Enucleation of a Schwannoma with Median Nerve Preservation
Sarita Mejia Jaramillo*, Xochilth Soraida Pinedo Ruan, Carlos Alfredo Bautista Lopez, Alberto Briceño Fuentes and Eduardo Sotelo Anaya
Department of General and GI Surgery, Hospital Civil de Guadalajara “Dr. Juan I. Menchaca”, University of Guadalajara, Guadalajara, México
Received Date: 01/02/2024; Published Date: 19/06/2024
*Corresponding author: Sarita Mejia Jaramillo, Department of General and GI Surgery, Hospital Civil de Guadalajara “Dr. Juan I. Menchaca”, University of Guadalajara, Guadalajara, México
Abstract
Schwannomas are benign, encapsulated, slow-growing and usually solitary tumours originating from Schwann cells of the peripheral nerve sheath. Approximately 25-40% of cases are seen in the head and neck region and they are the most common peripheral nerve tumor of the hand and upper extremity. We report a rare case of the median schwannoma in a woman who had symptoms of pain and paresthesias, she was treated with complete enucleation of the tumor, preserving median nerve, she presented moderate sensory and motor sequelae, however with rehabilitation with physical therapy at 6 months post-surgery the patient only presents mild sensitive sequelae. This kind of complete excision can be considered standard treatment for these tumours, with no recurrences.
Keywords: Schwannoma; Median nerve; Upper limb; Surgery; Enucleation; Nerve preservation; Case Report
Introduction
Neoplasms of the peripheral nervous system represent a heterogeneous group with a wide range of morphological characteristics and biological potential. They can vary from benign and curable through complete excision (such as schwannoma and perineurioma of soft tissues) to benign but potentially aggressive locally (plexiform neurofibroma) or highly malignant (malignant tumors of the peripheral nerve sheath). The most common peripheral nerve tumor in the hand and upper limb are schwannomas, benign tumors originating from Schwann cells.
In most patients, these tumors remain asymptomatic when small. However, as the tumor grows and exerts pressure on the originating nerve, symptoms such as dysesthesias, pain, sensory loss, and weakness may occur. Schwannomas are considered entirely benign and do not undergo malignant transformation. The primary goal in the surgical resection of these lesions is to preserve nerve function and continuity.
Patient Information
The patient is a 46-year-old female who presents with a clinical condition that has been developing for 2 months. She experiences a sensation of a mass in the upper third of her left arm, in the medial region. The mass is causing incapacitating pain and is associated with paresthesias (tingling or prickling sensations) and slight reduction in the range of motion of her hand.
Clinical Findings
Upon examination, a palpable mass of 2x1 cm is identified in the upper left extremity, specifically in the superior medial region. The mass is immobile and has well-defined edges. The patient experiences pain when the mass is palpated, but there are no swollen lymph nodes in the axillary region. The range of motion and sensitivity of the hand are preserved.
Imaging Studies
MRI (Magnetic Resonance Imaging) of the left upper extremity in the Proximal third specifically in the medial region reveals the following findings: (Figure 1-3)
Description:
- A hyperintense oval-shaped, well-defined image measuring approximately 1.8 x 1.1 x 1.7 cm is observed in the deep soft tissues.
- This image is dependent on the median nerve.
- Upon contrast administration, there is mild enhancement of the image (Figure 3)
- The tumor displaces the brachial artery and basilic vein in a posterolateral direction.
Surgical Intervention:
The enucleation of the lesion was performed under general anesthesia. The surgical procedure involved the following steps:
- An incision was made in the left axillary region, and dissection was carried out through the various tissue planes until the tumor dependent on the median nerve was identified (Figure 4(a)).
- The vascular and nerve bundle associated with the tumor was identified and carefully separated from the mass.
- The tumor was dissected circumferentially to ensure complete removal (Figure 4(b)).
- The excised tumor specimen was extracted (Figure 4(c)).
The tumor specimen was sent for histopathological examination (Figure 5), which ruled out malignancy and confirmed the diagnosis of a completely resected conventional schwannoma measuring 1.8 cm.
Follow-Up:
During the immediate postoperative period, the patient experienced moderate sensory and motor sequelae. However, upon commencing physical therapy rehabilitation at 6 months post-surgery, the patient has shown significant improvement in her condition.
Currently, the patient retains sensation throughout the hand and has preserved flexion of the thumb and hand pronation. The only persistent issue is a constant sensation of paresthesia in the dermatome of the median nerve.
Continuous follow-up and rehabilitation have been crucial in achieving these positive outcomes after the surgery.
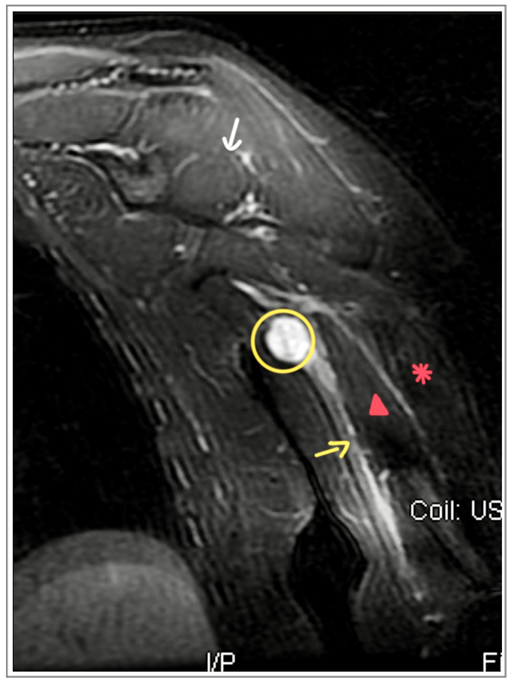
Figure 1: Sagital STIR: 𝇈 schwannoma. ➔ Median nerve. ▲Biceps short head. * Biceps long head.
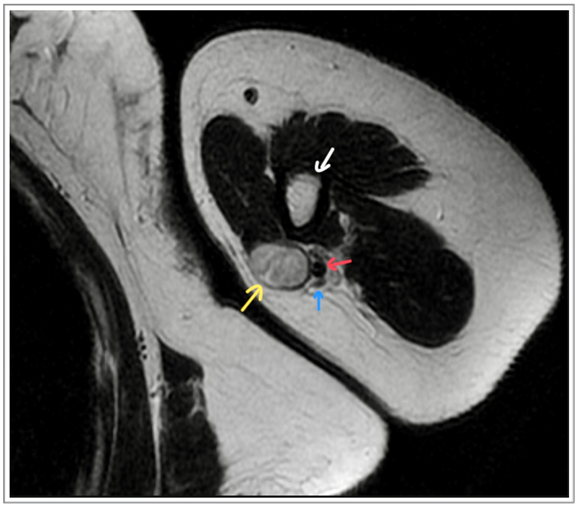
Figure 2: Axial T2: yellow➔ schwannoma, blue ➔ V. Basilic Vein, red ➔ Brauchial Artery ,white ➔ humerus
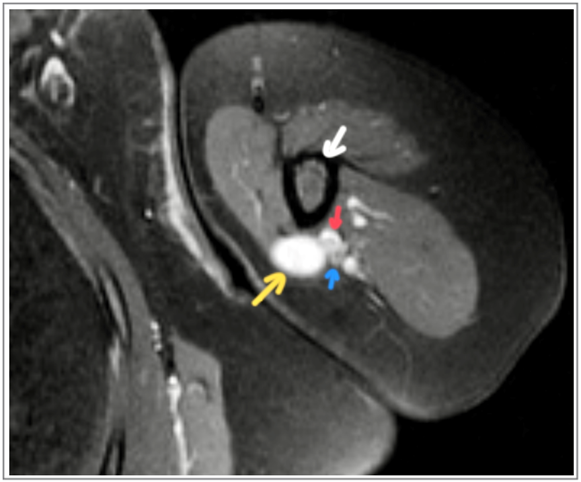
Figure 3: Axial T2 axial with contrast. Yellow ➔ schwannoma, blue ➔ V. Basilic Vein. Red ➔ Brauchial Artery, white ➔ humerus
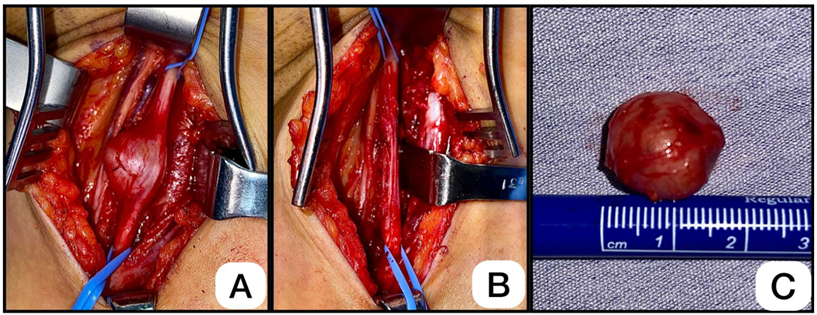
Figure 4: A.) tumor dependent on the Median Nerve B.) Median nerve after enucleation C.) Enucleated schwannoma.
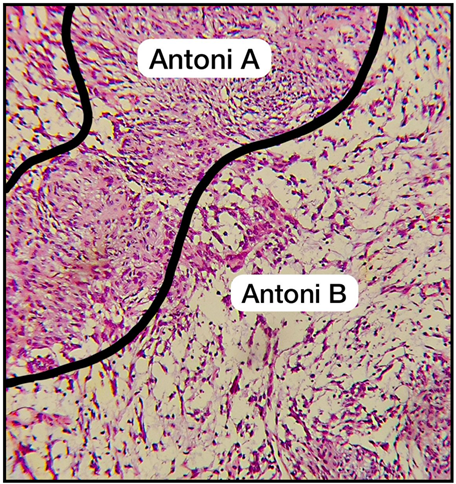
Figure 5: Hematoxylin-eosin stain, Biphasic component of the Schwannoma, with Antoni A areas (hypercellular) and Antoni B areas (hypocellular)."
Discussion and Conclusion
The block excision of nerve trunk schwannomas can lead to significant functional impairment. On the other hand, the meticulous enucleation of the tumor within the nerve trunk preserves most of the nerve fascicles and causes minimal deterioration of nerve function. Therefore, strict adherence to the principle of enucleation is of utmost importance for nerve function preservation. To achieve this, an accurate preoperative diagnosis based on clinical findings and imaging studies is essential.
Conflicts of Interest: There are no disclaimers, or conflicts of interest to declare. The present publication is being submitted in the category of case report. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This paper is not based on any previous communication o meeting. Ethical clearance has been obtained by the authors through a proper informed consent format that the patient signed to authorize the use of his personal information.
Acknowledgements: We would like to express our sincere gratitude to the Department of Radiology at our hospital, specifically to Dr. Endy Hollyver Sanchez Uribe and Dr. Jesús Alejandro Guerrero Velasco, for their invaluable assistance with the interpretation of the images. Additionally, we extend our appreciation to the Department of Pathology, specifically to Dr. Perla Guadalupe Franco del Toro and Dr. Isaac Gerardo Zamorano Mares, for their expert insights and support.
References
- Belakhoua SM, Rodriguez FJ. Diagnostic Pathology of Tumors of Peripheral Nerve. Neurosurgery, 2021; 88(3): 443-456. doi: 10.1093/neuros/nyab021.
- Strike SA, Puhaindran ME. Nerve Tumors of the Upper Extremity. Clin Plast Surg, 2019; 46(3): 347-350. doi: 10.1016/j.cps.2019.02.008.
- Lai Chih-Sheng, Chen I-Chen, Lan Haw-Chang, Lu Chen-Te, Yen Jung-Hsing, Song Ding-Yu, et al. Management of Extremity Neurilemmomas: Clinical Series and Literature Review. Annals of Plastic Surgery, 2013; 71: p S37-S42.

