Management of Rectovaginal Fistula in a 67-Year-Old Female Laparoscopically
Martin D Tanhaei1,2,*, Muresuk Mena2, Naga P Reddy-Mallu2 and Frederick Tiesenga3
1Biomedical Engineering, Johns Hopkins University, Baltimore, USA
2School of Medicine, St. George's University School of Medicine, True Blue, GRD
3General Surgery, Community Medical Center, Chicago, USA
Received Date: 21/01/2024; Published Date: 04/06/2024
*Corresponding author: Martin D Tanhaei, Biomedical Engineering, Johns Hopkins University, Baltimore, USA
Abstract
Rectovaginal Fistula (RVF) management requires adequate psychological support and individualized physiological management plans. Current research underscores the association between RVF development and previous exposure to radiation therapy or a history of intra-abdominal surgeries. This report focuses on the management of a 67-year-old woman with a history of anxiety, depression, COPD, and ovarian cancer who presented with a confirmed rectovaginal fistula. She had a diagnostic laparoscopy, a laparoscopic loop transverse colostomy, and a laparoscopic adhesiolysis. The patient reported no significant issues post-operatively and showed signs of recovery, such as a functional colostomy and food tolerance. Future care plans call for a follow-up for potential colon resection and colostomy reversal, pending continued ovarian cancer treatment. This case emphasizes how crucial it is to manage RVFs using a multidisciplinary approach, particularly when treating individuals with complicated medical histories. This paper focuses on the necessity of planned postoperative care and management using laparoscopic techniques.
Keywords: Laparascopic surgery; Recto-vaginal fistula; Medical management; RVFs
Introduction
Rectovaginal Fistulas (RVFs) can affect quality of life and frequently result in severe morbidity during colorectal surgery. RVFs, which are abnormal connections between the vagina and the rectum, can have various causes. In developed countries, problems from surgical procedures, especially after hysterectomy and colorectal surgeries, are linked to RVFs; however, obstetric trauma is still the leading cause in developing countries [1,2]. Other noteworthy causes include radiation therapy for pelvic malignancies and inflammatory bowel illnesses [3]. The difficulty of radiation therapy and previous surgical procedures can greatly influence the selection of management strategies for patients with a history of pelvic malignancies, adding to the complexity of RVF.
A thorough understanding of the underlying etiology, the architecture of RVFs, and the general health status of the patient are necessary for the management of RVFs. The literature has a detailed variety of methods for repairing RVF, from simple local surgeries to more involved abdominal procedures. These local techniques, like the advancing flap approach, are usually limited to low RVF cases that are straightforward and do not involve a considerable amount of the sphincter. On the other hand, abdominal techniques, like resection with primary anastomosis, are necessary for large, complex fistulas, especially when there has been a history of recurrent illness or failed previous repairs [4]. The surgical options for RVF repair have increased because of recent developments in minimally invasive surgery; laparoscopic and robotic procedures are becoming more and more popular because of their shortened recovery periods and associated lower morbidity [5].
A multidisciplinary approach is a key aspect of RVF management. A thorough evaluation and treatment plan require this kind of care, particularly for individuals who also have diabetes, COPD, or a history of pelvic radiation or cancer. Moreover, patient-specific factors like infection, active inflammation, and overall nutritional status have a significant impact on the surgical approach and subsequent postoperative care [6].
Case Report
A 67-year-old female presented with a few months of foul-smelling vaginal discharge, symptoms of anemia, hematuria, and pyuria. She had a past medical history of ovarian cancer, depression, anxiety, COPD, and the most recent episode of pneumonia. These urinary presentations, along with her past medical history, raised the suspicion of RVF. The patient's medical history included ovarian cancer radiation, which could have led to the RVF formation. Radiological images before her ovarian cancer diagnosis and radiation treatment are depicted in Figure 1 and showed a normal-appearing uterus without any air in the lumen and no apparent fistula.
Preoperative radiological images indicated the presence of air in her vaginal lumen (Figure 2A), vagina (Figure 2B, top arrow), and vaginal canal (Figure 2B, bottom arrow). Physical examinations showed the presence of stool in the vagina. The patient declined any further imaging during and after her surgery. Consequently, additional images, including clinical photography, are not available for this report. The diagnosis of RVF was confirmed based on her history of ovarian cancer radiation and aberrant results from her radiological findings and physical examination.
The complexity of this case and the difficulty in management necessitated the comprehensive management of RVF as the patient had gone through radiation for ovarian cancer. A diagnostic laparoscopy was initiated to explore the lower abdominal cavity precisely to locate any possible fistulas, as they were not visible radiologically. The laparoscopic technique was a critical approach, as it was a minimally invasive technique to visualize the abdominal cavity. A laparoscope was introduced through minimal incisions over the abdominal wall, facilitating visualization of the lower abdominal cavity and pelvic region. The advantage of using the laparoscopic technique in this surgery is that it is because of the patient’s history of ovarian cancer and radiation, which might have resulted in adhesion formation and anatomical abnormalities of the pelvic region.
After diagnostic visualization of the pelvic region, the next step was to remove the adhesions using laparoscopic adhesiolysis due to the discovered adhesions. These adhesions were most likely due to the previous cancer treatments. The adhesions were thoroughly dissected to ensure subsequent healing and avoid future adhesion formation. The laparoscopic approach to adhesiolysis was meticulously chosen to minimize postoperative complications through its accuracy and minimal invasiveness and effectively encourage quicker recovery.
Using a laparoscopic approach, a loop transverse colostomy was initiated to promote healing of the surgical site and prevent additional adhesion formations. The loop transverse colostomy procedure redirected the fecal stream away from the fistula. Hence, the procedure lowered the infection risk and sped up the healing of the affected side. The laparoscopic colostomy reduced the recovery time and risk of further complications, meeting the wishes of the patient for fewer complications post-surgery.
The main goal of this surgery was to holistically manage the patient’s RVF and keep in mind her complex case. Her medical history challenged the team to present a comprehensive plan for the potential ramifications of her long-term health and recovery from surgery. During the postoperative recovery, the patient aims for pain management, dietary changes, and recovery monitoring. She took ondansetron, loperamide, and morphine to treat her discomfort postoperatively. A tolerable diet was supplied to ensure adequate nutrition to reduce surgical complications and overburden the digestive system. Five days post-surgery, the patient was stable and demonstrated a functioning colostomy. She was able to tolerate a soft diet. Her physical examination showed a non-tender abdomen and no acute sign of infection or inflammation. The patient was cleared to go back to her assigned nursing home. She was scheduled for outpatient follow-up and future colon resection for treatment of her RVF pending her cancer treatment.
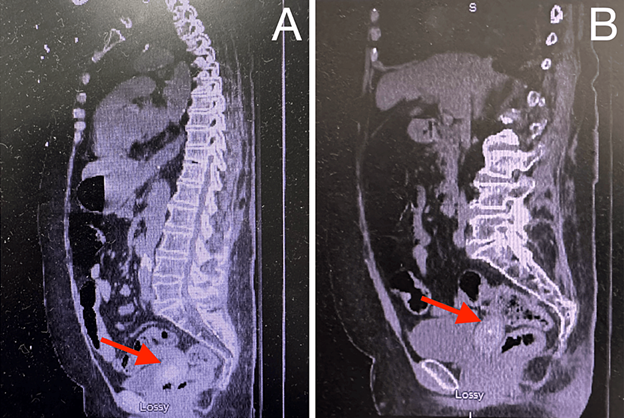
Figure 1: CT scan of the abdomen eight months before presentation, sagittal sections A and B.
CT scan of the patient eight months before presentation during her initial work-up for her ovarian cancer. The red arrows in Figures 1A and 1B showed a normal-appearing uterus without any air in the lumen and no apparent fistula. There was also persistent hyperdense material within the endometrial cavity, with subtle lucencies that likely represented a stable ongoing mass, as per radiological reports.
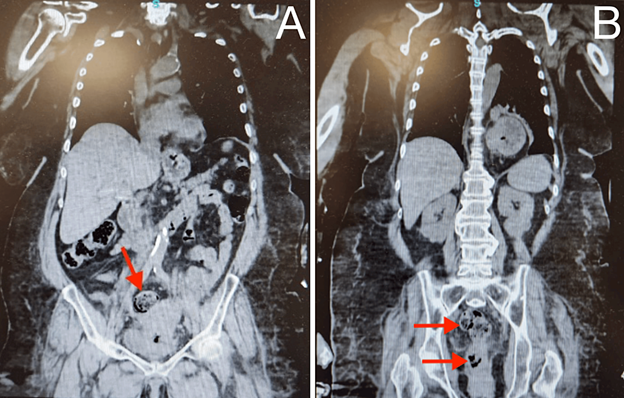
Figure 2: Preoperative CT scan of the abdomen, coronal sections A and B.
A. red arrow indicates air within the lumen of the vagina (black areas within the lumen), and B. red arrows demonstrate the air within the vagina (top arrow) and vaginal canal (bottom arrow). The vagina was distended and filled with stool. These findings suggested a rectovaginal fistula.
Discussion
Managing RVFs necessitates carefully considering several variables that have an impact on surgical results, especially in patients with complicated medical histories. This case study highlights several crucial elements of RVF management. Using laparoscopic methods aligns with the latest developments in colorectal surgery. Compared to open procedures, these minimally invasive techniques have the advantages of less postoperative pain, a decreased chance of wound complications, and a quicker recovery. In a study by Kamaran et al., the laparoscopic approach to repairing and managing RVF offered all the benefits of minimal access surgery, including superior postoperative outcomes [7]. Our case illustrates these goals clearly. The laparoscopically assisted loop transverse colostomy successfully diverts the fecal stream, which is an essential step in enabling the RVF site to heal [1].
Second, this case emphasizes how crucial customized management plans are. The surgical approach and postoperative care were heavily impacted by the patient's medical history, which included COPD and ovarian cancer. The concepts of patient-centered care in surgical practice are aligned with this individualized approach, which is essential for enhancing patient outcomes. A comprehensive approach to the patient's care, treating the fistula and her general health, was made possible by the multidisciplinary therapy comprising oncologists, pulmonologists, and pain management specialists [8].
The way this patient was managed after surgery also emphasizes how critical it is to take care of the patient's nutritional requirements and pain management during the healing period. In patients with preexisting respiratory disorders such as COPD, effective pain management is essential for improving patient comfort, encouraging early mobilization, and preventing consequences such as deep vein thrombosis or pulmonary complications [9]. Furthermore, nutritional support, usually an undervalued aspect of post-operative care, is essential for wound healing and subsequent recovery, especially for patients whose underlying illnesses or the side effects of their treatments may have affected their nutritional status [4]. Considering a patient's food consumption and its impact can suggest underlying pathology influencing their mental and physical health. Hence, nutritional levels may impact mental and physical symptoms and affect a patient's recovery.
In addition, people living with comorbidities often have increased levels of anxiety and depression and experience isolation and a lack of social support. In a study by Wilson et al., patients were interviewed and asked if they thought their fistulas were cured. The patients who reported leakage declared higher levels of PTSD and depressive symptoms compared to those who were identified as cured [10]. Hence, further longitudinal studies on the influence of the mental health status of RVF patients postoperatively should be conducted.
Conclusion
RVFs are clinically challenging to diagnose and manage, and they are distressing and complicated conditions that can affect the quality of life. Surgery is often required to resolve the RVFs, and selecting a surgical method is influenced by the patient’s current needs. This patient, a 67-year-old woman with a history of anxiety, depression, COPD, and ovarian cancer who presented with a confirmed rectovaginal fistula clinically and radiologically, was successfully managed laparoscopically, using a diagnostic laparoscopy, a laparoscopic adhesiolysis, and a laparoscopic loop transverse colostomy. This case adds to the expanding body of research supporting a patient-centered, comprehensive strategy to manage RVFs. It emphasizes the value of a multidisciplinary team in caring for patients with complicated medical histories and the efficacy of laparoscopic procedures in challenging surgical situations. Subsequent investigations and clinical applications ought to persist in propelling minimally invasive management forward and crafting all-encompassing care plans that consider the individual needs of every patient.
Author Contributions: All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Concept and design: Martin D. Tanhaei, Muresuk Mena, Frederick Tiesenga
Acquisition, analysis, or interpretation of data: Martin D. Tanhaei, Naga P. Reddy-MalluDrafting of the manuscript: Martin D. Tanhaei, Muresuk Mena, Naga P. Reddy-Mallu, Frederick Tiesenga
Critical review of the manuscript for important intellectual content: Martin D. Tanhaei, Muresuk Mena, Frederick Tiesenga
Supervision: Martin D. Tanhaei, Frederick Tiesenga
Disclosures
Disclosures Human subjects: Consent was obtained or waived by all participants in this study. Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Acknowledgements: Special thanks to the dedicated work of general surgeons, Frederick M. Tiesenga, MD, Juaquito M. Jorge, MD (on-call surgeon), and Deepa Patel, MD (on-call surgeon), whose expertise was fundamental in this case. Additional thanks to our editor doctors for their insightful edits, enriched by their multidisciplinary expertise, Talieh Norouzi MD, Mehdi Tanhaei MD, and Maryam Ghaemi DDS."
References
- Kniery KR, Johnson EK, Steele SR. Operative considerations for rectovaginal fistulas. World Journal of Gastrointestinal Surgery, 2015; 7: 133-137.
- Tracy LH, Michael AV. Rectovaginal fistula. Keighley & Williams' Surgery of the Anus, Rectum and Colon. CRC Press (ed), 2018. https://doi.org/10.1201/9781351105040: 251-253.
- Das B, Snyder M. Rectovaginal Fistulae. Clinics in Colon and Rectal Surgery, 2016; 50-56. doi: 1055/s-0035-1570393
- Kobayashi H, Sugihara K. Successful management of rectovaginal fistula treated by endorectal advancement flap: report of two cases and literature review. SpringerPlus, 2015; 1186: 40064-015.
- Buchs NC, Gervaz P, Secic M, et al. Incidence, consequences, and risk factors for anastomotic dehiscence after colorectal surgery: a prospective monocentric study. International Journal of Colorectal Disease, 2008; 23: 265-270.
- Tsang CB, Madoff RD, Wong WD, et al. Anal sphincter integrity and function influences outcome in rectovaginal fistula repair. Diseases of the Colon and Rectum, 1998; 41: 1141-1146.
- Kumaran SS, Palanivelu C, Kavalakat AJ, et al. Laparoscopic repair of high rectovaginal fistula: is it technically feasible?. BMC Surgery, 2005; 5: 20.
- Drumond DG, Condé CMS, Chebli JMDF, et al. Combined clinical and radiological remission of rectovaginal fistulas using fractional CO2 vaginal laser: a case series and medium-term follow-up. BMC Research Notes, 2023; 16: 371-410.
- Licker M, Schweizer A, Ellenberger C, et al. Perioperative medical management of patients with COPD. International Journal of Chronic Obstructive Pulmonary Disease, 2: 493-515.
- Wilson SM, Sikkema KJ, Watt MH, et al. Psychological Symptoms and Social Functioning Following Repair of Obstetric Fistula in a Low-Income Setting. Maternal and Child Health Journal, 2016; 20: 941-945.

