Severe Intra-Abdominal Hemorrhage Caused by Invasion of Chorionic Villi into the Myometrium Resulting from Undetected Uterine Perforation
Houyu Yang*, Yuanjunzi Shi, BD and Gang Ji
Department of Gynecology, The Second People’s Hospital of Guiyang, Guiyang, China
Received Date: 19/10/2023; Published Date: 27/03/2024
*Corresponding author: Gang Ji, Department of Gynecology, The Second People’s Hospital of Guiyang, No.547 South Jinyang Road, Guiyang 550023, China
Abstract
Perforation is a well-known complication of induced abortion, but severe intra-abdominal bleeding due to the invasion of chorionic villus into the uterine myometrium resulting from undetected perforation is rare. Herein, we report a case of a 26-year-old woman,who received an induced abortion 22 days ago,underwent laparoscopy for considered intra-abdominal bleeding and elevated plasma beta-HCG. Under laparoscopy, bleeding was active on the uterine surface, the superficial bleeding tissues were removed and confirmed as chorionic villi by histopathological examination, and methotrexate(50mg/m2) was locally injected. Because the plasma beta-HCG continued to rise and ultrasound indicated a mass in the left cornua uteri, we performed hysteroscopy after a 5-day combined drug therapy with only an empty cavity observed, so another drug therapy was applied for 5 days, and the plasma beta-HCG level gradually declined to negative. This case report highlights the importance of being alert to women who suffer from intra-abdominal hemorrhage after an induced abortion such as this condition.
Keywords: Chorionic villi; Hemorrhage; Induced abortion; Invasion; Uterine perforation
Introduction
Induced abortion is a common technique to terminate first- or second-trimester pregnancy. Injury caused by uterine perforation to organs such as the bowel, bladder, or vasculature may be the riskiest complication, and timely management is crucial to minimize harm [1]. However, if a perforation is ignored or not identified during the procedure and chorionic villi enter the damaged myometrium simultaneously, the patient may suffer from late severe intra-abdominal hemorrhage. It’s difficult to predict whether this rare condition will occur even if the patient has a regular ultrasound for a follow-up 1 week after the abortion because the patient can be asymptomatic before bleeding and chorionic villi need quite a few days to grow and invade the deeper myometrium. Hitherto, no studies or case reports of this condition have been reported, and we present a rare case herein to share the experience and difficulties we experienced in treating the patient.
Case Report
A 26-year-old woman, gravida 2 para 0, was admitted to the gynecological emergency department of our hospital for acute lower abdominal pain on Dec 27, 2022. Her skin and eyelid looked pale, and her blood pressure was 76/44mmHg, while other vital signs were normal. Except for a floating uterus, the gynecological examination was normal. When asked about her medical history, she emphasized that she had received an induced abortion 22 days ago at a local hospital, and the procedure wasn’t special, according to her doctor. In addition, she denied a history of sexual intercourse after the operation.
The plasma beta-HCG level was 2597.00mIU/ml, and transvaginal ultrasound indicated intra-abdominal hemorrhage with an unclear display of the uterus and double appendages, so we performed emergent laparoscopy immediately with a suspected diagnosis of ectopic pregnancy. Under laparoscopy, a total of 1200ml of intra-abdominal bleeding was aspirated. The fallopian tubes and ovaries were normal, and bleeding was active on the uterine surface where the origin of the left round ligament closed (Figure 1). The bleeding spot was 0.5cm in diameter with some resembled chorionic villi tissues on it. We removed the superficial bleeding tissues for histopathological examination and stopped bleeding by electrocoagulation. Then, methotrexate (50mg/m2) was locally injected to inactivate possibly retained products of conception. However, the plasma beta-HCG level rose to 2650.00mIU/ml on the second postoperative day, and ultrasound indicated a mass (1.4cm×1.1cm in size) in the left cornua uteri (Figure 2), so a drug combination of methotrexate (10mg/Qd) and mifepristone (50mg/Bid) was applied for 5 days. Unsatisfyingly, the plasma beta-HCG level declined to 2321.00 mIU/ml. Thus, after reviewing the ultrasound checked before the induced abortion (Figure 3), we performed hysteroscopy to try to clear the possibly retained products of conception inside the uterine cavity, but no tissue was observed (Figure 4).
It was the time we confirmed the invasion of chorionic villi into the myometrium led to severe intra-abdominal hemorrhage, a constant high level of plasma beta-HCG, and the futility of hysteroscopy when the histopathological examination indicated villi and trophoblast cells (Figure 5) 6 days after laparoscopy. In consideration of harm to the uterus if another surgery attempted to respect the invaded myometrium and methotrexate had been used intraoperatively and postoperatively, we used a single drug protocol of mifepristone (50mg/Bid×5days) to terminate the pregnancy further. The plasma beta-HCG declined to 1040.00mIU/ml, and the liver function test was normal. The patient departed from the hospital on the 11th day of hospitalization.
During a follow-up of 6 months, blood HCG was monitored once a week until negative on Feb 9, 2023. The patient resumed menstruation on Feb 21, 2023, with 5 subsequent cycles of the same volume and duration as preoperatively.

Figure 1: The fallopian tubes and ovaries were normal; the bleeding spot close to the origin of the left round ligament was 0.5 cm in diameter with some chorionic villi tissues.

Figure 2: A mass (1.4cm×1.1cm in size,white arrow) in the left cornua uteri was indicated by ultrasound on the second postoperative day.

Figure 3: The ultrasound checked in the local hospital before the abortion could exclude cornual or ectopic pregnancy.

Figure 4: Under hysteroscopy, no pregnancy tissue was observed in the uterine cavity; the left tubal ostium was visible (black arrow).
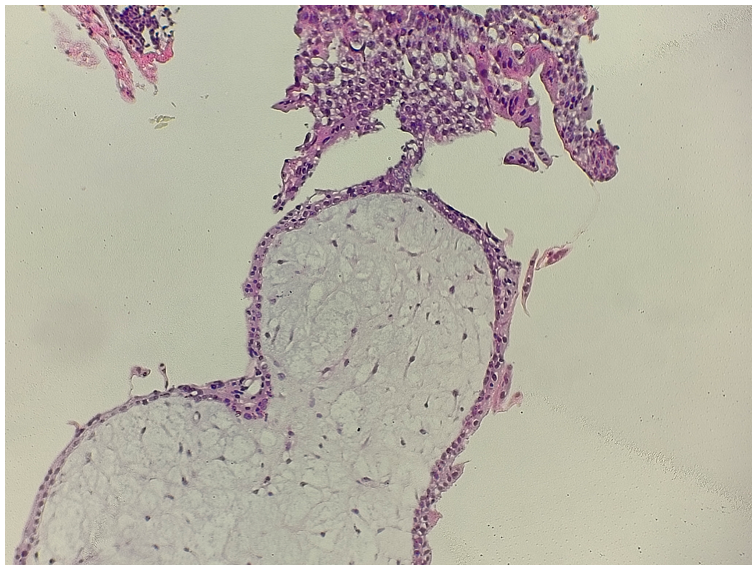
Figure 5: The tissues removed from the uterine surface were histopathologically confirmed as chorionic villi and trophoblast cells (hematoxylin and eosin staining × 40).
Discussion
An induced abortion can be safe with experienced providers [2], and perforation is not a rare complication because many factors can lead to its occurrence [3-5]. However, chorionic villi entering the myometrium along with uterine perforation and then causing late severe intra-abdominal bleeding is rare. We used “induced abortion; uterine perforation; chorionic villi; intra-abdominal hemorrhage” as keywords to search PubMed, but no articles published in English were retrieved.
The rarity of this condition may be attributed to clinicians being alert to perforation, and immediate identification and timely management can prevent concomitant injury from being life-threatening. However, perforation may be ignored or not identified because the provider is inexperienced or the myometrium isn’t fully perforated. Moreover, there are no concrete methods to predict whether chorionic villi invade, even if regular postoperative ultrasound is monitored, mainly because the invasion is asymptomatic until bleeding and the invading chorionic villi need time to be indicated by imaging examination.
To the best of our knowledge, there are pathological mechanisms by which chorionic villi can invade the uterine myometrium: 1) invasive hydatidiform mole or choriocarcinoma; 2) cesarean scar pregnancy; and 3) uterine perforation.
The patient in this report received an induced abortion but wasn’t told perforation. We analyzed the bleeding event as a subsequence of the pregnancy, and the invasion of chorionic villi led to severe intra-abdominal hemorrhage. The reasons are as follows: 1) the patient denied postoperative sexual intercourse; 2) HCG was still high 22 days after the abortion and even continued to rise; 3) chorionic villi and trophoblast cells located on the uterine surface were histopathologically confirmed; 4) a mass was indicated in the left cornua uteri by ultrasound but the uterine cavity was proven empty with hysteroscopy; and 5) the patient didn’t receive a surgery that may have left a scar on her uterus.
Unawareness of such a confusing condition and inadequate clinical evidence could explain our failure to make accurate diagnoses when the patient was admitted. We strongly recommend a CT scan before surgery if a patient is hemodynamically stable because studies have proven its superiority in finding a perforation compared with ultrasound[6,7]. Of course, laparoscopy was more reasonable than transferring the patient to a CT room when her blood pressure was 76/44mmHg. In addition, abdominal pregnancy should be distinguished from chorionic villi invasion if pregnant tissues accidentally appear outside uterine and fallopian tubes. Criteria from Studdiford [8] can help.
In addition to making an accurate diagnosis, another difficulty we encountered was how to operate. Certainly, surgical hemostasis is the first task to rescue, and laparoscopy is a preferred choice to explore, but a combination with hysteroscopy is necessary if the pathological mechanism is considered; thus, a second anesthesia can be avoided. Of note, considering harm to the uterus, full-layer myometrium removal isn’t a recommendation for nulliparas, and it’s difficult to ensure that the invaded myometrium is completely removed during the operation, even if the patient agrees to undergo this operation. In addition to surgical treatment, subsequent drug treatment plays an essential role in inactivating the residual invading tissues. A combination of methotrexate and mifepristone is effective, but liver function should be monitored. For postoperative follow-up, we recommend monitoring both HCG and transvaginal ultrasound. Menstrual recovery is a sign of disease cure.
Conclusion
Intra-abdominal hemorrhage after a recent induced abortion should take chorionic villi invasion into account, and it’s preferred to perform laparoscopy combined with hysteroscopy. If full-layer invaded myometrium removal isn’t under consideration, a subsequent combined drug application is recommended. We suggest monitoring both HCG and transvaginal ultrasound until regular menstruation recovers.
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Grant Information: The authors received no specific funding for this work.
Acknowledgments:We thank Dan Wu for treating the patient.
References
- Bridwell RE, Long B, Montrief T, Gottlieb M. Post-abortion Complications: A Narrative Review for Emergency Clinicians. West J Emerg Med, 2022; 23(6): 919-925.
- Kerns J, Steinauer J. Management of postabortion hemorrhage: release date November 2012 SFP Guideline #20131. Contraception, 2013; 87(3): 331-342.
- Adler AJ, Filippi V, Thomas SL, Ronsmans C. Quantifying the global burden of morbidity due to unsafe abortion: magnitude in hospital-based studies and methodological issues. Int J Gynaecol Obstet, 2012; 118 Suppl 2: S65-77.
- White K, Carroll E, Grossman D. Complications from first-trimester aspiration abortion: a systematic review of the literature. Contraception, 2015; 92(5): 422-438.
- Wu YM, Gomez-Alzugaray M, Haukkamaa M, Ngoc N,Ho PC,PretnarDarovec A,et al. Comparison of two doses of mifepristone in combination with misoprostol for early medical abortion: A randomised trial. BJOG An Int J Obstet Gynaecol, 2000; 107(4): 524–530.
- Shulman SG, Bell CL, Hampf FE. Uterine perforation and small bowel incarceration: sonographic and surgical findings. Emerg Radiol, 2006; 13(1): 43-45.
- Grossman D, Grindlay K, Buchacker T, Lane K,Blanchard K. Effectiveness and acceptability of medical abortion provided through telemedicine. Obstet Gynecol, 2011; 118(2 Pt 1): 296-303.
- Studdiford WE. Primary peritoneal pregnancy. Am J Obstet Gynecol, 1942; 44(3): 487-491.

