Standardizing Results through Uniform Dilution of BoNT-As: A Comprehensive Approach for Scientific Consistency
Redaelli A1,*, Baldelli I2, Smit R3, Diaspro A4, Braccini F5, Vitale M6 and Sukmanskaya N7
1Visiting professor at Genova University, Italy
2Department of Integrated Surgical and Diagnostic Sciences, University of Genova; IRCCS Policlinico San Martino Hospital Genova, Italy
3Private practice, Pretoria, South Africa
4Private practice, Torino, Italy
5Private practice, Nice, France
6Private practice, Bologna Italy
7Head of global training, Fillmed, Paris, France
Received Date: 09/12/2023; Published Date: 24/04/2024
*Corresponding author: Alessio Redaelli, Mail@docredaelli.com, via di vittorio 24, 20070 Dresano, Milan Italy
Abstract
In the realm of scientific research, achieving consistent and comparable results across studies involving toxins of varying potencies poses a significant challenge. This article proposes a novel approach to address this issue by advocating for a uniform dilution strategy for both more and less powerful toxins. The rationale behind this unified dilution approach lies in its potential to enhance result reliability, comparability, and overall scientific consistency, irrespective of the toxin's potency. The Author has diluted the main European toxins (Abo – Azzalure 125U, Ona – Vistabex 50U, Inco – Bocouture 50U) with 0,63 ml of normal saline. In this way, doesn’t matter the toxin, the Author injects 0,01 ml for a very safe result, 0,02-3 ml for an average result and 0,05 ml to inject the on-label units for glabella and crow’s feet and have a strong result. Preliminary results are very good but a study on duration is on the way to check if the preliminary idea is right or not.
Keywords: Botulinum toxin; BoNT-A; Dilution; Active protein; Core toxin
Introduction
Toxins, ranging from highly potent molecules to less powerful substances, play a pivotal role in elucidating muscular and cosmetic responses and underlying biochemical mechanisms (5). However, the lack of standardized procedures in toxin dilution may lead to disparate findings, hindering the progress of scientific knowledge. This article advocates for a uniform dilution strategy to establish a common ground for result interpretation and comparison. The challenge arises when attempting to compare the effects of toxins with divergent potencies, as inconsistent methodologies in their dilution may lead to disparate results.
Diverse toxins exhibit varying degrees of potency, solubility, and stability, posing challenges in establishing a one-size-fits-all dilution protocol. Researchers often resort to ad-hoc dilution schemes, introducing variability that may compromise the robustness of experimental outcomes.
Rationale for Standardization:
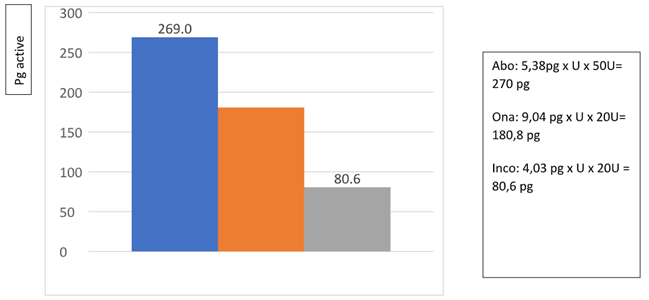
We know exactly [1]:
- the active core toxin (150 kD) is the same for all toxins type A.
- how many picograms of active neurotoxin we need to have a long-lasting result: around 270 pg.
- reducing the dilution, the diffusion will decrease accordingly maintaining the same results (to be proven)
- it is so easy get the final possibility to inject a similar quantity of active neurotoxin without increasing too much the dilution and so the diffusion.
This scientifical study is built of 2 steps:
- the first to confirm that on label units in a lower dilution are not affecting the safeness of the product and assess results at 1 month and 6 months (at least 1 grade improvement)
- the second step will be injecting more picograms of active neurotoxin in weaker toxins to try to uniform results without increasing side effects due to more diffusion.
A standardized dilution approach offers several advantages. Firstly, it ensures consistency in toxin (to be proved) exposure across experiments, reducing the impact of confounding variables, that are so real especially in young doctors.
Secondly, it facilitates the comparison of results obtained from different laboratories, fostering collaboration and cumulative knowledge.
Thirdly, it streamlines the optimization of experimental conditions, minimizing unnecessary complexities in study design.
Proposed Dilution Protocol:
The Author proposes a systematic dilution protocol that considers the unique characteristics of each toxin while maintaining a standardized framework. This involves establishing a baseline concentration range, employing a common solvent system, and accounting for factors such as stock solution preparation.
So, I propose 0,63 ml of normal saline for AboBoNT-A in 125U (on label dilution).
Again I propose half dilution of 0,63 ml of normal saline also for ONA BoNT-A 50 U
and finally again 0,63 ml of normal saline for IncoBoNT-A 50U.
This range will serve as the foundation for subsequent different injected ml of final diluted different toxins, ensuring that all experiments fall within a consistent and biologically relevant concentration spectrum.
Standardizing the preparation and storage of stock solutions contributes to result consistency, and in the opinion of the Author reduces diffusion allowing the injector to increase injected units to arrive around the same quantity of picograms demonstrated useful for best results. Researchers should provide detailed protocols for preparing and storing stock solutions, specifying parameters such as solution concentration, temperature, and dilution immediately prior to the treatment. Adhering to standardized stock solution procedures mitigates variations arising from differences in solution preparation.
The on-label injection in on label points for glabella is always the same with this dilution already approved by companies:
50U for 5 points in Glabella for AboBoNT-A and 30U for crow’s feet lines in 3 points x side
20U for 5 points in Glabella for Ona and for Inco BoNT-A and 12U for crow’s feet lines in 3 points x side (Off label dilution proposed by the Author).
Uniforming the dilution, we inject always 0,05 ml, doesn’t matter the toxin we use. Of course, it is possible the results will change slightly and this is the first target of our study.
The following further step will be increasing units, and so real pg injected, in weaker toxins to have similar results for all toxins.
Case Studies
Our target, at this step, will be demonstrate that on label units have good efficacy also in half dilution. To demonstrate the effectiveness of the proposed standardized dilution protocol, we will present case studies involving the most widely used toxins: ona, inco and abo BoNT-As but this dilution can be used with all possible toxins knowing exactly the pcgr present in each unit of different toxins. Through meticulous adherence to the standardized approach, we highlight the reduction in result variability and the enhancement of reproducibility across experiments.
A multicenter scientific study has been runned with 5 doctors treating each one 5 patients with different toxins and same dilution 0,63 ml, to check if this uniformation leads really to uniform results with a lower dilution and the same diffusion.
Final results of injected on label units will be presented in a next report. The first reports underline a similar effect of half diluted BoNT-As with a 1-2 grade reduction of glabellar lines at 1 month.
Discussion
Implementing a standardized dilution protocol has far-reaching implications for toxin-induced research. It fosters transparency, facilitates the validation of findings, and promotes the establishment of universal benchmarks. Additionally, it paves the way for meta-analyses and systematic reviews, offering a more comprehensive understanding of the effects of toxins on biological systems.
The effects I’m expecting are very similar to the on-label dilution. While the proposed standardized dilution protocol offers significant advantages, challenges and limitations must be acknowledged. Certain toxins may pose unique challenges in terms of diffusion and results, requiring adjustments to the protocol. Additionally, the adoption of standardized procedures may face initial resistance due to the inertia of established practices. However, these challenges can be addressed through collaborative efforts within the scientific community and ongoing refinement of the protocol.
For this reason, next step will be the uniformation of injected picograms to see if results get uniform. According to this principle, the author will inject the usual 0,05 ml x point for abobonta (270 pcgr total of active neuro-protein in glabella 5 points), but a bit more, 0,075 ml x point of OnaBoNT,A (280 pcgr x 30 U in 5 glabellar points) and 0,1 ml x point of IncoBoNT-A (161 pcgr x 40U in 5 glabellar points). The quantity of Pcgr for incoBoNT-A will be still too low, but anyway the increase of units will probably give us better results compared with on label units and dilution.
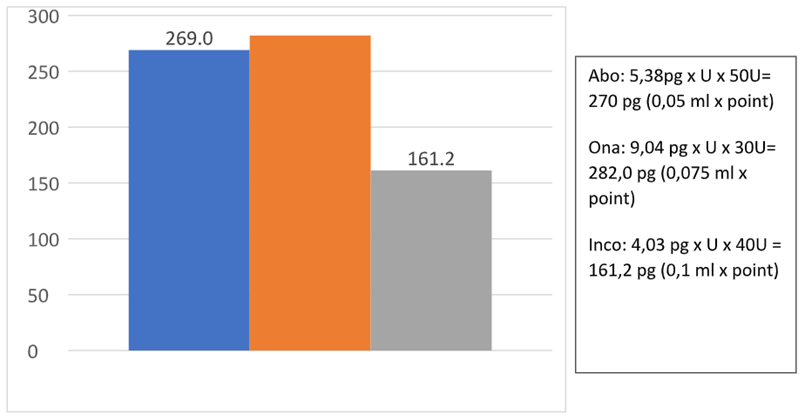
Then we’ll see the results at 6 months.
Conclusion
Standardizing the dilution of toxins represents a crucial step toward improving the rigor and reliability of scientific investigations. By adopting a uniform approach, researchers can enhance the reproducibility of results, promote cross-study comparability, and contribute to the advancement of knowledge in toxin-induced research. As the scientific community continues to grapple with the complexities of muscles responses to toxins, a commitment to standardized methodologies will undoubtedly strengthen the foundation of our collective understanding. The proposed dilution protocol serves as a practical guide for researchers, encouraging a shift towards greater consistency and harmonization in experimental practices. Preliminary results after 1 month, are very good but a study on duration is on the way to check if the preliminary idea is right or not. And remains valid that the only toxin to get fast onset of action and long results with on label units is only AboBoNT-A. All other toxins in on label units do not deliver sufficient quantity of active neurotoxin.
References
- Field M, et al. AbobotulinumtoxinA (Dysport®), OnabotulinumtoxinA (Botox®), and IncobotulinumtoxinA (Xeomin®) Neurotoxin Content and Potential Implications for Duration of Response in Patient. Toxins, 2018; 10(12): 535.
- Dysport® (abobotulinumtoxinA) [Prescribing Information]. Basking Ridge, NJ: Ipsen Biopharmaceuticals, Inc, 2017.
- Xeomin® (incobotulinumtoxinA) [Prescribing Information]. Raleigh, NC: Merz Pharmaceuticals, LLC, 2015.
- Botox® (onabotulinumtoxinA) [Prescribing Information]. Irvine, CA: Allergan, Inc, 2015.
- Redaelli A, et al. Botulinum Toxin A in aesthetic medicine and for hyperidrosis. 3rd edition OEO Firenze, 2020

