Peritoneal Hydatidosis Complicating a Splenic Ruptured Hydatid Cyst
Jidal M*, Horache K, El Haddad S, Allali N and Chat I
Radiology department, Children’s hospital, Mohammed V university, Rabat, Morocco
Received Date: 12/12/2023; Published Date: 09/05/2024
*Corresponding author: Manal JIDAL, Radiologydepartment, Children’s hospital, Mohammed V University of Rabat, Morocco
Abstract
Hydatid cyst, a zoonotic infection prevalent in Mediterranean countries, typically affects the liver and lungs but can involve other organs, including the spleen. This article presents a case study of a 10-year-old child with a ruptured splenic hydatid cyst leading to peritoneal dissemination. This case emphasizes the significance of prompt recognition and management in splenic hydatidosis, facilitating improved patient outcomes.
Keywords: Hydatid cyst; Rupture; Peritoneal hydatidosis; CT
Introduction
Hydatid cyst is a zoonosis frequently found in several endemic countries around the Mediterranean basin. Although it most commonly affects the liver and lungs, other organs can be involved, such as the spleen in 0.9 to 8% of cases [1]. The severity of this condition is closely related to its complications, namely bacterial superinfection and rupture. The latter constitutes a real emergency and a transition stage towards peritoneal hydatidosis.
Clinical Observation
This involves a 10-year-old child living in a rural area with no medical history, presenting to the clinic with left hypochondrial pain. During the medical history, there is a mention of abdominal trauma a few months earlier. Clinical examination reveals slight tenderness on palpation of the left hypochondrium without other associated signs. Ultrasound shows the presence of a roughly oval-shaped formation with pure anechoic content, irregular wall, containing calcifications, and discontinuous in some places, communicating the cyst content with the peritoneal cavity. It is associated with a moderate amount of peritoneal effusion. Complementary CT scan highlights the previously described splenic cyst and abdominal effusion (Figure 1a and 1b). Additionally, in the pelvic area, on the right lateral-vesical side, two roughly rounded formations with thick walls and liquid density content are found (Figure 2a and 2b). All of this is indicative of a ruptured splenic hydatid cyst with peritoneal dissemination. The patient underwent surgical treatment with splenectomy, resection of peritoneal cysts, abundant peritoneal lavage, and adjunctive medical treatment with albendazole.
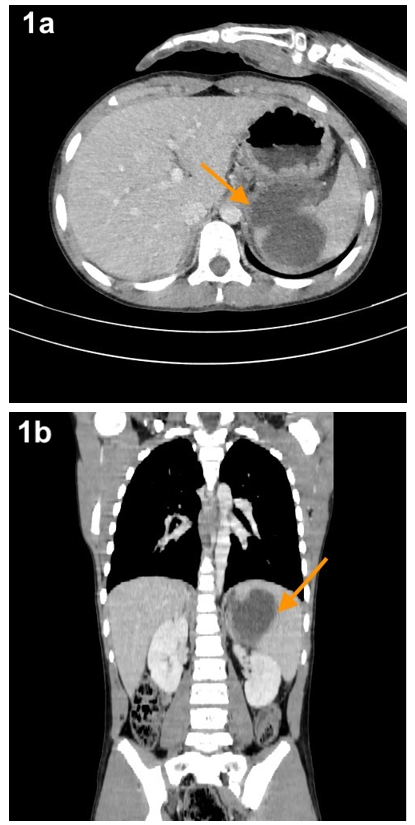
Figure 1: Axial (a) and coronal (b) views of an abdominopelvic CT scan with contrast injection, revealing a splenic cyst with discontinuous wall in some areas, allowing communication between the cyst content and the peritoneal cavity.

Figure 2: Axial sections (a and b) showing two cystic formations with thick walls in the pelvic region, indicative of peritoneal infection and dissemination of Echinococcus granulosus. This is referred to as cystic peritoneal echinococcosis.
Discussion
The spleen is the third organ most affected by Echinococcus granulosus after the liver and lungs. Splenic cysts tend to gradually increase in size, making the organ more vulnerable to abdominal trauma. Rupture of these cysts into the abdominal cavity is a rare complication. It can occur spontaneously or following abdominal trauma, and the risk increases with the size of the cyst and intra-cystic pressure. Some authors consider young age and the superficial position of the cyst as predictive factors [2,3]. Clinically, this manifests as abdominal pain, nausea, vomiting, and allergic symptoms ranging from simple urticaria, itching, asthmatic dyspnea to anaphylactic shock [3,4]. Imaging is essential for diagnosis and early management. Ultrasound reveals variable amounts of peritoneal effusion and the splenic cyst with a clean wall, anechoic liquid content, with or without septations and calcifications. CT has better specificity, allowing a better characterization of the cyst by studying its content and wall. It is liquid-filled, with a thickened wall, sometimes containing calcifications, fenestrated or discontinuous in places, communicating the liquid content of the cyst with the peritoneum. The CT scan also specifies the location of the lesion and explores the rest of the abdominal cavity for liquid effusion or other locations of this condition, specifically intraperitoneal cysts suggesting dissemination in the abdominal cavity. This is called encapsulated peritoneal hydatidosis [3,4].
The treatment is surgical, involving abundant lavage of the peritoneal cavity, cyst resection, and adjuvant medical treatment, typically with albendazole, administered in 15-day cycles for a duration of 6 months [5]. Follow-up ultrasound after the procedure is useful to detect potential recurrence or complications.
Conclusion
Splenic localization of hydatid cyst is relatively rare, and one of its most dreaded complications is its rupture into the peritoneal cavity. Ultrasound and CT imaging allow for diagnosis and assessment of the extent of lesions to guide the clinician and enable prompt patient management.
Conflicts of Interest: None
References
- Pedrosa I, Saíz A, Arrazola J, Ferreirós J, Pedrosa CS. Hydatid disease: radiologic and pathologic features and complications. Radiographics, 2000; 20(3): 795-817. doi: 10.1148/radiographics.20.3.g00ma06795.
- Mouaqit O, Hibatallah A, Oussaden A, Maazaz K, Taleb KA. Acute intraperitoneal rupture of hydatid cysts: a surgical experience with 14 cases. World J Emerg Surg, 2013; 8: 28. doi: 10.1186/1749-7922-8-28.
- Toumi O, Noomen F, Salem R, Rabeh H, Jabra SB, Korbi I, et al. Intraperitoneal rupture of hydatid cysts. Eur J Trauma Emerg Surg, 2017; 43(3): 387-391. doi: 10.1007/s00068-016-0662-9.
- Ozlem N. Traumatic rupture of a splenic cyst hydatid. Int J Surg Case Rep, 2015; 7C: 112-114. doi: 10.1016/j.ijscr.2014.10.092.
- Rao SB, Madi DR, Shetty AK. A cystic splenic mass in a farmer. European Journal of Internal Medicine, 2017; 46: e5–e6. doi: 10.1016/j.ejim.2017.04.024

