Melkersson-Rosenthal Syndrome: A Rare Entity Not to Be Ignored
Hajar El Bennaye*, Zakia Douhi, Hanane Baybay, Meryem Soughi, Sara Elloudi and Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II, Morocco
Received Date: 06/09/2023; Published Date: 31/01/2024
*Corresponding author: Dr. EL BENNAYE Hajar, Department of Dermatology, University Hospital Hassan II, Fes, Morocco
Introduction
Melkersson-Rosenthal Syndrome (MRS) is a rare clinical entity defined by the triad of orofacial edema, recurrent facial paralysis and fissured tongue. This triad may be incomplete or appear at different times [1,2]. We describe the case of two patients with chronic and recurrent macrocheilitis, diagnosed as Melkersson-Rosenthal syndrome.
Observation 1
This 35-year-old patient, with no previous pathological history, had presented for 5 years with persistent labial edema, predominantly in the upper lip, with paroxysmal episodes of aggravation occurring without any obvious triggering factor and not accompanied by laryngeal edema or other allergic signs. On examination, there was no change in general condition, no digestive signs and no joint symptoms. Examination revealed edema of the upper lip with an elastic consistency (Figure 1), associated with facial asymmetry and a puckered tongue (Figure 2). The rest of the examination was unremarkable. Skin biopsy revealed a lymphocytic inflammatory infiltrate with no specific lesion.

Figure 1: Clinical image showing macrocheilitis with facial paralysis.
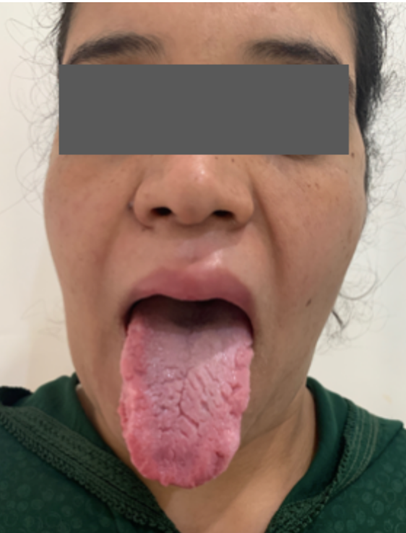
Figure 2: Clinical image of fissured tongue.
Observation 2
A 30-year-old patient with no previous pathological history presented with labial edema that had been evolving for 4 years. Clinical examination revealed erosive machrochleitis and sequelae of facial asymmetry associated with a puckered tongue. Labial biopsy revealed an epithelioid granuloma without caseous necrosis and a lymphocytic inflammatory infiltrate. Assessment for sarcoidosis was negative.
Discussion
Melkersson-Rosenthal syndrome is a rare primary or secondary granulomatosis, inconsistently associated with facial paralysis that may be delayed in time, and a grooved tongue appearance. However, it presents a wide variety of clinical symptoms. It appears in young adults between the 2nd and 4th decade of life, with no predilection for race or sex in our patients, although some authors claim a female predominance. Indeed, in the majority of cases, the cardinal signs of the disease do not present synchronously, but appear successively, which explains the delay in diagnosis. This is a relatively benign condition, which is only exceptionally life-threatening, but often causes significant cosmetic damage, as was the case in our patient [3].
Treatment of SMR appears to be a challenge, with several drugs having been used including corticosteroid therapy, which may not be effective and, in this case, cyclins may be used. Some authors have resorted to facial and optic nerve decompression surgery in cases of severe damage, and to plastic surgery [4].
Conclusion
Our cases illustrate the typical clinical presentation of histologically confirmed Melkersson-Rosenthal syndrome, as well as the efficacy of oral corticosteroid therapy in the treatment of flares and intralesional corticosteroid therapy for macrocheilitis [3].
References
- Domaneschi C, Arruda CFJ, Carvalho VJG, Santos RLO, Sugaya NN. Melkersson-Rosenthal syndrome: a classical case report. RGO, Rev Gaúch Odontol, 2023; 71: e20230019. http://dx.doi.org/10.1590/1981-86372023001920200005
- Tang J-J, Shen X, Xiao J-J, Wang X-P. Retrospective analysis of 69 patients with Melkersson-Rosenthal syndrome in mainland China. Int J Clin Exp Med, 2016; 9(2): 3901-3908.
- Wehl G, Rauchenzauner M. A Systematic Review of the Literature of the Three Related Disease Entities Cheilitis Granulomatosa, Orofacial Granulomatosis and Melkersson - Rosenthal Syndrome. Curr Pediatr Rev, 2018; 14(3): 196-203.
- Dhawan SR, Saini AG, Singhi PD. Management Strategies of Melkersson-Rosenthal Syndrome: A Review. Int J Gen Med, 2020; 13: 61-65.

