Incomplete Common Mesentery in Adults
Bouali Mounir, Eddaoudi Yassine, El Azhari Ilias*, El Bakouri Abdelilah, El Hattabi Khalid, Bensardi Fatima Zahra and Fadil Abdelaziz
Visceral surgery emergency department p35, University hospital center IBN rochd, Morocco
Received Date: 22/10/2023; Published Date: 02/04/2024
*Corresponding author: El Azhari Ilias, Visceral surgery emergency department p35, University hospital center IBN rochd, Morocco
Abstract
Introduction: Anomalies of intestinal rotation are widespread congenital anomalies in the general population, with clinical manifestations frequently found in pediatric age. One of the most common forms is the 180◦ incomplete common mesentery, whose most dreaded complication is volvulus.
Case Presentation: We report the case of a 60-year-old patient operated on for squamous cell carcinoma of the uterine cervix, who presented with an occlusive syndrome consisting of cessation of matter and gas with vomiting.
An abdomino-pelvic CT scan showed a 61.5 mm maximum-diameter bowel distension, with local hydroaeric levels, upstream of a transitional zone in the right iliac fossa, and a collapsed colonic frame, with diffuse peritoneal nodules heterogeneously enhanced after contrast injection.
The patient underwent a laparotomy, the exploration of which confirmed the presence of a 6-cm bowel distension with a magma of coves located at 1. 5 m from the duodeno-jejunal angle, trapped by nodules of carcinosis, with a SugarBaker Index of 13, with the presence of an incomplete common mesentery with the small intestines to the right of the rachis and the cecum subhepatically with the presence of Ladd's flange, the rest of the colon to the left.
Clinical Discussion: Incomplete common mesentery results from a rotation anomaly of the digestive tract, the prevalence of which is estimated at between 0.5% and 1% of the world population based on autopsy series .
During embryological development, the primitive intestine undergoes 3 rotations of 90° each.
When intestinal rotation stops at 180°, the position known as incomplete common mesentery is reached, resulting in the cecum rising upwards and to the right in a sub-hepatic position, with the duodenojejunal angle to the right of the rachis. The first jejunal loop and the last ileal loop are therefore located next to each other.
The position of the cecum forms an abutment between the cecum and the right upper parietal peritoneum known as Ladd's Bride.this position is at high risk of volvulus given the proximity of the first and last loop of the cecum.
Clinically, uncomplicated incomplete common mesentery is often asymptomatic or manifested by nonspecific abdominal symptoms such as chronic pain and diarrhoea, and can be diagnosed in a wide variety of circumstances, usually incidentally on radiological examination, or rarely during surgery.
When an incomplete common mesentery is discovered incidentally on radiology or intraoperatively, there is no consensus in the literature on whether to perform a prophylactic or elective Ladd procedure.
Laparoscopy is contraindicated in cases of volvulus on incomplete common mesentery.
It is estimated that the prevalence of these congenital malformations in adulthood is in the order of 0.2% to 0.5%, at which age they very often remain asymptomatic and therefore undiagnosed.
Conclusion: Abdomino-pelvic computed tomography with contrast injection is the gold standard for the positive diagnosis of incomplete common mesentery in adults. However, radiological examination should not delay therapeutic management. The prognosis is that of an occlusive syndrome, and is highly dependent on the time required for treatment and the patient's condition.
Keywords: Volvulus; Common mesentery; Intestinal occlusion; Small intestine
Introduction
Anomalies of intestinal rotation are widespread congenital anomalies in the general population, with clinical manifestations frequently found in pediatric age. One of the most common forms is the 180◦ incomplete common mesentery, whose most dreaded complication is volvulus. We report here on the discovery of a malrotation of the incomplete common mesentery type in a patient admitted for occlusion on peritoneal carcinosis.
Observation
We report the case of a 60-year-old patient operated on for squamous cell carcinoma of the uterine cervix, who presented with an occlusive syndrome consisting of cessation of matter and gas with vomiting.
On clinical examination, the patient presented with hypotension at 080/040 mmHg with tachycardia at 120 bpm, the abdomen was tympanically distended, with palpation of a subcutaneous nodule at the umbilicus. Rectal examination was unremarkable, finding an empty rectal ampulla with no palpable mass and the vaginal examination was marked by the presence of a free section.
Hemoglobin was 13.3 g/dl, white blood cells 8340/mm 3, natremia 140 mEq/L and kalemia 5.2 mEq/L. Renal function was preserved, with urea 0.46 g/L and creatinemia 8.9 mg/L.
An abdomino-pelvic CT scan showed a 61.5 mm maximum-diameter bowel distension, with local hydroaeric levels, upstream of a transitional zone in the right iliac fossa, and a collapsed colonic frame, with diffuse peritoneal nodules heterogeneously enhanced after contrast injection (Figure 1).
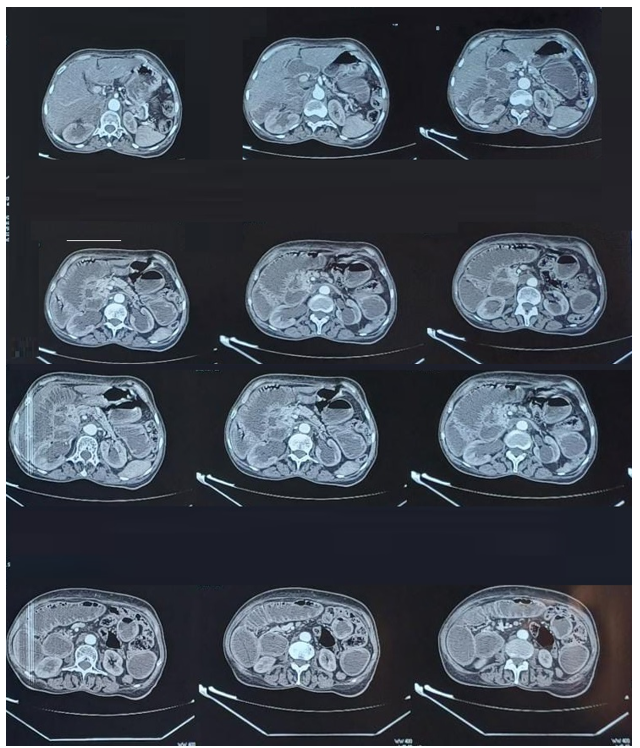
Figure 1: An abdomino-pelvic CT scan showed a 61.5 mm maximum-diameter bowel distension, with local hydroaeric levels, upstream of a transitional zone in the right iliac fossa, and a collapsed colonic frame.
The patient underwent a laparotomy, the exploration of which confirmed the presence of a 6-cm bowel distension with a magma of coves located at 1. 5 m from the duodeno-jejunal angle, trapped by nodules of carcinosis, with a SugarBaker Index of 13, with the presence of an incomplete common mesentery with the small intestines to the right of the rachis (Figure 2) and the cecum subhepatically with the presence of Ladd's flange, the rest of the colon to the left (Figure 3).

Figure 2: Intraoperative image: shows treitz angle before the detachment on the right of the spinal line.

Figure 3: Intraoperative image: the abnormal layout with small intestine on the right and the entire colon on the left with cecum on the lower left.
Surgery consisted of segmental resection of the magma of coves trapped by carcinosis, double gun barrel ileostomy with prophylactic LADD procedure: cecum release, release of Treitz angle, principal appendectomy. and positioning of the coves in complete common mesentery position at 90°.
The post-operative course was straightforward and uncomplicated, with a functional ileostomy at 2 days post-operatively. The patient was subsequently referred for chemotherapy.
Discussion
Incomplete common mesentery results from a rotation anomaly of the digestive tract, the prevalence of which is estimated at between 0.5% and 1% of the world population based on autopsy series [1].
During embryological development, the primitive intestine undergoes 3 rotations of 90° each [2]. When intestinal rotation stops at 180°, the position known as incomplete common mesentery is reached, resulting in the cecum rising upwards and to the right in a sub-hepatic position, with the duodenojejunal angle to the right of the rachis. The first jejunal loop and the last ileal loop are therefore located next to each other.
The position of the cecum forms an abutment between the cecum and the right upper parietal peritoneum known as Ladd's Bride.this position is at high risk of volvulus given the proximity of the first and last loop of the cecum.
Clinically, uncomplicated incomplete common mesentery is often asymptomatic or manifested by nonspecific abdominal symptoms such as chronic pain and diarrhoea, and can be diagnosed in a wide variety of circumstances, usually incidentally on radiological examination, or rarely during surgery, as in our case [3].
In these asymptomatic patients, the diagnosis may be revealed during attacks of ectopic appendicitis [12] or by chance during radiological examination. Complications of intestinal rotation anomalies can be acute or chronic in adults. Acute complications include duodenal flange occlusion and total volvulus of the small bowel, which remains exceptional in adults, but has a dreadful prognosis. Chronic complications arise from incomplete duodenal stenosis or chronic small bowel volvulus with mesenteric arterial insufficiency. The diagnosis of total small bowel volvulus can be made in a wide variety of circumstances: in an emergency, in the face of acute intestinal obstruction, or even a state of shock [13] that can lead to death.
The gold standard for diagnosing an incomplete, uncomplicated common mesentery is an abdominal CT scan, which shows Treitz's angle, the whole of the small intestine to the right of the spine, the cecum in a subhepatic position and malposition of the mesenteric vessels, with the superior mesenteric vein directly behind the superior mesenteric artery. Abdominal MRI provides the same results as CT. Abdominal Doppler ultrasound is of little interest, but in certain cases it can visualize malposition of the mesenteric vessels [3].
Ladd's procedure is the reference treatment for volvulus on incomplete common mesentery, and consists in detorsion of the small intestine, release of the cecum, appendectomy in principle and placement in complete common mesentery at 90° [2]. Appendectomy in principle is performed because of the risk of diagnostic delay when placing the patient back in complete common mesentery at 90°, as the appendix will be in the left iliac fossa in this situation [4].
Pexy is of no interest, as it does not prevent the intestine from returning to the malrotation position, and may even lead to complications such as internal flanges and hernias [2].
When an incomplete common mesentery is discovered incidentally on radiology or intraoperatively, there is no consensus in the literature on whether to perform a prophylactic or elective Ladd procedure [5]. Some authors believe that all malrotations should be operated on [6]. The elective Ladd procedure in adults presents few post-operative complications, the most dreaded of which is occlusion due to post-operative flange formation [3,7]. Laparoscopy presents fewer complications than laparotomy, with less risk of post-operative flange formation, and remains a less invasive approach [8].
Laparoscopy is contraindicated in cases of volvulus on incomplete common mesentery [2]. In our case, there were no post-operative complications.
It is estimated that the prevalence of these congenital malformations in adulthood is in the order of 0.2% to 0.5% [10,11], at which age they very often remain asymptomatic and therefore undiagnosed.
Conclusion
Abdomino-pelvic computed tomography with contrast injection is the gold standard for the positive diagnosis of incomplete common mesentery in adults. However, radiological examination should not delay therapeutic management. The prognosis is that of an occlusive syndrome, and is highly dependent on the time required for treatment and the patient's condition.
A fearsome and exceptional complication in adulthood. The high mortality rate due to delayed diagnosis means that every practitioner must be aware of these rotational anomalies and the complications they can cause. Since clinical symptoms are non-specific, there should be no delay in performing radiological examinations. The prognosis for total volvulus of the small intestine is determined by the occlusive syndrome and the microbial proliferation it causes, and is highly dependent on the time taken to treat the condition, as well as on the terrain.
References
- Kapfer SA, Rappold JF. Intestinal malrotation-not just the pediatric surgeon’s problem. J Am Coll Surg, 2004; 199: 628–635.
- Peycelon M, Kotobi H. Complications des anomalies embryologiques de la rotation intestinale: prise en charge chez l’adulte. EMC - Techniques chirurgicales - Appareil digestif, 2012; 7(4): 1-12.
- Moldrem AW, Papaconstantinou H, Broker H, et al. Late Presentation of Intestinal Malrotation: An Argument for Elective Repair. World J Surg, 2008; 32: 1426–1431. https://doi.org/10.1007/s00268-008-9490-3.
- Tan V, Kotobi H, Parc Y. Technique chirurgicale: la procédure de Ladd pour volvulus total du grêle sur malrotation,,Journal de Chirurgie Viscérale, 2017; 154(3): Pages 204-208. https://doi.org/10.1016/j.jchirv.2016.04.022.
- David C Yu, Ravi R, et al. Outcomes after the Ladd procedure in patients with heterotaxy syndrome, congenital heart disease, and intestinal malrotation, Journal of Pediatric Surgery, 2009; 44(6): 1089-1095.
- Draus JM Jr, Foley DS, Bond SJ. Laparoscopic Ladd procedure: a minimally invasive approach to malrotation without midgut volvulus. Am Surg, 2007; 73(7): 693-696.
- Malek MM, Burd RS. The optimal management of malrotation diagnosed after infancy: a decision analysis. Am J Surg, 2006; 191(1): 45-51. doi: 10.1016/j.amjsurg.2005.10.002.
- A.P. Arnaud, C. Capito, et al SFCP CO-04 - Procédure de Ladd coelioscopique pour malrotation intestinale, une approche controversée, Archives de Pédiatrie, 2014; 21(5): Supplement 1.
- Durkin Emily T, Lund Dennis P, et al. Age-Related Differences in Diagnosis and Morbidity of Intestinal Malrotation. Journal of the American College of Surgeons.
- Gamblin T, Stephens R, Johnson R, Rothwell M. Adult malrotation: a case report and review of the literature. Curr Surg, 2003; 60(5): 517–520.
- Jarry J, Razafindratsira T, Bodin R, Lepront D, Durand-Dastes F. À propos d'un cas de mésentère commun complet de l'adulte révélé par une complication occlusive. Presse Med, 2008; 37(11): 1689–1692.
- Sarazin R, Voisin R, Sarroste J, Manabie B. Mésentérium commune découvert chez l'adulte à l'occasion d'une appendicite aigue. Journal de médecine de Bordeaux, 1967; 144: 1556–1561.
- Amaral L, Quintanilha R, Bernardo L, Eloi T, Bento F, Santos V. Intestinal malrotation in the elderly. Am Surg. 2009;75(7):631–633.

