Histiocytoselangerhansian Andpathological Fractures
Chirimwami BR1,*, Mushegera DK1, Galant C2, Kuyigwa G3, Mubenga3, Maheshe B3 and Ngalula UA1
1Faculty of Medicine, Department of Surgery and Department of Pathological Anatomy, University of Kinshasa, R.D. Congo
2Université Catholique de Louvain en Woluwé, School of Public Health, Belgium
3Faculty of Medicine, Department of Surgery and Department of Internal Medicine, Catholic University of Bukavu, R.D. Congo
Received Date: 17/10/2023; Published Date: 26/03/2024
*Corresponding author: Chirimwami BR, Faculty of Medicine, Department of Surgery and Department of Pathological Anatomy, University of Kinshasa, Belgium
Summary
Purpose and Context: Pathological fractures are not uncommon. We wanted to draw the attention of practitioners to this section of medical pathology, the etiological basis of which is often found in rare diseases, as is the case in the patient we report here.
Methodology: Here, we present a review of the literature on pathological fractures, with a focus on children and young adults, with a clinical illustration.
Results: Pathological fractures are favoured by various pathologies, congenital or acquired, ranging from metabolic and genetic diseases, through neoplasms including benign neoplasms and malignant neoplasms to infectious diseases. In children and young adults, genetic diseases such as haemoglobinosis S in our regions of Central Africa are the main preoccupations, followed by infectious diseases such as acute or chronic osteomyelitis, bone cysts, benign neoplasms (fibroids, chondromas) and proliferative haematological diseases such as Langerhans cell histiocytosis.
We take this opportunity to illustrate thislast rare pathology, by the case of a 35-year-old young adult patient of masculin sex for whom the histopathological diagnosis has been clarified by identifying, on the biopsy sample, the proliferation of Langerhans cells by the antigenic marker specific to this cell.
Conclusion: In the case of an almost spontaneous fracture, because it is caused by a very slight trauma, particularly in children, the underlying cause that allows for the administration of an etiological treatment should not be missed.
Keywords: Pathological fractures; Children; Langerhans cell histiocytosis
Introduction
Pathological fractures are defined as those that occur as a result of minimal trauma, on a bone weakened by a pre-existing condition [1]. The underlying condition can be either systemic such as osteoporosis [2], endocrine metabolic disorders, hematologic malignancies [3] or local diseases such as bone tumors [4]. In children and young adults, it is mainly genetic diseases such as sickle cell anemia in our region of Central Africa [1], followed by infectious diseases such as acute or chronic osteomyelitis [5,6], then bone cysts [7], benign tumours [8,9] but also rare proliferative haematological diseases such as Langérhans cell histiocytosis [10, 11].
Objective
The aim of this work is to illustrate the case of pathological fracture secondary to histiocytoselangerhansia, an unusual diagnosis and the very first case, to our knowledge, reported in our country, the Democratic Republic of Congo.
Observation
In 2003, the 35-year-old patient, who was married, father of 6 children and a soldier by profession, presented with complaints, pain, infirmity and deformity of the right thigh. These symptoms began when the patient was getting out of a car 4 days prior. In his story, we noted that he was hospitalized in another unit for aswollen right collarbone, for which he received non-precise treatment.
In October 2002, 9 months before our consultation, this patient was hospitalized for generalized bone pain, particularly in the hip. Later, in 2003, he developed a deformity of the skull in the form of 3 depressions, at the occipital and the 2 parietals.
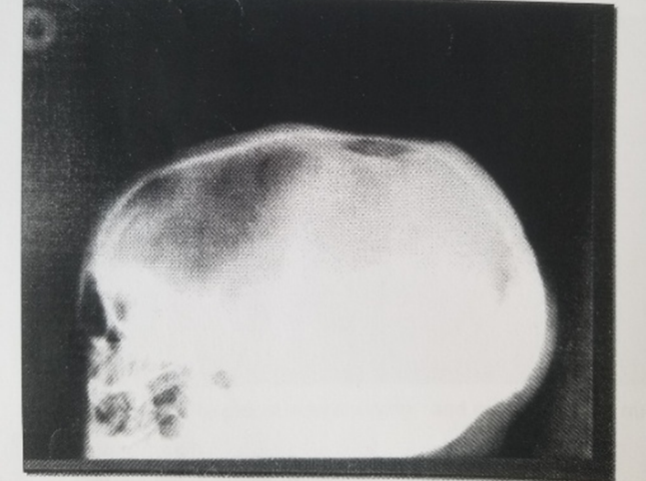
Figure 1: Lateral view of the skull showing lytic lesions of the frontal and occipital bone.
The patient is the4th of eight siblings. His siblings were apparently in good health. He was a cigarette smoker and took alcohol. He presented with asthenia and polyuria with transient polydipsia. The pain in the thigh radiated to the knee, it was exacerbated by walking and calmed by rest.
Cardiac and pulmonary physical examination were within normal limits.
Lymphadenopathy and hepatosplenomegaly were not present. The fractured femur had kept the classic posture, it was shortened and the lateral side of the right foot was lying on the bed. The diagnosis of pathological fractures with probable diabetes mellitus has been suggested. Usual laboratory tests demonstrated high sedimentation rate, mild leukopenia, and hypoglycemia. X-ray of the right femur showed a single, roughly oblique fracture line at the union of the medial third with the proximal third of the femoral shaft, with an overlap of 2 cm.

Figure 2: Fracture of the right femur at the union of the middle third and proximal third with an overlap of 2 cm.
This fracturewas treated by osteosynthesis with the Kuntscher pin and we found a satisfactory reduction. There was loss of bone substance due to the biopsy.
Histopathological analysis showed 2 fragments of fibrous tissue vascularized and containing a fibrinous deposit on the surface. On one fragment we observed a polymorphic inflammatory granuloma made of numerous eosinophils, lymphocytes and medium-sized cells with a large cytoplasmic vacuole and a nucleus with a strong notch. There were also rare multinucleated giant cells. The diagnosis of Langerhansian cell histiocytosis was retained.
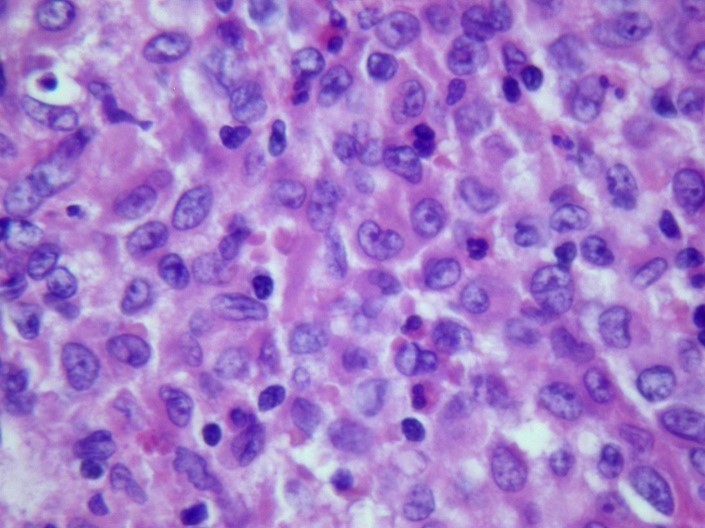
Figure 3: HEX400 showing numerous histiocytes with a large vacuolar cytoplasm, a notched nucleus, and a prominent nucleolus, suggesting langurhanian cells.
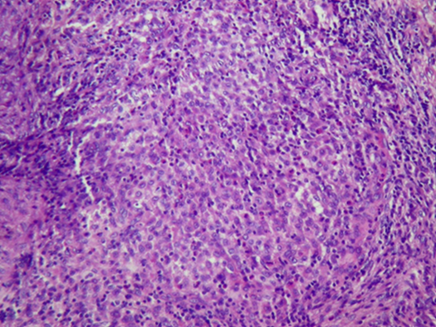
Figure 4: HEx100 overview showing cells with dark nuclei corresponding to inflammatory cells.
The sample was then sent to the laboratory of the Saint-Luc Clinics in UCL, Leuven, Belgium. An immunohistochemical assay with anti-CD1a antibodies labeled these cells with inter-shaped nuclei, confirming the diagnosis of histiocytoselangerhans.

Figure 5: X400 CD1a immunohistochemistry showing membrane marking of langerhansian cells.
Later, the patient experienced another fracture in the humerus, for which he received specific treatment. This patient was seen again in July 2009, somelesions healed, and others appeared on X-rays of the shoulder blades and femoral necks.
Discussion
Langerhans cell histiocytosis is a rare disease, characterized by clonal proliferation of dendritic cells that resemble Langerhans cells, in different tissues of the body [11,12]. A mutation in the B-RAF gene has been found in more than 50% of patients [13]. It is a disease that affects all ages with a predominance in children and young adults [11]. The global incidence is estimated at 5 cases per million in children under 15 years of age and 2.7 cases per million in adults [14]. The clinical aspects are polymorphic, the disease can affect several organs including the lungs, skin, pituitary gland and many other systems [11]. Depending on the clinical manifestations, three forms are classified by the Histiocyte Society [13]:
- Localized forms (eosinophilic granuloma) in adults, affecting in particular the bone, the lungs, and often of a favorable course,
- Multifocal forms of older children and young adults (Hand-Schuller-Christian syndrome): variable in course, often indolent,
- Disseminated multi-tissue forms (Letterer Siwe): acute presentation, in infants, and severe evolution;
Bone is more affected than other organs with 30 to 50% craniofacial localization and long bones [14]. The symptoms of bone damage are mainly pain, swelling and rarely pathological fracture [1]. Diagnosis is based on radiological (lytic image) and clinical signs, combined with histopathological analysis on bone biopsy [12]. Histologic analysis shows clonal tissue proliferation of dendritic cells with the morphological and immunohistochemical characteristics of Langerhans cells. Thus, antibodies such as anti-CD1a and langerin are useful for confirmation of diagnosis [14]. Histiocytoselangerhansian is not immediately considered to be a malignant tumor, despite the aggressive form, Letterer-Siwe's disease [11].
The prognosis of the disease is generally good, but it is highly variable depending on the clinical form. The factors for poor prognosis are [13]:
- The age of disclosure less than 2 years (and especially less than 1 year),
- A number of organs affected greater than or equal to 3
- Hepatic, spinal cord, pulmonary or digestive damage
As a result, the disease can regress spontaneously or progress rapidly, sometimes leading to death [13].
Conclusion
Pathological fractures can be caused by several etiologies ranging from genetic diseases to tumor diseases to inflammatory diseases. Langerhans cell histiocytosis is a rare cause of pathological fractures that are diagnosed by clinical, imaging, and histopathology.
°In memorium Pr Dr Mushegera D.K, University of Kinshasa, D.R. Congo
References
- Akinyele Lawrence Akinyoola, Elkanah Ayodele Orimolade et Moruf Babatunde Yusuf. Pathologic fractures of long bones in Nigerian children J Child Orthop, 2008; 2: 475-479. DOI 10.1007/s11832-008-0141-x
- Sophia D Sakka, Moira S Cheung. Management of primary and secondary osteoporosis in children. Ther Adv Musculoskel Dis, 2020; 12: 1–21. DOI: 10.1177/1759720X20969262.
- Ngolet LO, Kocko I, GalibaAtipo FO, Guelongo Okouango Ova JD, Ntsiba H, Elira Dokekias A. Symptomatic multiple myeloma in Brazzaville: About 40 cases, Annals of Marien Ngouabi University, 2016; 16 (1): 1-7.
- EL Batochy Meriem. Pathological fractures in bone tumors. Doctoral Thesis in Medicine, Rabat, 2015; N° 122: p 158.
- Mohamed Ben Jemaa, et al. Community-acquired methicillin-resistant Staphylococcus aureus acute osteomyelitis in children: about 15 cases. Pan AfricanMedical Journal, 2021; 39(84). DOI: 10.11604/pamj.2021.39.84.12560:3.
- Traoré O, Yilboudo J, Reyes G, Rouamba A, Ouiminga RM. Chronic osteomyelitis: clinical and therapeutic aspects about 38 cases at the National Hospital Center (C.H.N) OF BOBO-DIOULASSO. Black African Medicine, 1997; 44(3).
- Kaelina A, Dutoitb M, Jundtc G, Siebenrockd K, von Hochstettere A, Heftif F. The Solitary Bone Cyst (KOS) For Forum Med Switzerland, 2007; 7: 345–350.
- Youssef Nader, et al. Secondary pathological fractures of benign tumors in children: about 20 cases. Pan AfricanMedical Journal, 2015; 21: 204. doi: 11604/pamj.2015.21.204.6556.
- Abdelkader Bahi. Pathological fractures secondary to benign bone lesions in children: about a series of 32 cases. Ph.D. Thesis in Medicine, Rabat, 2012; No. 261: p 159.
- Histiocytoselangerhansienne Orphanet Urgences, 2020.
- Sabani H, El Khatib MK, Hamama J, Nassih M, Rzin A, Zoubir Y, et al. Multifocal bone histiocytoselangerhansian. About a case. ActualOdonto-Stomatol, 2012; 258:127-133.
- Nguyen K, Tazi A. Histiocytoselangerhansian in adults. Rev Prat, 2006; 56: 1863-1871.
- pdf [Internet]. [cited 2023 Jun 23]. Available at: https://www.has-sante.fr/upload/docs/application/pdf/2021-11/pnds_hl_has_15112021revue_litterature.
- Tazi A, Saint-Louis H. Langerhansian histiocytosis in adults, 2018.

