A Devastating Illness: Necrotizing Fasciitis
Yesenia Brito1,*, Nawal Majid1, Bruce Wilson1, Abshiro H Mayow1, Frederick Tiesenga2 and Juaquito Jorge2
1Saint George’s University School of Medicine, Grenada
2Department of Surgery, Community First Medical Center, Grenada
Received Date: 05/09/2023; Published Date: 06/02/2024
*Corresponding author: Yesenia Brito, Saint George’s University School of Medicine, Grenada
Abstract
Necrotizing Fasciitis (NF) is a rare but life-threatening bacterial infection that can quickly destroy skin and soft tissues. Its symptoms can vary from subacute to hyperacute, which often leads to misdiagnosis. Due to its high mortality and morbidity rate, accurate diagnosis and prompt medical and surgical intervention are crucial in preventing the disease from worsening. Early surgical intervention has been found to reduce hospital stay in severe cases of NF.
We present a case of a 55-year-old female with an extensive medical history. The patient arrived at the Emergency Department (ED) with abdominal pain and swelling after a scratch. The medical team suspected NF, promptly intervened with a multidisciplinary approach, including antibiotic, wound debridements, and close postoperative monitoring. This case report highlights the importance of a comprehensive approach in treating severe NF, particularly in comorbid patients with poor prognosis.
Keywords: Necrotizing Fasciitis; Abdominal Wall Necrotizing Fasciitis; Urgent Debridement; Broad Spectrum Antibiotics
Introduction
NF is the infection of the subcutaneous tissue that invades the fascia and fat due to poor blood supply [1]. Initially, the overlying tissue may remain unaffected, which can result in delayed diagnosis and potential misdiagnosis [1]. By the time diagnosis has been made, the infection can spread, causing extensive systemic toxicity and organ damage [2]. As a result, the mortality rate exceeds 70% before treatment [2]. Appropriate and timely treatment can reduce the mortality rate to 11.6% in patients with NF [3].
Diagnosis is primarily clinical, however magnetic resonance imaging (MRI) and lab values may be used to aid diagnosis if clinical findings are equivocal [1,4]. A Computer Tomography (CT) can also be useful in diagnosing NF, especially in cases where MRI is not readily available [5]. A biopsy taken during debridement is the gold standard for both, diagnosis and confirmation of the condition [6]. Clinical concern for necrotizing fasciitis requires prompt surgical evaluation.
Differential diagnosis includes cellulitis, pyoderma gangrenosum, gas gangrene, pyomyositis, and deep venous thrombosis.
Less than an hour after her presentation to the ED, our patient was taken to the Operating Room (OR). However, her symptoms had started two weeks prior. Her medical history includes obesity and diabetes. The delay in seeking treatment as well as prior medical conditions created a presentation which required prolonged treatment in the intensive care unit and multiple debridements. The combination of delayed care and multiple comorbidities makes this case noteworthy for further study.
Case Presentation
We present a case of a 55-year-old female with a body mass index (BMI) of 51.1. Her past medical history is significant for diabetes mellitus, hypertension, hyperlipidemia, depression and laparoscopy hysterectomy with salpingo-oophorectomy in 2016 for endometrial carcinoma. She presented to the Emergency Department (ED) complaining of a two-weeks history of abdominal pain, swelling and redness following a scratch. The pain had been progressive and worse on the right lower quadrant. The patient had associated symptoms of shortness of breath, frequent dry cough and weakness. She also reported falling twice over the past few days. Injuries were denied, but she was unable to get up for 20 minutes.
During the examination, her vital signs gave cause for concern. Her blood pressure (BP) recorded was 96/61 mm Hg, heart rate was 110 beats per minute, temperature was 100.7 F, respiration rate was 22 breaths per minute and pulse oximeter was 92% on room air. Abdominal examination revealed erythema and warmth of the majority of pannus, without extension to the pelvic area.
There was also an area that appeared flocculant with some greenish discoloration (Figure 1), and severe right lower quadrant tenderness.
On admission, blood work showed multiple abnormalities (Table 1), including: severe leukocytosis, hyponatremia, subpar renal function, mild troponin, lactic acidosis and rhabdomyolysis. Given the concern for necrotizing fasciitis, broad-spectrum antibiotics were administered. Vancomycin 2000 mg, piperacillin/tazobactam 3.375 g and clindamycin 600 mg were given intravenously. The surgery team was consulted, and the patient was taken to the Operating Room (OR) requiring emergent abdominal wall debridement.

Figure 1: Flocculant area measuring 5 cm x 5 cm with greenish discoloration of the abdominal wall.
Table 1: Laboratory values on admission.
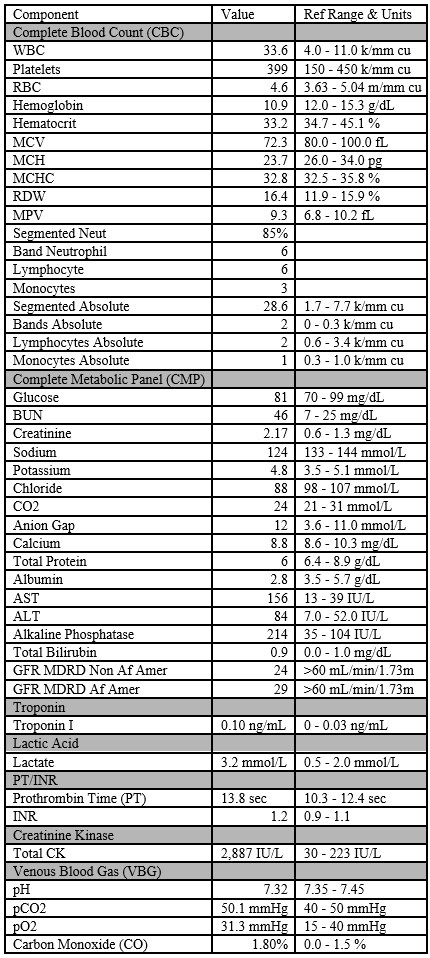
GFR MDRD Non Af Amer*: Glomerular Filtration Rate Modification of Diet in Renal Disease in non-African American.
In the operative room, all infected tissue was sharply excised and immediately sent for histological evaluation. Approximately 50 x 70 cm in dimension of the abdominal wall was excised, including the fascia. A malodorous, purulent collection was noted. Cultures were taken, and the collection was drained. The extent of deep penetration into the fascia and potential involvement beyond it was challenging to determine due to the substantial inflammation present. The patient was taken to the ICU intubated for mechanical ventilation and further management.
Although the histopathology report indicated the absence of malignancy, the cultures showed the growth of Methicillin-Resistant Staphylococcus Aureus (MRSA) and Peptoniphilus. The blood cultures were negative.
On postoperative day (POD) one, a computed tomography (CT) of the abdomen and pelvis revealed a residual abscess in the medial midline above fascia (Figure 2). The patient was taken emergently to the OR for re-exploration and debridement of the abdominal wound (Figure 3).

Figure 2: Large soft tissue defect along the anterior pelvic subcutaneous tissue and skin along the right side with small air. (A) A fluid collection approximately 8.1 cm in the pelvic wall musculature, (B) 7.8 cm in transverse dimension by (C) 2.4 cm in AP dimension.

Figure 3: Anterior abdominal wall post re-exploration and debridement.
During wound examination, two days post her second debridement, ongoing necrotic tissue was noted as well as a fascial defect. A third abdominal debridement was performed. A Wound Vaccum-Assisted Closure (VAC) was placed on the wound to promote the growth of healthy tissue. Although white blood cells had increased from previous encounters, no new infection was found. Operative cultures were negative.
On day eight, post third debridement, small scattered areas of necrosis throughout the abdominal wound were found. Excisional re-debridement of the abdominal wound was performed, and new wound VAC was placed.
The patient continued to receive mechanical ventilation, and vasopressors following multiple complex abdominal debridement and wound VAC placements (Figure 4). Following evaluation, the patient was discharged to Kindred Hospital for long term care. To ensure the best possible outcomes for the patient’s, recovery, close monitoring and appropriate care are recommended.

Figure 4: Wound after wound VAC removal 5 days after patient’s fourth debridement. An increase in blood flow to the wound area as well as growth of healthy tissues can be appreciated.
Discussion
The major causes of NF are classified into two groups [2]. Type one is caused by polymicrobial organisms that are anaerobic and aerobic [2]. This type targets the elderly as well as those with comorbidities, including: diabetes, gynecologic procedures, and malignancies [2]. Type two are monomicrobial organisms, mainly due to Group A Streptococcus or Staphylococcus aureus [2].
This group targets all ages and those who do not have prior illnesses [2]. Overall, type two infections consist of about 55 to 87% of the total cases, but some studies portray the incidence of both types to be similar [2]. Patients with methicillin-resistance Staphylococcus aureus (MRSA), have worse outcomes compared to those caused by other pathogens or no pathogens identified [7,8]. MRSA-associated NF can result in several outcomes, including a high rate of amputation, longer hospital stays, and higher mortality [7,8].
The onset of the infection can start out with a small scratch. Whether it be from trauma, skin infection, IV, or surgeries, it allows bacteria to enter and release its toxins causing tissue destruction [9]. The clinical presentation may include: erythema, swelling, tenderness and eventually cause skin changes with crepitus and fluctuance. Failure to prompt treatment can result in necrosis [9]. The incidence for NF is estimated to be between 0.3 to 15 cases for a population of 100,000 annually [2]. Although anyone can be affected by NF, several risk factors have been identified, including: advanced age, obesity, diabetes, cancer and immunocompromised [9].
The treatment for this condition starts with aggressive and urgent surgical debridement, which is a crucial component of the overall management [6]. Simultaneously, the initiation of empiric antibiotic therapy is crucial and should commence as soon as possible [6]. The initial antibiotic regimen should provide broad spectrum coverage [6]. One effective combination consists of ampicillin, gentamicin, and clindamycin or metronidazole [6]. Another recommended option is ampicillin-sulbactam, ticarcillin-clavulanate potassium, and piperacillin-tazobactam, particularly if there is a suspicion of pseudomonas infection [6]. Imipenem-cilastatin, along with a beta-lactam and beta-lactamase inhibitor, is also a viable choice [6]. However, it is important to re-evaluate the antibiotic regimen once culture data becomes available. Multiple debridements are often necessary in these patients, as occult areas of infection are common and can spread after initial treatment [6]. Therefore, patients should undergo regular assessments for surgical intervention [6].
Early and prompt treatment is associated with lower rates of mortality in cases of necrotizing fasciitis [10]. Patients who undergo surgery within 12 hours of admission have a lower mortality rate compared to those who undergo surgery after 12 hours (16.1 % vs. 50%, p<0.001) [11].
Patients whose debridement is delayed by over 12 hours also suffer increased amputation rates [10]. Sepsis is a common complication, and vasopressors are often required to control hypotension [12]. Even with effective and prompt treatment, mortality rates are high. Patients who receive such treatment still face a mortality rate of at least 20% [12]. Individuals who show signs of streptococcal toxic shock syndrome have a mortality rate of at least 33% [12]. Those who manage to survive the initial infection are more likely to experience premature death [13]. Older age is a significant risk factor for mortality in patients with NF [14]. Patients over the age of 75 have a significant higher mortality rate compared to younger patients (62.5% vs 16.8%, p<0.001) [14].
While surgery and rigorous anti-microbial therapy can help treat NF, unfortunately, 1 in 5 people succumb to the infection [12]. Patients who survive NF should be treated pertaining to their risk factors and encouraged to make life-style changes to minimize complications. Modifiable risk factors include: obesity, diabetes, smoking, and atherosclerotic disease. Female sex predisposes patients to reduced post-disease survival, although the reason is unknown [13]. Overall, adequate treatment prevents numerous complications associated with NF including acute kidney injury, organ failures, limb amputation, arrhythmias, sepsis and even death.
Conclusion
Necrotizing fasciitis is a serious medical and surgical emergency that demand immediate treatment to prevent fatality. Its association with high mortality and morbidity rates in patients with comorbid conditions, such as diabetes, hypertension, cancer, and liver disease. Despite having a complex medical history, this patient was treated using an interdisciplinary approach. She received an immediate diagnosis, and a prompt medical management, resulting in a stable outcome. Caution and prompt decision-making when caring for immunocompromised patients who present signs and symptoms of NF is crucial, as such patients have poor prognosis.
Author Contributions
Yesenia Brito: Concept and Design of study, Acquisition of data, drafting article, revising article. Guarantor Author
Nawal Majid: Concept and Design of study, drafting article intellectual content, revising article
Bruce Wilson – Acquisition of data, drafting article, revising article
Abshiro H Mayow: Acquisition of data, drafting article, revising article
Rederick Tiesenga: Final Approval, Intellectual Content, revising article
Juaquito Jorge: Final Approval, Intellectual Content, revising article
Informed Consent: A signed statement of informed consent was obtained for publication of the details of this case
Competing Interests: None
Grant Information: None
References
- Wallace HA, Perera Necrotizing Fasciitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023.
- Stevens DL, Bryant AE. Necrotizing soft-tissue infections. New England Journal of Medicine, 2017; 377(23): 2253-2265.
- Wong CH, Chang HC, Pasupathy S, Khin LW, Tan JL, Low Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. JBJS, 2003; 85(8): 1454-1460.
- Loh NN, Ch'en IY, Cheung LP, Li Deep fascial hyperintensity in soft-tissue abnormalities as revealed by T2-weighted MR imaging. AJR Am J Roentgenol, 1997; 168: 1301-1304. 10.2214/ajr.168.5.9129430
- Paz Maya S, Dualde Beltrán D, Lemercier P, Leiva-Salinas Necrotizing fasciitis: an urgent diagnosis. Skeletal radiology, 2014; 43: 577-589.
- Headley Necrotizing soft tissue infections: a primary care review. Am Fam Physician, 2003; 68(2): 323-328. PMID: 12892352.
- Goh T, Goh LG, Ang CH, Wong Early diagnosis of necrotizing fasciitis. Br J Surg, 2014; 101(1): e119-25. doi: 10.1002/bjs.9371. Epub 2013 Nov 29. PMID: 24338771.
- Lemsanni M, Najeb Y, Zoukal S, Chafik R, Madhar M, Elhaoury Necrotizing fasciitis of the upper extremity: a retrospective analysis of 19 cases. Hand Surg Rehabil, 2021; 40(4): 505-512. doi: 10.1016/j.hansur.2021.02.004. Epub 2021 Mar 31. PMID: 33812083.
- Hakkarainen TW, Kopari NM, Pham TN, Evans HL. Necrotizing soft tissue infections: review and current concepts in treatment, systems of care, and Curr Probl Surg, 2014; 51(8): 344-362. doi: 10.1067/j.cpsurg.2014.06.001. Epub 2014 Jun 12. PMID: 25069713; PMCID: PMC4199388.
- Sudarsky LA, Laschinger JC, Coppa GF, Spencer Improved results from a standardized approach in treating patients with necrotizing fasciitis. Ann Surg, 1987; 206: 661-665. 10.1097/00000658-198711000-00018
- Su YC, Chen HW, Hong YC, Chen CT, Hsiao CT, Chen Laboratory risk indicator for necrotizing fasciitis score and the outcomes. ANZ J Surg, 2008; 78(11): 968-972. doi: 10.1111/j.1445-2197.2008.04713.x. PMID: 18959694.
- CDC
- Timothy D Light, Kent C Choi, Timothy A Thomsen, et al. Journal of Burn Care & Research, 31: 93-99.
- Lancerotto L, Tocco I, Salmaso R, Vindigni V, Bassetto Necrotizing fasciitis: classification, diagnosis, and management. J Trauma Acute Care Surg, 2012; 72(3): 560-566. doi: 10.1097/TA.0b013e318232a6b3. PMID: 22491537.

