Angioid Streaks Secondary to Pseudoxanthoma Elasticum: About Two Cases
Salaheddine Bouabbadi*
Ophthalmology, Avicenne Military Hospital of Marrakech, Mohammed V University, Morocco
Received Date: 18/09/2023; Published Date: 20/02/2024
*Corresponding author: Salaheddine Bouabbadi, Ophthalmology, Avicenne Military Hospital of Marrakech, Mohammed V University, Rabat, Morocco
Introduction
Angioid streaks are an irregular breaklines in Bruch membrane, radiating from the papilla, secondary to alteration of the elastic layer due to calcium overload. The major complication is the development of choroidal neovessels, which are particularly severe.
This bilateral, often asymmetrical and usually progressive disease, was first described by Knapp in 1892.
Angioid streaks are often observed in the context of general pathologies, in particular pseudoxanthoma elasticum, found in 53 to 65% of cases [1,2], an autosomal recessive disease caused by the mutation of the ABCC6 gene [3].Other diseases with which angioid streaks may be associated include, Paget's disease (of unknown origin), sickle cell disease (autosomal recessive inheritance), senile elastosis of the skin, certain vascular disorders associated with arterial hypertension, and more rarely Ehlers-Danlos syndrome (autosomal dominant inheritance).
Here, we report two cases of angioid streaks secondary to pseudoxanthoma elasticum.
Case Report
Case 1:
A 36-year-old man, with no significant medical history, he consults for a rapidly progressive decrease in visual acuity in both eyes, associated with metamorphopsia. Ophthalmological examination finds a best-corrected visual acuity of 4/10, P4 in the right eye, and 2/10, P4 in the left eye, the anterior segment was free of abnormalities with ocular tonus at 15 mm Hg in both eyes. Fundus examination revealed the presence of bilateral angioid streaks associated with granular pigment abnormalities called ‘’Peau d’orange’’ appearance in the temporal retina (Figure 1).
Fluorescein angiography (FA) confirmed the diagnosis of angioid streaks complicated by neovessels in both eyes (Figure 2). Optical coherence tomography reveals fusiform hyperreflectivity in front of the pigment epithelium-choriocapillaris complex with cystoid macular edema and serous retinal detachment.
As part of the etiological assessment, the dermatological and anatomopathological examination confirmed the diagnosis of PXE.
Treatment was based on intravitreal injection (0.5 mg or 0.05 ml) of ranibizumab.
Case 2:
A 40-year-old man, with no significant medical history, he consults for myodésopsies.
Ophthalmological examination finds visual acuity at10/10, P2 in both eyes, the anterior segment was free of abnormalities with ocular tonus at 17 mm Hg in both eyes. Fundus examination revealed the presence of bilateral angioid streaks with exudates, associated with granular pigment abnormalities called ‘’Peau d’orange’’ appearance in the temporal retina (Figure 3).
Optical coherence tomography shows a normal anterior retinal profile line (preservation of the foveolar depression) in both eyes, with presence of a small uplift of the pigment epithelium, associated with a layer of subretinal fluid.
As part of the etiological assessment, dermatological examination showed the presence of papules and micropapules grouped in placards on the lateral surfaces of the neck and external genitalia. the biopsy confirmed the diagnosis of Pseudoxanthoma Elasticum (Figure 4).
Ophthalmological monitoring was recommended, and urgent consultation in case of macular syndrome, with preventive measures including the avoidance of ocular trauma.

Figure 1: Retinograph: Angioid streaks associated with granular pigment abnormalities called ‘’Peau d’orange’’ appearance in the temporal retina (a,b). Fluorescein angiography: Angioid streaks,appear hyperfluorescent (Window defect),complicated by neovessels in both eyes (c,d).

Figure 2: Bilateral angioid streaks with exudates, associated with granular pigment abnormalities called ‘’Peau d’orange’’ appearance in the temporal retina.
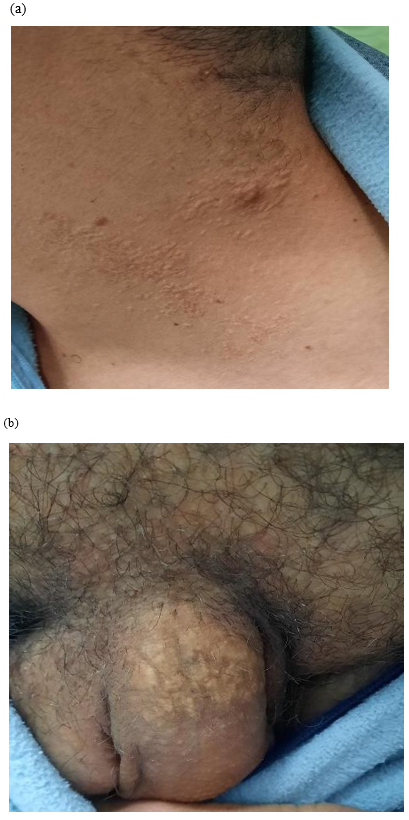
Figure 3: Cobblestone-like appearance of skin lesions at the neck (a) and external genitalia (b) caused by PXE.
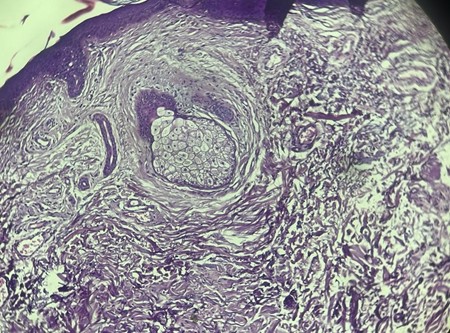
Figure 4: Hematoxylin and esoin stain of a skin biopsy of the second case.
Discussion
Pseudoxanthoma elasticum is a rare autosomal recessive genetic disorder, which prevalence varies between 1/25,000 and 1/100,000 [4], characterized by calcification of elastic tissues, affecting various tissues, cutaneous, vascular, digestive and ophthalmological (angioid streaks). Angioid streaks are present in 85% of patients with elastic pseudoxanthoma [5]. On the fundus, angioid streaks; appearing as darksirregulars lines, starting from the optic disc, interconnected by a ring surrounding the optic disc, with a radial arrangement, and the‘’Peau d’orange’’ appearance in the temporal retina, are characteristics of pseudoxanthoma elasticum, such is the case of our patients.On fluorescein angiography, the angioid streaks appear non-homogeneous and hyperfluorescent throughout the entire sequence, without diffusion [6].
As ophthalmic lesions associated with pseudoxanthoma elasticum, angioid streaks develop in most patients, and the risk of neovascularization increases with age [7]. The frequency of non-exudative macular neovascularization is 33.3%[8]. Bilateralization is common (42-60%), asis the case in our two patients.
Preserving visual function and avoiding complications are the main goals of treatment.
Angioid streaks remain asymptomatic in the absence of neovascularization, and require no treatment other than regular ophthalmological monitoring [9]. However, prevention is recommended, in particular the avoidance of eye trauma [9,10].
Previously, many therapies have been proposed but without any visual benefit in the majority of cases. Argon laser photocoagulation has long been proposed for the treatment of extrafoveolar neovessels,with disappointing results and frequent recurrences (88% at 5 years) [9], and the retreatment was the norm [9,11]. Photodynamic therapy (PDT) has also been used to treat extra-, juxta- and retrofoveolar neovessels, but often without significant functional results [9,11,12].
Based on the results and efficacy of intravitreal injections of anti-VEGF, in the treatment of new vessels complicating age-related macular degeneration and high myopia [13,14], publications regarding the treatment of newvessels complicating angioid streaks by anti- VEGF IVTs, appeared in 2006 [9].
Recently, other studies have shown stabilization or improvement of visual acuity after intravitreen injection of anti-VEGF. Finger et al. reported in their prospective study of seven patients with PXE with CNV, who received IVT of anti-VEGF, an improvement in visual acuity, regression of CNV on AGF and a decrease in foveolar thickness on OCT, without recurrence with a follow-up of three months [3]. In their study of 35 eyes, Mimoun et al. found, an improvement in visual acuity in 85.7% of eyes, a stabilization or decrease in macular
thickness in 51.5% of eyes, and absence of activity on AGF in 65.7% of eyes in the six months following the last IVT [12]. Weigand et al. revealed, in their series, a regression of centromacular thickness averaging 67m after IVT, with complete resolution of subretinal fluid, with the exception of a single patient [15].Sawa et al. evaluated the efficacy of anti-VEGF IVTs in a retrospective study involving 15 eyes. Two-line VA improvement was noted in 33% of eyes, stabilization in 54% and worsening in 13% of cases. Angiographic follow-up showed the absence of neovascular reactivation in 67% of eyes [16].
The natural evolution of neovessels complicating the angioid streaks is extremely severe, and anti-VEGF IVTs have shown their effectiveness in our patient, which is consistent with the results of various studies.
Conclusion
Pseudoxanthoma elasticum is a rare genetic disorder characterized by calcification of the elastic fibers of the skin, retina and cardiovascular system, threatening especially the vital and visual prognosis.There is no specific treatment for angioid streaks. Anti-VEGF IVT is the only treatment capable of stabilizing or even improving vision in the case of neovessels associated with angioid streaks, while preserving the integrity of retinal structures as far as possible.
References
- Archer DB, Logan Angioid streaks. Hereditary retinal and choroidal diseases. Clinical characteristics vol. 2. Hagerstown: Harper and Row; 1976; p. 851-909.
- Neldner Pseudoxanthoma elasticum. Clin Dermatol, 1988; 6: 1-159.
- Finger RP, Charbel Issa P, Hendig D, Scholl HP, Holz FG. Monthly ranibizumab for choroidal neovascularizations secondary to angioid streaks in pseudoxanthoma elasticum: a one-year prospective Am J Ophthalmol, 2011; 152: 695-703.
- Finger Monthly Ranibizumab for choroidal neovascularizations secondary to angioid streaks in pseudoxanthoma elasticum: a one-year prospective study. Am J Ophthalmol, 2011; 152: 695-703.
- Connor PH, Juergens JL, Perry HO, Hollenhorst RW, Edwards Pseudoxanthoma elasticum and angioid streaks: a review of 106 cases. Am J Med, 1961; 30: 537-543.
- Finger RP, Charbel Issa P, Ladewig M, Gotting C, Holz FG, Scholl Fundus autofluorescence in pseudoxanthoma elasticum. Retina, 2009; 29: 1496-1505.
- Risseeuw S, Ossewaarde-van Norel J, van Buchem C, Spiering W, Imhof SM, van Leeuwen R. The extent of angioid streaks correlates with macular degeneration in pseudoxanthoma Am J Ophthalmol, 2020; 220: 82–90.
- Marques JP, Bernardes J, Geada S, et non-exudative macular neovascularization in pseudoxanthoma elasticum. Graefes Arch Clin Exp Ophthalmol, 2021; 259(4): 873–882.
- Souied E, Quentel G, Cohen Dégénérescence maculaire liéeà l’âge Myopie et étiologies de la néovascularisation choroï-dienne/sous la direction de Salomon Yves Cohen et GabrielQuentel. Paris: Médecine Sciences Publications Lavoisier, 2012.
- FajardoSánchez J, Chau Ramos CE, Mazagatos Used PJ, Aparicio Hernandez-Lastras The effect of the accelera-tion/deceleration trauma in angioid streaks: a pathogenichypothesis. Arch Soc Espanola Oftalmol, 2016.
- Wolff B, Sahel JA, Mateo-Montoya A, Mauget-Fa¨ysse M, BaillifS, Le Mer Traitement par injection intravitréenne de rani-bizumab de néovaisseaux choroïdiens compliquant des striesangioïdes: à propos d’un cas. J Fr Ophtalmol, 2013; 36: e5-e9.
- Mimoun G, Tilleul J, Leys A, Coscas G, Soubrane G, Souied EH. Intravitreal ranibizumab for choroidal neovascularizationin angioid Am J Ophthalmol, 2010; 150: 692—700.e1.
- Querques G, Azrya S, Martinelli D, Berboucha E, FeldmanA, Pece A, et Ranibizumab for exudative age-relatedmacular degeneration: 24-month outcomes from a single-centre institutional setting. Br J Ophthalmol, 2010; 94: 292-296.
- Lalloum F, Souied EH, Bastuji-Garin S, Puche N, QuerquesG, Glacet-Bernard A, et Intravitreal ranibizumab for choroi-dal neovascularization complicating pathologic myopia. Retina Phila Pa, 2010; 30: 399-406.
- Wiegand TW, Rogers AH, McCabe F, Reichel E, Intravitreal bevacizumab (Avastin) treatment of choroidalneovascularisation in patients with angioid streaks. Br J Oph- thalmol, 2009; 93: 47-51.
- Sawa M, Gomi F, Tsujikawa M, Sakaguchi H, Tano Long-term results of intravitreal bevacizumab injection for choroidal neovascularization secondary to angioid streaks. Am J Ophthalmol, 2009; 148: 584-590.

