Surgical Management of Congenital Melanotic Nevus Using Wolfe’s Graft
Shailesh Kokal, Sri Sai Aishwarya, Yamini Ghatikar*, Vidya KC and Mena C
Department Of Oral and Maxillofacial Surgery, Coorg Institute of Dental Sciences, India
Received Date: 21/09/2023; Published Date: 23/02/2024
*Corresponding author: Dr. Yamini Ghatikar, Post Graduate Trainee, Department of Oral and Maxillofacial Surgery, Coorg Institute of Dental Sciences, Virajpet, India
Abstract
Congenital and acquired melanocytic nevi are thought to be precursors to melanomas. The somatic mutation of melanocytic cells during embryofetal development results in these congenital pigmented skin lesions. The risk of a nevus developing into a malignant transformation is the main factor to think about. A variety of treatment options are available for excision of Congenital Melanotic Nevus. The purpose of this paper is to describe a case of congenital melanotic nevus below the lower eyelid treated with surgical excision and reconstruction with Wolfe’s graft. A 72-year-old female reported blackish-brown pigmentation below the left eyelid. The excision of the nevus, reconstruction with a Wolfe’s graft from the neck under local anaesthesia was planned. The use of this approach enables the surgeon to perform the necessary preventive surgery, reducing the risk of melanoma development while simultaneously improving cosmetic appearance and reducing the psychological stress associated with such lesions.
Keywords: Nevus; Transplant; Grafts; Melanoma; Cosmetic surgery
Introduction
Congenital and acquired melanocytic nevi are thought to be precursors to melanomas. These are cutaneous lesions that grow over time and are unesthetic when they appear on the face or other exposed places. Understanding about the malignant potential of these nevi is ambiguous. The odds of acquiring melanoma in patients with pre-existing melanocytic nevi (both congenital and acquired) are different from those without them. A full thickness skin transplant known as a Wolfe graft is frequently used to repair damage caused by the removal of facial skin malignancies in the head and neck region.
Case Description and Results
A 72-year-old female reported to the department complaining of blackish-brown pigmentation below the left eyelid present since birth which had grown to attain the present size (3cm x 3cm). The pigmentation was suspected to be a melanotic nevus. The excision of the nevus with 4mm of clear wound margin, reconstruction with a Wolfe’s graft from the neck under local anaesthesia was planned.
Under aseptic conditions the patient was painted and draped. The border of the nevus was marked using marking ink and 4mm free margin surrounding it was marked. Local anaesthetic was infiltrated in the surroundings of the lesion. The incision was placed along the free margins, blunt dissection was carried out and the entire nevus was excised. The recipient site was measured using a calliper and these measurements were transferred on to the sterile graft site on the lower border of right neck. A full thickness graft or a Wolfe’s graft was harvested from the donor site. Haemostasis at the donor site was obtained using sutures. Double layer closure was done at the donor site with 4-0 vicryl and 5-0 prolene sutures in simple interrupted manner. The graft was transfixed to the recipient site with 5-0 prolene sutures in continuous locking manner. Bactigrass dressing and Bolster (autoclaved sponge) were secured over the graft site with 5-0 prolene suture. Both the donor and recipient site received closed dressings. The excised specimen was sent for Histopathology. Post operative instructions were given and the patient was asked to revert back after 7days for suture removal and follow up. On the 8th post operative day the bolster sutures were removed and wound margins were cleaned with spirit and betadine, histopathology reported it to be a congenital melanotic nevus. The patient was asked to revert back after every 2 days for follow up. On the 10th post operative day the wound was examined, there was a haematoma collection beneath the skin. The haematoma was evacuated by placing nicks over the skin layer of graft. Due to poor patient compliance on the 15th post operative day there was haematoma collection beneath the skin graft. The skin over the graft had turned black and stony hard. The haematoma was evacuated and the skin was peeled off. On examination the subcutaneous tissue of the graft was accepted along the 2/3 of the periphery of the wound with raw wound bed at the centre of the recipient site. The wound was cleaned with surgical spirit and betadine and closed dressing with Bactigrass was placed every alternative day. On the 20th postoperative day, the periphery along with centre of the wound showed ingrowth of granulation tissue suggestive of healing. The sutures at the periphery of the wound were removed. Every 3 days the dressing was changed for the patient. On 45th post operative day the recipient site had healed completely with normal skin covering over it. Despite the fact that we lost the graft's superficial skin, there was no ectropion in our situation.

Figure 1: Preoperative margin of the lesion.
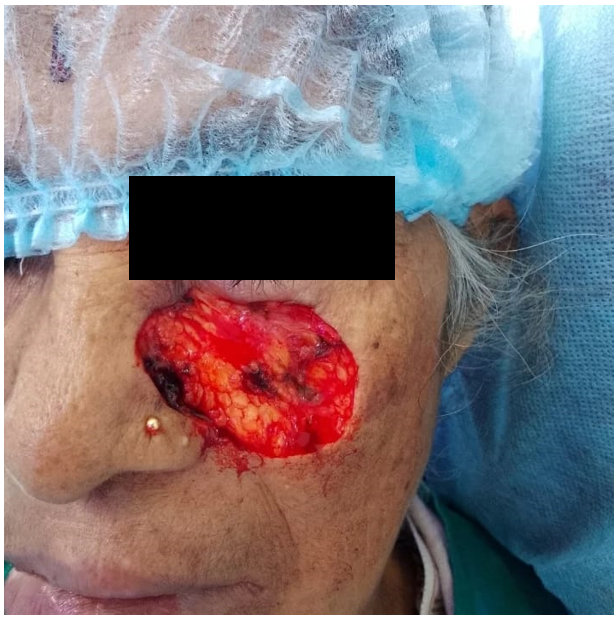
Figure 2: Intra operative picture of the recipient site.

Figure 3: Transfer of measurements onto the graft site.

Figure 4: Donor site post graft excision.

Figure 5: Transfixation of graft to the recipient site.

Figure 6: 15th post operative day.

Figure 7: 20th post operative day with in growth of granulation tissue in the wound.

Figure 8: 45th post operative day.
Discussion
A person's daily life is impacted by the face because it is an essential component of human appearance. Congenital nevi are lesions that expand over time and make the face aesthetically unpleasant. Between 1 and 6% of all newborns have congenital melanocytic naevi (CMN) at birth [1]. Malformations of the neuroectoderm, which contains melanocytes and occasionally neural components, lead to their development after dysregulated growth and halt of melanocytes migration to the skin from the neural crest [2]. They are typically subclassified based on size. They are susceptible to malignant transformation, but the psychological effects of prominent CMNs may be of greater concern [3,4]. When evaluating potential CMN treatment options, numerous criteria must be taken into account. The risk of a nevus developing into a malignant transformation is the main factor to think about. Studies suggest that the chance of developing melanoma varies based on the size of the CMN, and ranges from 0.05% to 10.7%.[3] Additionally, one must not undervalue how the patient may be affected psychologically or cosmetically from childhood through adulthood. As of now, there are treatment options such as laser therapy, dermabrasion, curettage, chemical peels, and total surgical excision with defect restoration [4]. The treatment option for this case was surgical excision of the nevus with reconstruction with a full thickness flap. Defect can be reconstructed with full or split-thickness skin graft. Method of choice of the graft type has been much debated question; however, sufficient number of studies reported good results with Full Thickness Skin Graft (FTSG) due to its presence of more dermis and subsequent less contraction. The draw backs of skin grafting are contracture, colour difference, scar formation and donor site injuries. Due to the fact that FTSG contracts by at least a third, special attention should be paid to grafts that are larger than the defect. For face surgery, these grafts are frequently employed with positive aesthetic outcomes. In this case, the graft was not completely accepted at recipient site due to poor patient follow up and minimal scarring was observed in the nasolabial region.
Conclusion
The surgical procedure of nevus excision promotes quick epithelialization with suitable scar pigmentation and offers a simple, secure and verified one-step means of removing the melanocytic pigmented load of CMN. This technique enables the surgeon to undertake the required pre-emptive surgery, limiting the chance of melanoma formation, while also enhancing the cosmetic look and perhaps lowering the psychological stress related to such lesions.
Conflicts of interest: There are no conflicts of interest to disclose.
References
- Helmbold P, Rompel R, Petres J, D Lübbe, WC Marsch. Kongenitale melanozyta¨re Na¨vi. Hautartz, 1999; 50: 779e84.
- Betti R, Inselvini E, Vergani R, Crosti Small Congenital Nevi Associated with Melanoma: Case Reports and Considerations. The Journal of Dermatology, 2000; 27: 583-590.
- O’Neill TB, Rawlins J, Rea S, Wood F. Treatment of a large congenital melanocytic nevus with dermabrasion and autologous cell suspension (ReCELL): A case report Journal of Plastic, Reconstructive & Aesthetic Surgery, 2011; 64: 1672-e1676
- Kinsler VA, Birley J, Atherton DJ. Great Ormond street hospital for children registry for congenital melanocytic naevi:prospective study 1988e2007. Part 1 e epidemiology, phenotype and outcomes. Br J Dermatol, 2009; 160(1): 143e50.
- Marghoob AA. Congenital melanocytic nevi. Evaluation manages. Dermatol Clin, 2002; 20: 607e16.
- Whang K, Kim M, Song W, Cho S. Comparative treatment of giant congenital melanocytic nevi with curettage or Er:YAG laser ablation alone versus with cultured epithelial autografts. Dermatol Surg, 2005; 31: 1660e7.
- Krengal S, Hauschild A, Scha¨fer T. Melanoma risk in congenital melanocytic naevi: a systematic review. Br J Dermatol, 2006; 155: 1e8.
- M Proctor, R Banks, A Burns, J Ryan. Wolfe Graft: Monitoring Success; j. bjoms, 2017; 8: 106.
- Jovanovic N, Dizdarevic A, Dizdarevic N, Haracic A, GafurovicL. Case report of Wolfe grafting for the management of bilateral cicatricial eyelid ectropion following severe burn injuries. Annals of Medicine and Surgery, 2018; 34: 58-61.
- Juan Sun MD. Staged excision of a cheek congenital melanocytic nevus: a case report and literature review. J Cosmet Dermatol, 2022; 21; 4605-4608.

