The Role of Exploratory Laparoscopy in the Diagnosis and Management of Pancreatic Masses: A Case Report and Review of the Literature
Shaniah S Holder1,*, Ehizele Itama1, Abigail R Greaves1, Alaerebo Malvan-Iyalla1 and Frederick Tiesenga2
1Department of Medicine, American University of Barbados School of Medicine, Barbados
2Department of Surgery, Community First Hospital, USA
Received Date: 20/12/2023; Published Date: 03/05/2024
*Corresponding author: Shaniah Holder, Department of Medicine, American University of Barbados School of Medicine, Barbados
Abstract
Pancreatic cancer has a large global effect due to its aggressive nature and typically late-stage detection. Pancreatic masses pose a diagnostic and therapeutic challenge due to their complex nature and potential for malignancy. Laparoscopy, as a minimally invasive surgical approach, has emerged as an important tool in a surgeon's toolkit, providing several advantages over traditional open methods. The diagnostic usefulness of laparoscopy in pancreatic masses stems from its ability to offer a direct view of the pancreas and allow the exact evaluation of the tumor features. Laparoscopy also allows for tissue sample collection, which aids in histological diagnosis. This report describes the case of a 54-year-old female who had radiologic evidence of a pancreatic mass. Percutaneous biopsy was nondiagnostic resulting in the need for laparoscopic evaluation which yielded histological results that confirmed the diagnosis of pancreatic adenocarcinoma. This article aims to explore the procedure that is laparoscopy and its benefits in the evaluation of pancreatic masses.
Keywords: Pancreatic Cancer; Pancreatic Mass; Laparoscopic Biopsy; Percutaneous biopsy
Introduction
Pancreatic cancer is rare and serious and accounts for about 3% of cancer diagnoses, 7% of cancer-related deaths in the United States, and a poor five-year survival rate [1,2]. Environmental influences such as smoking, chronic pancreatitis, and gene mutations have been associated with an increased risk for the development of pancreatic cancer. They are usually classified into exocrine and endocrine pancreatic cancers with the most common type being pancreatic ductal adenocarcinoma. Early detection of this cancer is difficult, and symptoms are usually presented at an advanced stage which results in a lower long-term survival rate compared to other cancers [3].
The location of the tumor can affect the symptomatic presentation. Tumors in the head of the pancreas cause painless jaundice while abdominal pain radiating to the back and weight loss are seen in tumors of the pancreatic body or tail [3]. Other common symptoms include loss of appetite, new-onset diabetes, itchy skin, and blood clots. In addition to the medical history and physical exam, imaging, blood tests, and biopsy can aid in the diagnosis of pancreatic cancer. Multi-detector row computed tomography (MDCT) is considered the best diagnostic imaging modality for the evaluation of pancreatic cancer [2]. A commonly known tumor marker for diagnoses is the carbohydrate antigen 19-9 (CA 19-9), however, it has a low specificity [4].
Different methods of biopsies can be employed, such as percutaneous, endoscopic, or surgical. Recent literature has explored the role of laparoscopy in the evaluation and management of pancreatic cancer. It is an easy procedure that allows the collection of biopsies, identifying unresectable cases, and further decreasing the number of unnecessary diagnostic procedures [4]. Laparoscopic biopsy can be done to identify certain mutations, such as BRCA or NTRK genes that aid in creating targeted therapy drugs for cancer treatment [5].
In this case, we present a patient who had a history of abdominal pain and weight loss with a pancreatic body and tail tumor found on CT of the abdomen. After a nondiagnostic percutaneous biopsy attempt, an exploratory laparoscopy biopsy was done and the mass was histologically confirmed to be pancreatic ductal carcinoma.
Case Presentation
A 54-year-old female presented to the outpatient clinic with a 3-month history of dull abdominal pain that occasionally radiated to the back. Upon further questioning, she admitted to feeling fatigued and having a decreased appetite which resulted in a 7kg weight loss. She denied any nausea, vomiting, changes in bowel movement or consistency, or pruritus. The physical examination was remarkable for epigastric tenderness to palpation; however, jaundice or scleral icterus were absent. Due to the suspicion of biliary or pancreatic etiologies being the cause of her symptoms, an abdominal ultrasound (U/S) was conducted. It showed a 1.4 x 6.0 cm pancreatic mass at the junction of the body and head of the pancreas with no evidence of biliary or pancreatic ductal dilation. (Figure 1) highlights this finding.
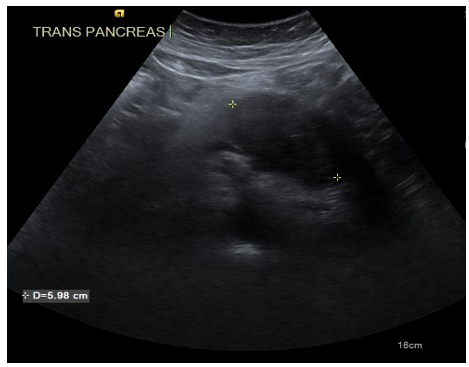
Figure 1: A pancreatic mass at the junction of the body and head of the pancreas measuring 1.4 x 6.0 cm.
Computed Tomography (CT) of the abdomen was conducted due to the positive findings on the U/S. It showed a 7.5 x 3.9 cm low-attenuation mass replacing the pancreatic parenchyma within the body and tail of the pancreas. The mass partially abutted surrounding structures such as the splenic artery and superior mesenteric artery. (Figure 2) shows these findings.
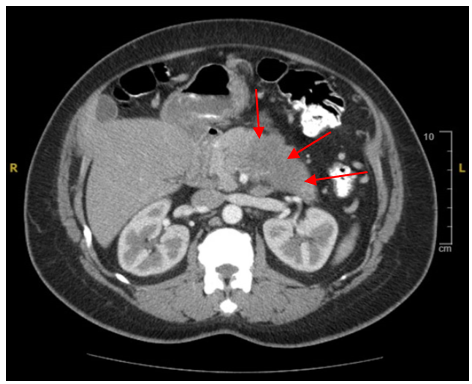
Figure 2: A hypoattenuating mass within the pancreatic body and tail measuring 7.5 x 3.9 cm.
These findings were highly concerning for pancreatic malignancy; therefore, a CT-guided pancreatic biopsy was conducted, however, the volume of the core biopsies taken made it difficult to definitively diagnose the patient resulting in the need for an exploratory laparoscopy to obtain an adequate amount of tissue. Upon exploration, an obvious mass in the center of the pancreatic body was visualized; it was firm and very abnormal in appearance. A Tru-Cut needle biopsy was done and the specimen was sent to pathology. Meticulous hemostasis was assured and the patient’s postoperative period was uncomplicated. Figure 3 highlights these findings.
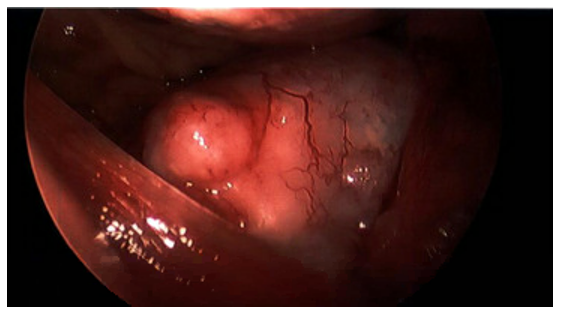
Figure 3: Laparoscopic imaging of the pancreatic mass.
Pathology results were positive for moderately differentiated adenocarcinoma most consistent with pancreatic duct carcinoma. A Port-A-Cath was placed for chemotherapy and the patient followed up with her oncologist for further management.
Discussion
Gene mutations in KRAS, CDKN2A, TP53, and SMAD4 contribute to abnormal epithelial proliferation within the pancreatic ducts [6]. This leads to the formation of pancreatic intraepithelial neoplasias which can progress to invasive pancreatic cancer when it spreads to other tissues and organs [6]. Diagnosis of pancreatic cancer requires multiple diagnostic scans, blood tests, and biopsies which are usually conducted when patients become symptomatic; by then there would be widespread metastasis and organ dysfunction [7]. In this case, our patient complained of abdominal pain radiating to the back. CT Scan and U/S with fine-needle aspiration can be used to confirm the diagnosis and surgical resection with adjuvant chemotherapy is the gold-standard treatment [6]. Only 10-20% of patients are eligible for surgical resection at the time of presentation [8].
Laparoscopy plays a big role in the diagnosis and management of pancreatic cancer. Small keyhole incisions are created and an instrument with a camera and tools known as the laparoscope is placed through the holes [9]. It allows the visualization of the entire abdominal cavity without the need to create large or midline incisions, allowing persons to recover at a quicker rate and have a short hospital stay [10]. There is less bleeding, pain, and a reduced risk of scarring after this procedure [9]. The risk of complications such as superficial site infections, perforation, and vascular injury ranges from 0.2 to 10.3% [11]. Laparoscopy can be used to take a biopsy, stage, and surgically resect the tumor when presented with a pancreatic mass.
For a pancreatic mass biopsy, samples of the tissue can be taken via percutaneous U/S-guided fine-needle aspiration, brush biopsy during an ERCP, and laparoscopic biopsy [12]. Laparoscopic biopsy is superior to the rest because it allows localization of the mass to allow accurate tissue sampling. In a retrospective review conducted on 76 people with pancreatic masses, there was a comparison of efficacy between CT-guided pancreatic biopsy and laparoscopic pancreatic biopsy [13]. It showed that laparoscopic biopsy had a higher diagnostic accuracy of 100% compared to the FNA with an accuracy of 81% [13].
Laparoscopic staging can occur after the diagnosis of pancreatic cancer has been established via biopsy. However, with advancements in CT imaging, the indications for laparoscopic staging of pancreatic masses have decreased [14]. Nevertheless, using laparoscopic U/S has been shown to detect locally advanced tumors with intraparenchymal involvement of surrounding structures and possible vascular involvement [14]. Some indications for laparoscopic U/S include large tumor size, involvement of the pancreatic neck, body, or tail, findings of hepatic involvement on CT that cannot be reached by percutaneous biopsy, and clinical findings pointing to advanced disease such as elevated CA19-9 of more than 150 U/ml, hypoalbuminemia and immense weight loss [11]. The sensitivity and specificity of diagnostic laparoscopy in identifying metastatic adenocarcinoma of the pancreas are 94% and 89% respectively [11]. In a study by Pisters et al, they found that in 4-13% of patients, laparoscopy detected metastatic cancer when there was no evidence found on CT [15]. This infers that laparoscopic staging reduces the number of radiologic investigations needed and the rate of subsequent non-therapeutic surgeries for non-resectable tumors.
Pancreaticoduodenectomy (PD) also known as the Whipple procedure can be conducted either open or laparoscopically. It involves the removal of the head of the pancreas, duodenum, gallbladder, and bile ducts in resectable pancreatic tumors [16]. A meta-analysis aimed to compare the benefits of a laparoscopic versus an open approach in 39771 patients [17]. They found that a laparoscopic approach was associated with less intraoperative blood loss, lower blood transfusion rate, less perioperative morbidity, lower wound infection rate, and shorter hospital stay length [16, 17]. However, the operative time was longer and patients who underwent this procedure had a smaller tumor size when compared to patients who underwent an open PD [17]. Absolute contraindications to laparoscopic procedures include perforation, peritonitis, history of surgical complications such as evisceration or shock, coagulopathy, and trauma with hemodynamic instability [11].
In this case, our patient underwent a needle-aspiration biopsy, however, an adequate diagnosis was not reached. The use of laparoscopic biopsy allowed a sufficient amount of tissue to be collected which provided the diagnosis of ductal pancreatic adenocarcinoma. According to the literature, biopsy, staging, and resection of pancreatic tumors via a laparoscopic approach are safe and effective and decrease unnecessary procedures that can impact the patient’s quality of life.
Conclusion
In conclusion, the minimally invasive procedure laparoscopy is an important diagnostic and therapeutic tool used in the management of pancreatic masses. It is beneficial due to its ability to offer a direct view of the pancreas, precisely assess the tumor's size, position, and link to adjacent tissues, and aid in the management of these masses without creating large or midline incisions, allowing persons to recover quickly. In this case, we explored the literature surrounding the benefits of using a laparoscopic approach for the diagnosis and management of this patient’s pancreatic mass and found that it is not only safe but an effective method for diagnosing and treating pancreatic masses without the need for additional, more extensive procedures.
Author Contributions
Shaniah Holder- Concept and Design of study, Acquisition of data, drafting article, revising article. Guarantor Author
Ehizele Itama – Concept and Design of study, drafting article intellectual content, revising article
Abigail Greaves – Acquisition of data, drafting article, revising article
Alaerebo Malvan Iyalla – Acquisition of data, drafting article, revising article
Frederick Tiesenga – Final Approval, Intellectual Content, revising article
Informed Consent: A signed statement of informed consent was obtained for publication of the details of this case
Competing Interests: None
Grant Information: None
References
- Moore K. Pancreatic cancer: Causes, symptoms, prognosis, and treatments. Healthline, 2021.
- Lee ES, Lee JM. Imaging diagnosis of pancreatic cancer: A state-of-the-art review. World Journal of Gastroenterology, 2014; 20(24): 7864. https://doi.org/10.3748/wjg.v20.i24.7864
- Pancreatic cancer symptoms. Johns Hopkins Medicine, 2021.
- Yang M, Zhang C-Y. Diagnostic biomarkers for pancreatic cancer: An update. World Journal of Gastroenterology, 2021; 27(45): 7862–7865. https://doi.org/10.3748/wjg.v27.i45.7862
- Pancreatic cancer early detection, diagnosis, and staging. (n.d.). American Cancer Society, 2023.
- Kamisawa T, Wood LD, Itoi T, et al. Pancreatic cancer. The Lancet, 2016; 388: 73-85. DOI: 10.1016/S0140-6736(16)00141-0.
- Pancreatic Cancer Screening, 2022.
- Muniraj T, Barve P. Laparoscopic staging and surgical treatment of pancreatic cancer. N Am J Med Sci, 2013; 5: 1-9. 10.4103/1947-2714.106183
- Laparoscopy (keyhole surgery), 2018.
- Ballehaninna UK, Chamberlain RS. Exploratory (Diagnostic) Laparoscopy. Medscape, 2022.
- Margina JF. Complications of Laparoscopic Surgery. Clinical Obstetrics and Gynecology, 2002; 45: 469-480.
- Biopsy of the Pancreas, 2023.
- Lin X, Lin R, Lu F, et al. Laparoscopic biopsy and staging for locally advanced pancreatic cancer: experiences of 76 consecutive patients in a single institution. Langenbecks Arch Surg, 2021; 406: 2315–2323. 10.1007/s00423-021-02199-5
- Shrikhande SV, Barreto SG, Shukla PJ. Laparoscopy in pancreatic tumors. J Minim Access Surg, 2007; 3: 47-51. DOI: 10.4103/0972-9941.33272
- Pisters PW, Lee JE, Vauthey JN, et al. Laparoscopy in the staging of pancreatic cancer. Br J Surg, 2001; 88: 325-337. DOI: 10.1046/j.1365-2168.2001.01695.x
- Gagner M, Palermo M. Laparoscopic Whipple procedure: review of the literature. J Hepatobiliary Pancreat Surg, 2009; 16: 726. DOI: 10.1007/s00534-009-0142-2
- Zhang H, Lan X, Peng B, et al. Is total laparoscopic pancreaticoduodenectomy superior to open procedure? A meta-analysis. World J Gastroenterol, 2019; 25: 5711-5731. DOI: 10.3748/wjg.v25.i37.5711

