolic past medical history, but she had got the gall bladder operation 25 years ago.
Differential Diagnosis
The main differential diagnoses are acute left heart failure that may cause acute dyspnea and other causes of acute chest pain: Myocardial infarction, pericarditis and aorta dissection.
History of presenting complaint and physical examination
She consulted at the emergency department for an acute dyspnea associated with a chest pain. During the general exam, she was conscious, but with oxygen desaturation at 88% in ambient air. Her blood pressure was normal (126/76mmhg) and with 92 beats per minute of heart rate.
The physical exam found no cardio-respiratory murmurs nor any heart failure signs.
Investigations
Infront of the acute dyspnea and oxygen desaturation with normal physical exam, we suggested a pulmonary embolism. Geneva score modified was calculated at 4 (Age >65 years and Heart rate between 75-94) reflecting an intermediate clinical probability of pulmonary embolism and the d-dimers were elevated at seven times the normal value. Based on previous data, a chest contrast tomography scan angiogram was requested, and has shown a proximal bilateral pulmonary embolism with the “Saddle” typical aspect (Figure 1) with an extension to the division branches (Figure 2).
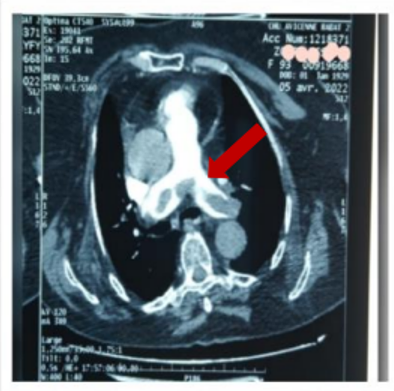
Figure 1: Pulmonary embolism in the saddle.
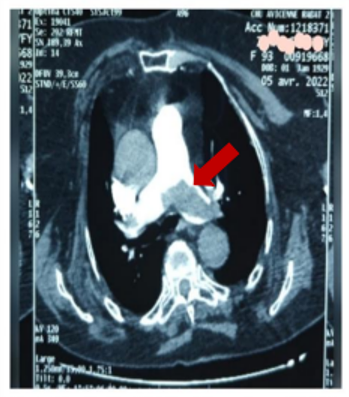
Figure 2: Extension of the thrombus to the dividing branches.
Management
The PESI-s score was calculated at 3 (Age >80 years, Oxygen desaturation <90% on ambient air), there were ischemia signs of the right ventricle and the troponin rate was positive. According to the European Society of Cardiology guidelines our patient had a high intermediate risk of complications, which required her transfer to the cardiology intensive care unit for oxygenation and a curative anticoagulation (Non-Vitamin-K oral anticoagulant) management.
Follow-up
The next following day, our patient improved clinically, her breathing was normal with 98% of oxygen saturation on ambient air and was stayed hemodynamically stable without any complaints.
An etiological workup based on of the lower limbs venous doppler ultrasound, thoraco-abdomin-pelvic contrast tomography scan and the screening of tumor markers was normal.
She was discharged after a one-week stay and she should achieve at least 3-6 moths of anticoagulation.
Discussion
Saddle pulmonary embolism has an incidence around 5.2% in patients with pulmonary embolism [1], we also find in other studies incidences ranging from 2.6 to 5.4% [5]. This is a rare case. The main symptom is dyspnea in 72% of cases [6].
The main exam for the diagnosis of proximal pulmonary embolism is a contrasted tomography angiograph in patients with high clinical probability (REVISED GENEVA SCORE).
Despite of their proximal locations with sometimes massive thrombi, saddle pulmonary embolisms are often hemodynamically stable. Even some asymptomatic cases have already been reported in the literature [2]. But they are at intermediate risk of complication requiring a hospitalization in a cardiology intensive care unit [3].
The hemodynamic state of a patient with pulmonary embolism depends on the size of the clots and on the presence of cardio-respiratory comorbidities as well [8].
Patients with stable state can be managed with anticoagulants, however authors reported the possibility of using thrombolytics or even performing an embolectomy in case of hemodynamic instability, with right ventricular dysfunction, and the elevation of troponin. [4,9]
About our 93-years-old patient we could directly do a pulmonary contrast tomography angio-scan without dosing the Dimer, because statistically pulmonary embolisms are more frequent in people over 64 years old (incidence = 6/1000 after 75 years) [7] and her Revised Geneva Score was high. In addition, she presented the main symptom which is dyspnea associated with oxygen desaturation.
Despite the size of the clot and their proximal position at the pulmonary contrast tomography angio-scan, our patient remained hemodynamically stable. This could be explained by his normal lung parenchyma and the fact that he had no previous cardiovascular disease.
The s-PESI score was at high intermediate risk and we start in our patient an anticoagulant treatment.
Learning points:
The saddle pulmonary embolism is a rare type of pulmonary embolism, characterized its “saddle” aspect at pulmonary contrast tomography angio-scan.
People diagnosed with saddle pulmonary embolism are often stable hemodynamically, however they are likely to present complications and then requiring for a close monitoring.
For the treatment, authors recommend anticoagulation therapy except in cases of hemodynamic instability and/or in case of right ventricular dysfunction where thrombolysis or even embolectomy can be necessary.
References
- https://doi.org/10.1016/j.chest.2021.07.819.
- https://journals.sagepub.com/doi/pdf/10.1177/1076029610363588.
- Wong Kevin J, Kushnir Margarita, Billett Henny H. Saddle Pulmonary Embolism: Demographics, Clinical Presentation, and Outcomes, Critical Care Explorations, 2021; 3(6): p e0437 doi: 10.1097/CCE.0000000000000437
- Sardi A, Gluskin J, Guttentag A, Kotler MN, Braitman LE, Lippmann M. Saddle pulmonary embolism: is it as bad as it looks? A community hospital experience. Crit Care Med, 2011; 39(11): 2413-2418. doi: 10.1097/CCM.0b013e31822571b2.
- Alkinj B, Pannu BS, Apala DR, et al. Saddle vs non saddle pulmonary embolism : Clinical presentation, hemodynamics, management, and outcomes. Mayo Clin Proc. Faisant d’elle un cas rare, 2017.
- Pruszczyk P, Pacho R, Ciurzynski M, et al. Short term clinical outcome of acute saddle pulmonary embolism. Heart, 2003; 89(3): 335.
- L'embolie pulmonaire chez les personnes âgées de plus de 65 ans: valeur diagnostique du score de Genève révisé et évaluation des pratiques professionnelles dans un service d'accueil des urgences (cnrs.fr).
- Goldhaber SZ. Echocardiography in the management of pulmonary embolism. Ann Intern Med, 2002; 136(9): 69.
- Wan S, Quinlan DJ, Agnelli G, Eikelboom JW. Thrombolysis compared with heparin for the initial Treatment of pulmonary embolism: a meta-analysis of the randomized controlled trials.

