Cystic Dilatations of the Bile Ducts: Differential Diagnosis of Hydatid Cyst of the Liver
Bachar A, Azhari F, Benzidane K*, Elabbassi T and Lefriyekh R
Department of Medicine, Faculty of Medicine and Pharmacy of Casablanca, Morocco
Received Date: 03/01/2024; Published Date: 16/05/2024
*Corresponding author: Benzidane K, Department of Medicine, Faculty of Medicine and Pharmacy of Casablanca, Morocco
Abstract
Liver hydatid cyst has many differential diagnoses that require a cautious surgical approach. The congenital cystic dilatations of the common bile duct are one of them and they represent the most common congenital disorder of the biliary tree. this multitude of differential diagnosis explains the need to carry out a radiological examination which may include a CT scan, ERCP or magnetic resonance cholangiopancreatography to better characterize the lesion and for a better surgical approach.
We report in this article the observation of 2 patients admitted for a hydatid cyst of the liver with as intraoperative diagnosis a cystic dilation of the convergence of the two hepatic ducts and the second one, a biliary cyst.
Keywords: Liver hydatid cyst; Differential diagnoses; Congenital cystic dilatations of the common bile duct; Biliary cyst; Classification of these dilations is that of TODANI
Introduction
Congenital cystic dilatations of the common bile duct are rare malformations of the bile ducts, which are characterized by one or more communicating cystic dilatations of the bile ducts [1]. They represent the most common congenital disorder of the biliary tree preceded by biliary atresia [2].
Their diagnosis is based on ultrasound and Bili-MRI with a definitive diagnosis intraoperatively. The most widely used classification of these dilations is that of TODANI, which is interested in both intra and extra haptic damage, unlike that of ALONSO-LEJ.
The early diagnosis and proper treatment are very important, because biliary cyst (BC) is associated with a risk of carcinogenesis. According to the literature, biliary tract malignancy occurs in 2.5% - 28% of patients with BC [3,4].
However, the management of a hepatobiliary cyst should always be extremely cautious. the differential diagnoses are multiple, ranging from a hydatid cyst, Congenital cystic dilatations of the common bile duct, benign adenoma, focal nodular hyperplasia, metastatic lesion, biliary cystadenoma or cystadenocarcinoma, primary hepatoma, pyogenic or amebic abscess.
We report in this article the observation of 2 patients admitted for a hydatid cyst of the liver with as intraoperative diagnosis a cystic dilation of the convergence of the two hepatic ducts and the second one, a biliary cyst.
Observation
First observation:
A 32-year-old patient, with no pathological history, reported contact with dogs. The symptomatology was intermittent and dated back to 10 years, characterized by the onset of pains in the right hypochondrium in the form of heaviness, not radiating, associated with generalized cutaneo-mucous jaundice with cholestasis, without other associated signs, all evolving in the context of a well-preserved general condition.
During the clinical examination, the patient was conscious, in good general condition, with normo-colored conjunctivae. Abdominal examination revealed slight tenderness, with no palpable mass, hepato-splenomegaly, and pelvic abnormalities.
In September 2014, the patient underwent an abdominal CT showing a liver of normal size, regular contours, hosting a rounded oval formation. This formation was well-limited, hypodense, heterogeneous, not enhanced after the injection of contrast product, compressing the biliary convergence with discreet dilation of the bile ducts upstream. It measured 63 x 40 mm. In conclusion: CT appearance suggestive of a type IV hepatic hydatid cyst (Figure 1).
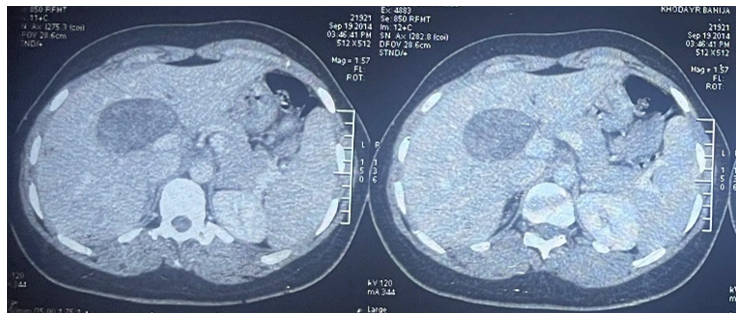
Figure 1: CT scan showed a type IV hepatic hydatid cyst.
A hepatic MRI performed in December 2019 showed a liver of normal size, with regular outlines. At the segment IV level, there was a roughly oval, well-limited cystic formation with a T1 and T2 isosignal content, discreet hypersignal diffusion with intermediate ADC, not enhanced after the injection of Gadolinium. It measured 67x45 mm, extending to 64.4 mm. This formation came into intimate contact with the portal trunk and the common bile duct, which were of normal caliber with no detectable endoluminal material. In conclusion, MRI appearance suggestive of a hepatic hydatid cyst (Figure 2).
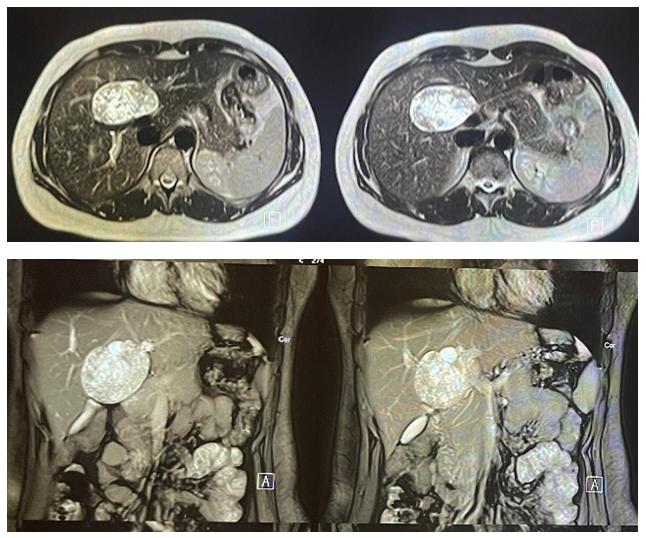
Figure 2: MRI image of the hepatic hydatid cyst.
Upon admission to the department, the patient underwent an abdominal CT scan with the following results: Liver of normal size, regular contours, situated straddling segments IV, V, and VIII with a roughly oval formation, bumpy contours in places, heterodense, not enhanced after the injection of contrast agent, site of calcifications, measuring 75×48 mm, spread over 64.4 mm (compared to 67×45 mm, spread over 64.4 mm). This formation exerts a mass effect on biliary convergence with dilation of the right and left proximal intrahepatic bile ducts. It pushes back the right and left portal branches, which are laminated but nevertheless remain permeable.
With echographic complement: This formation is well-limited, with regular contours, echogenic, delimiting small cystic cells, not vascularized with the color Doppler, and site of calcifications. In conclusion: CT appearance suggestive of a type IV hepatic hydatid cyst, having slightly increased in volume (Figure 3).
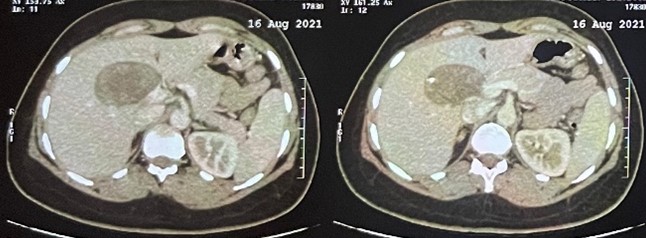
Figure 3: CT scan image of a type IV hepatic hydatid cyst.
On the biological assessment:
- AST: 22 IU/L ALT: 24 IU/L
- Gamma-glutamyl transferase: 19 IU/L; alkaline phosphatase: 38 IU/L
- Total bilirubin: 7.1 mg/L; conjugated bilirubin: 2.7 mg/L; conjugated bilirubin: 4.4 mg/L
- Hydatid serology: negative
The patient underwent surgery, and upon exploration: Figure 4
- Absence of peritoneal effusion.
- Presence of a cystic mass, measuring 6 cm, affecting the biliary convergence, and its puncture yielded bile. Dissection of the mass and tracking of the bile duct were performed until the retro-duodenal area. The common bile duct was of normal caliber, and the gallbladder had thin walls.
Faced with this aspect, the decision was therapeutic abstention with the intention of further exploration.
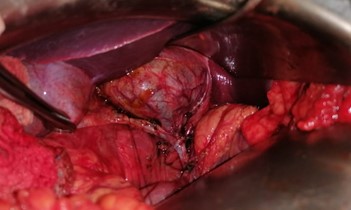
Figure 4: intraoperative image showing a dilatation of the convergence of the common bile duct.
A hepatic MRI was performed postoperatively with the result: liver of normal volume, regular contours, homogeneous signal, site at the level of segments IV and V of a well-limited formation, oval, with a very heterogeneous signal, mainly in T2 hypersignal, and T1 hyposignal with spots in T1 hypersignal, not enhanced after injection of contrast product. It measures: 6.3 × 4.5 x 6.0 cm. This formation is in intimate contact with the main trunk and its branches, which remain permeable, with no detectable signs of invasion. It pushes back the biliary convergence and the main bile duct without dilation of the CBD or of the intrahepatic bile ducts. Posteriorly, it comes into contact with the inferior vena cava which is of normal caliber and permeable. Below it comes into contact with the vesicular infundibulum, the pancreatic head and the duodenum. With echographic complement: well limited oval formation of heterogeneous echogenicity.
A postoperative hepatic MRI was conducted with the following result: The liver had a normal volume, regular contours, and homogeneous signal. At the level of segments IV and V, there was a well-defined, oval formation with a highly heterogeneous signal, predominantly showing T2 hypersignal and T1 hyposignal with spots in T1 hypersignal. The formation did not enhance after the injection of contrast product and measured 6.3 × 4.5 x 6.0 cm. This formation was in intimate contact with the main trunk and its branches, which remained permeable, with no detectable signs of invasion. It pushed back the biliary convergence and the main bile duct without dilation of the common bile duct (CBD) or the intrahepatic bile ducts. Posteriorly, it came into contact with the inferior vena cava, which was of normal caliber and permeable. Below, it came into contact with the vesicular infundibulum, the pancreatic head, and the duodenum. With echographic complement: a well-limited oval formation of heterogeneous echogenicity (Figure 5).
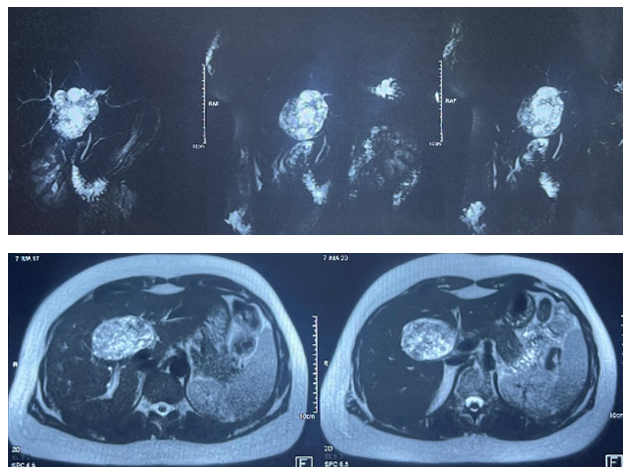
Figure 5
Second observation:
63-year-old patient, operated 2 months before admission for a pulmonary hydatid cyst. The symptoms dated back 6 months, w characterized by the onset of pains in the right hypochondrium in the form of heaviness, without any other associated sign, all evolving in the context of a well-preserved general condition.
On clinical examination, we found a conscious patient in good general condition with normal-colored conjunctivae. During abdominal examination, there was tenderness in the right hypochondrium, and hepatomegaly was observed with a hepatic span of 17 cm. There was no splenomegaly, and pelvic examinations showed no abnormalities.
The patient underwent an abdominal CT scan in January 2023, revealing an enlarged liver with a right hepatic span of 19 cm. The liver exhibited multiple cystic formations of variable sizes, both isolated and grouped in clusters. These formations had fluid content, without wall thickening, calcifications, or solid bud images. The largest among them was an agglomerate in the left liver measuring 84x47 mm, and a cyst in segment VI measuring 64x47 mm. The kidneys measured 110x49 mm on the right and 110x52 mm on the left, appearing homogeneous with notably no cystic images. A discreet postero-superior cortical notch was noted with discreet infiltration of neighboring fat in contact with the reaction-like diaphragm. There was no dilation of the intra- and extra-hepatic bile ducts. In conclusion, the aspect favored a diagnosis of isolated polycystic liver disease.
Absence of dilation of the right and left VBIH. Absence of dilatation of the VBP (measuring 4.3 mm). Gallbladder not distended, appears to have homogeneous contents. Kidneys of normal size, with regular contours, well differentiated, without dilation of the excretory cavities, sites of several subcentimetric bilateral renal cysts. In conclusion, MRI appearance of multiple diffuse cystic hepatic lesions: hydatid cysts? simple biliary cysts? Bilateral renal cysts: simple cortical cysts (Bosniak I)? locations of hydatid cysts?
A hepatic Bili-MRI performed in May 2023 showed an increased liver volume (20 cm) with bumpy contours, exhibiting multiple cystic formations involving all segments, predominantly in the left liver. These formations were confluent in some areas, with thin walls and showed no enhancement after the injection of Gadolinium. The largest cysts were located as follows:
- Segment II: 79x37 mm, extending to 60.8 mm
- Straddling segments VII and VIII: 55x40 mm, extending over 50 mm.
- Segment VI: 40x36.8 mm
There was no dilation of the right and left intrahepatic bile ducts. The common bile duct was not dilated (measuring 4.3 mm). The gallbladder, not distended, appeared to have homogeneous contents. The kidneys were of normal size, with regular contours, well-differentiated, without dilation of the excretory cavities, and showed several subcentimetric bilateral renal cysts.
In conclusion, the MRI appearance suggested multiple diffuse cystic hepatic lesions, raising questions about the possibility of hydatid cysts, simple biliary cysts, or bilateral renal cysts (simple cortical cysts, Bosniak I). The locations of hydatid cysts were also considered (Figure 6).
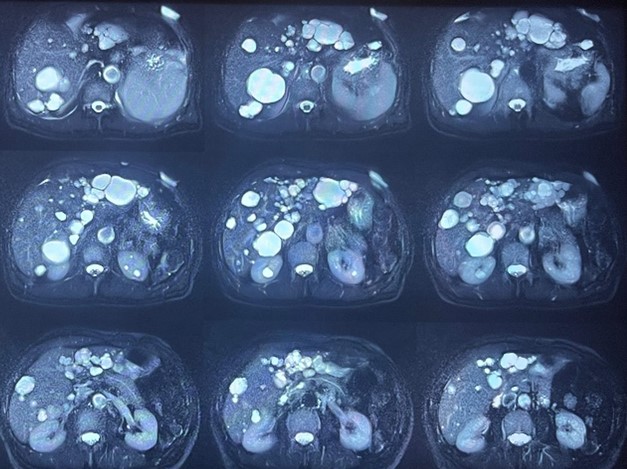
Figure 6
On the biological assessment:
- AST: 14 IU/L ALT: 09 IU/L
- Gamma-glutamyl transferase: 13 IU/L; alkaline phosphatase: 71 IU/L
- Total bilirubin: 2.8 mg/L; conjugated bilirubin: 1 mg/L; conjugated bilirubin: 1.8 mg/L
- Hydatid serology: negative
The patient underwent surgery having benefited from fenestration of several hepatic cysts with exploration: (Figure 7)
- Absence of peritoneal effusion
- Liver riddled with cysts with serous content. Presence of a whitish lesion at segment IV (biopsy done).

Figure 7: Intraoperative image showing the liver riddled with cysts with serous content.
Discussion
It is the second leading cause of congenital malformation of the biliary tract after biliary atresia [5]. They are usually a surgical problem of infancy or childhood; however, in approximately 20% of cases they are recognized in adults [6].
Many theories explain the etiology and pathogenesis of BC. Yotsuyanagi supposed that BC arouse from inequality in the cellular proliferation of the biliary tract during the early fetal life [7].
Babbitts’s theory of the “common channel” is the most widely accepted in the literature. According to this theory, the common cannel is formed by abnormal pancreaticobiliary junction (APBJ) of the pancreatic and bile ducts outside the ampulla of Vater. This condition leads to pancreaticobiliary reflux and mixing of the pancreatic and biliary juices and activations of pancreatic enzymes, because the maximal pressure within the pancreatic duct is two to three timed higher than within a biliary tract. Activated pancreatic enzymes cause inflammation and deterioration of the bile duct wall that leads to biliary dilatation [8]. A number of studies analyzed the levels of amylase within the bile duct. The higher amylase concentrations have been observed in patients with BC compared to the control groups. Also, association between the amylase level, earlier presentation and dysplasia grade in patients with BC has been reported in the literature [9,10].
APBJ occurs only in 50%-80% patients with BC. Another counterargument to this hypothesis is a fact, that immature neonatal acini do not produce sufficient pancreatic enzymes to explain antenatal BC [11-13].
According to Singham et al, biliary dilation can be a result of embryologic overproliferation of epithelial cells within solid bile ducts during the fetal life [11].
According to Davenport and Basu, dilations are due to a lower number of neurons and ganglions in patients with BC that have been recognized pathologically. They suggested that round
cysts were congenital with distal obstruction due to aganglionosis and proximal dilation similarly to Hirschprung’s disease. In this theory, chronic inflammation and clinical manifestation are caused by bile stasis within dilated bile ducts [11,13,14].
According to the literature, biliary tract malignancy occurs in 2.5%-28% of patients with BC [3,4]. The risk of biliary cancer increases with the age. It is the lowest in the childhood in the first decade (< 1%) [15]. In the third decade the cancer risk is > 10% [16,17]. According to the literature, cholangiocarcinoma is reported the most frequently at the age of 32 years in patients with BC (about 20 years earlier than in general population) [16]. There are reports of cholangiocarcinoma developing in adult many years after radical BC resection in infant [18]. Cholangiocarcinoma is the most serious and dangerous BC complication. The other complications associated with BC involve cholelithiasis and hepatolithiasis, cholangitis, acute and chronic pancreatitis, portal hypertension, liver fibrosis and secondary liver cirrhosis and spontaneous cyst perforation [17,19].
The triad pain, jaundice, mass classically evokes a cystic dilation of the bile ducts but it was never found complete. In most cases, imagery can make the diagnosis, especially in types I, IV, and V [20].
For imaging modalities that can be used, abdominal ultrasonography (US) is in first intension, to explore with sensitivity ranging from 71% to 97% and in addition for follow-up surveillance [21,22]. But if distal common bile duct is not visualized due to bowel gas, or overlying structures, CT is required. CT is useful in showing part that US is not able to show, like continuity of the cyst in intrahepatic bile ducts, distal bile duct, and pancreatic head [23].
The ERCP has in addition, therapeutic possibility but it still an invasive process and its sensitivity and quality of images is dependent for operation [24].
Magnetic resonance cholangiopancreatography with her noninvasive and no complications characteristics, beside of that having 90%–100% sensitivity and avoids ionizing radiation make it the gold standard of diagnosis [25,26].
Surgery is the treatment of BC. The goal of surgical treatment is to remove a cyst and to reconstruct the proper bile flow to the alimentary tract. In order to achieve this goal, different techniques are used. Roux-Y hepaticojejunostomy is the method of choice in most patients with BC [27,28].
JA Calvo-Ponce et al. propose introducing a variant as type Id in Todani’s Modified Classification of biliary duct cysts so it includes every type of cystic dilatation described as well as their surgical treatment [29].
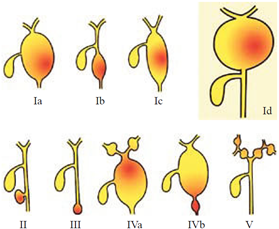
Figure 8: Todani’s Modified Classification of biliary duct cysts 29.
Conclusion
Hydatid disease is an endemic problem in many parts of the world. Despite attempts to identify imaging findings that distinguish hepatic echinococcal cysts from other hepatic cystic lesions, echinococcosis is still a challenging disease to diagnose radiographically. This case of hydatid cyst in the liver revealing during surgery other lesions, emphasizes the importance of taking precautions when exploring a hepatobiliary cyst, its anatomical relationships and its contents by needle puncture.
References
- Mercadier M, Chigot JP, Clot JP, Langlois P, Lansiaux P. Caroli disease. World J Surg, 1984; 8: 22–29.
- Kianmanesh R, Régimbeau JM, Belghiti J. Anomalies de la jonction biliopancréatique et dilatations kystiques congénitales des voies biliaires. J Chir (Paris), 2001; 138(4): 196–204.
- Jan YY, Chen HM, Chen MF. Malignancy in choledochal cysts. Hepatogastroenterology, 2000; 47: 337-340.
- Bloustein PA. Association of carcinoma with congenital cystic conditions of the liver and bile ducts. Am J Gastroenterol 1977; 67: 40-46
- Kianmanesh R, Régimbeau JM, Belghiti J. Anomalies de la junction biliopancréatique et dilatations kystiques congénitales des voies biliaires. J Chir (Paris), 2001; 138(4): 196–204.
- Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: part 1 of 3: classification and pathogenesis. Can J Surg, 2009; 52: 434-440.
- Yotsuyanagi S. Contributions to etiology and pathogeny of idiopathic cystic dilatation of the common bile duct with report of three cases: new etiological theory based on supposed inequal epithelial proliferation at the stage of physiological epithelial occlusion of primitive choledochus. Gan, 1936; 30: 601-650.
- Babbitt DP. [Congenital choledochal cysts: new etiological concept based on anomalous relationships of the common bile duct and pancreatic bulb]. Ann Radiol (Paris), 1969; 12: 231-240.
- Sugiyama M, Haradome H, Takahara T, Izumisato Y, Abe N, Masaki T, et al. Biliopancreatic reflux via anomalous pancreaticobiliary junction. Surgery, 2004; 135: 457-459.
- Todani T, Narusue M, Watanabe Y, Tabuchi K, Okajima K. Management of congenital choledochal cyst with intrahepatic involvement. Ann Surg, 1978; 187: 272-280.
- Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: part 1 of 3: classification and pathogenesis. Can J Surg, 2009; 52: 434-440.
- Imazu M, Iwai N, Tokiwa K, Shimotake T, Kimura O, Ono S. Factors of biliary carcinogenesis in choledochal cysts. Eur J Pediatr Surg, 2001; 11: 24-27.
- Hosoki T, Hasuike Y, Takeda Y, Michita T, Watanabe Y, Sakamori R, et al. Visualization of pancreaticobiliary reflux in anomalous pancreaticobiliary junction by secretin-stimulated dynamic magnetic resonance cholangiopancreatography. Acta Radiol, 2004; 45: 375-382.
- Davenport M, Basu R. Under pressure: choledochal malformation manometry. J Pediatr Surg, 2005; 40: 331-335.
- Clifton MS, Goldstein RB, Slavotinek A, Norton ME, Lee H, Farrell J, et al. Prenatal diagnosis of familial type I choledochal cyst. Pediatrics, 2006; 117: e596-e600.
- Søreide K, Søreide JA. Bile duct cyst as precursor to biliary tract cancer. Ann Surg Oncol, 2007; 14: 1200-1211.
- Benjamin IS. Biliary cystic disease: the risk of cancer. J Hepatobiliary Pancreat Surg, 2003; 10: 335-339.
- Nicholl M, Pitt HA, Wolf P, Cooney J, Kalayoglu M, Shilyansky J, et al. Choledochal cysts in western adults: complexities compared to children. J Gastrointest Surg, 2004; 8: 245-252.
- Saluja SS, Nayeem M, Sharma BC, Bora G, Mishra PK. Management of choledochal cysts and their complications. Am Surg, 2012; 78: 284-290.
- Vullierme MP, Vilgrain V, Zins M, et al. Dilatations kystiques congénitales de la voie biliaire principale. Gastroenterol Clin Biol, 1997; 21: 201–208
- Tsuchida A, Nagakawa Y, Kasuya K, et al. Computed tomography virtual endoscopy with angiographic imaging for the treatment of type IV-A choledochal cyst. World J Gastroenterol, 2012; 18(28): 3761–3764.
- Haliloglu M, Akata D, Gurel S, Ozmen MN, Akhan O. Choledochal cysts in children: evaluation with three-dimensional sonography. J Clin Ultrasound JCU, 2003; 31(9): 478–480.
- Jablonska B. Biliary cysts: etiology, diagnosis and management. World J Gastroenterol, 2012; 18(35): 4801–4810.
- Arshanskiy Y, Vyas PK. Type IV choledochal cyst presenting with obstructive jaundice: role of MR cholangiopancreatography in preoperative evaluation. AJR Am J Roentgenol, 1998; 171(2): 457–459.
- Kim MJ, Han SJ, Yoon CS, et al. Using MR cholangiopancreatography to reveal anomalous pancreaticobiliary ductal union in infants and children with choledochal cysts. AJR Am J Roentgenol, 2002; 179(1): 209–214.
- Park DH, Kim MH, Lee SK, et al. Can MRCP replace the diagnostic role of ERCP for patients with choledochal cysts? Gastrointest Endosc, 2005; 62(3): 360–366.
- Tan SS, Tan NC, Ibrahim S, Tay KH. Management of adult choledochal cyst. Singapore Med J, 2007; 48: 524-527.
- Katyal D, Lees GM. Choledochal cysts: a retrospective review of 28 patients and a review of the literature. Can J Surg, 1992; 35: 584-588.
- Jorge A Calvo-Ponce, Rafael V Reyes-Richa, Homero A Rodríguez Zentner. Cyst of the common hepatic duct: Treatment and proposal for a modification of Todani’s classification. Annals of Hepatology, 2008; 7(1): 80-82.

