Ileo-Ileal Intussusception Secondary to Meckel's Diverticulum
Amal Hajri, Kabira Falousse*, Mounir Bouali, Abdelilah El-Bakouri, Khalid El-Hattabi, Fatima Zahra Bensardi and Abdelaziz Fadil
Department of Visceral Surgical Emergency, Faculty of Medicine and Pharmacy, University Hospital Center Ibn Rochd, Hassan II University, Casablanca, Morocco
Received Date: 02/09/2023; Published Date: 25/01/2024
*Corresponding author: Kabira Falousse, Department of Visceral Surgical Emergency, Faculty of Medicine and Pharmacy, University Hospital Center Ibn Rochd, Hassan II University, Casablanca, Morocco
Abstract
Introduction: Intussusception secondary to Meckel's diverticulum is a rare entity in adults and can therefore be difficult to diagnose accurately preoperatively.
Case Report: We present the case of a 43-year-old patient who presented to the emergency department with an occlusive syndrome evolving for 5 days. Clinical examination revealed a distended, tympanic abdomen with a normal rectal exam, The PSA showed grelic hydroaeric levels, and the abdominal CT scan revealed a grelic intussusception in the right iliac fossa, with occlusion beginning upstream. The patient underwent emergency surgery, and was found to have a grelo-grelic intussusception secondary to a meckel diverticulum.
Discussion: Meckel's diverticulum results from incomplete obliteration of the vitelline or omphalomesenteric duct, which connects the developing intestines to the yolk sac. It occurs in around 2% of the population, of whom only around 4% may become symptomatic due to a number of complications. Specifically, small bowel obstruction and diverticulitis secondary to ectopic gastric or pancreatic tissue are the most common presentations of symptomatic DM.
Conclusion: Although relatively rare in adults, Meckel's diverticulum should be considered in the list of differentiations in patients with intussusception leading to acute intestinal obstruction.
Keywords: Intussusception; Meckel's diverticulum; Small bowel; Surgery
Introduction
Meckel's diverticulum is the most common congenital anomaly of the small intestine, originally described by Fabricius-Hildanus in 1598. However, it is named after Johann Friedrich Meckel, who established its embryonic origin in 1809, with a prevalence of around 1-3% [1-3]. It arises from a persistent remnant of the omphalomesenteric duct [4,5], which usually involutes during the fifth week of gestation, but various anomalies, including fistulae, sinuses, cysts or diverticula, may remain if this process is incomplete [2]. It is located on the anti-mesenteric border of the terminal ileum, less than 60 cm from the ileocecal junction, and averages 5 cm in length [6]. Complications of Meckel's diverticulum are more frequent in children and diminish with age. An exceptional complication is intussusception, manifested by signs of intestinal obstruction. In this article, we present the case of an adult with ileo-ileal intussusception caused by an inverted Meckel diverticulum.
The work has been reported in line with the SCARE criteria [15].
Case Report
A 43-year-old patient, treated for depression for a year on anxiolytics and antidepressants, presented to the digestive surgery emergency department with an occlusive syndrome consisting of vomiting, right iliac fossa pain and cessation of matter and gas, evolving for 5 days in a context of preserved general condition, On clinical examination, the patient was stable, BP 140/70 mmHg, heart rate 87 Bpm, respiratory rate 24 cpm, abdomen distended, tympanic and tender, rectal examination unremarkable and hernial orifices free.
The patient underwent an unprepared abdomen, which revealed large hydroaerosic levels.

Figure 1: Abdominal x-ray showing dilated small bowel loops with gas-fluid levels.
abdominal CT scan revealed a cocoon formation of 2 digestive structures measuring 113*39 mm, with distension of the upstream bowel measuring 34 mm, site of hydroaeric levels, laboratory tests showed Hb:14.7g/dl
WBC: 15000 /mm3 CRP: 241.6 mg/L Albumin: 40 mg/L
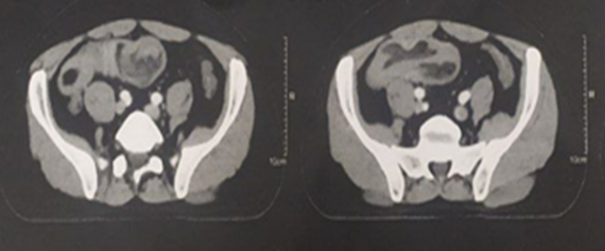
Figure 2: Abdominal CT showed invagination of MD (arrowhead).
The patient received a nasogastric tube aspiration with venous rehydration, and it was then decided to operate urgently, under general anaesthesia and endotracheal intubation, with administration of prophylactic antibiotics. The patient was approached via a median laparotomy, with exploration revealing a bowel obstruction 3m 70 from the ADJ and 50 cm from the JIC, upstream of a grelo-below intussusception. After deinvagination, an intussusception secondary to a Meckel diverticulum was found, and a 50-cm segmental bowel resection was performed, removing the intussusception with terminal grelogrelic anastomosis, Post-operative follow-up was straightforward, and the patient was declared discharged after resumption of transit.

Figure 3: intraoperative image showing ileoileal invagination.

Figure 4: Opening of the operating room reveals a meckel diverticulum.
The operative specimen was sent for histopathology, which confirmed the diagnosis of a true Meckel's diverticulum of the small intestine.
Discussion
During fetal life, the yolk duct (omphalomesenteric) connects the midgut to the yolk sac. Between 5◦ and 7◦ weeks' gestation, the duct obliterates and becomes a fibrous band connecting the umbilicus to the intestine, which is eventually completely absorbed. In the absence of obliteration in the proximal part of the yolk duct, an intestinal evagination called Meckel's diverticulum forms [7,8].
Most cases of Meckel's diverticulum are asymptomatic (over 90%), with an estimated lifetime risk of developing complications of around 4% [3,9-11]. Complications include hemorrhage, intussusception, diverticulitis, peptic ulceration and intestinal obstruction [12].
Numerous mechanisms have been proposed to explain intestinal obstruction due to Meckel's diverticulum. Obstruction may be caused by entrapment of an intestinal loop by a mesodiverticular band, volvulus of the diverticulum around a mesodiverticular band, invagination, as well as extension into a hernial sac (Littré hernia) [3].
A study of 754 adults with intussusception showed that around 52% had intussusception in the small intestine, 38% in the large intestine and the remainder in the stomach and duodenum.The etiology of intussusception in the small intestine differs in children and adults, since in children it is often idiopathic, whereas in adults there is often a pathological cause [13].
Preoperative diagnosis of intussusception secondary to Meckel's diverticulum remains a challenge and therefore requires comprehensive data on clinical, pathological, radiological and surgical findings. Clinically, patients with intussusception often present with symptoms that overlap with other types of intestinal obstruction, including vomiting, acute abdominal pain, tenderness and distension. Other clinical signs include fever, mildly elevated white blood cell count, bleeding and a history of recurrent abdominal pain [4-14].
Intestinal obstruction secondary to Meckel's diverticulum often shows dilated coves of the small intestine with multiple hydroaeric levels or intestinal perforation. However, this modality is not very effective in identifying Meckel's diverticulum as the cause of intestinal intussusception. Ultrasound is another modality that can help in the diagnosis of Meckel's diverticulum intussusception. Inverted diverticulum often manifests as a "double target" sign, also known as the donut or bullseye sign. However, CT is the most reliable diagnostic tool for intestinal obstruction, with a better visualized target lesion. The result represents the blocked bowel seen in cross-section with thickening of the bowel wall and mesenteric blockage. It is also sensitive in the diagnosis of intussusception with or without a starting point, enabling management to be directed [4].
Whether all incident Meckel diverticula should be resected in asymptomatic individuals remains controversial. On the other hand, treatment of symptomatic patients should always include resection of the diverticulum or segment of intestine affected by the pathology [3].
Conclusion
We conclude that invagination of Meckel's diverticulum is a rare complication in adults, but should be taken into account in the differential diagnosis of individuals suffering from chronic abdominal pain and intermittent intestinal obstruction. We present here an exceptional form of this complication, in which the diverticulum was inverted.
The consent statements: Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review: Not commissioned, externally peer-reviewed
Conflicts of interest: None
Sources of funding: None
Ethical approval: As per international standard written ethical approval has been collected and preserved by the author(s).
Consent: Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution: This work was carried out in collaboration among all authors. All authors contributed to the conduct of this work. They also declare that they have read and approved the final version ofthe manuscript.
Research registration (for case reports detailing a new surgical technique or new equipment/technology): None
Guarantor: DR L F
References
- Nemeh C, Almaz B, Ko VH, Walsh A, Panasiti R, Gitzelmann CA. Ileoileal intussusception due to Meckel’s diverticulum in a pre-term neonate. Journal of Pediatric Surgery Case Reports, 2023; 88: 102529.
- Lafarge B, Dray X, Boudiaf M, Pocard M. Ileocolic intussusception due to an inverted Meckel’s diverticulum. Dig Liver Dis, 2012; 44(1): e2.
- Ying L, Yahng J moh J. A rare case of Meckel’s diverticulum causing small bowel obstruction in a 50-year-old man. Int J Surg Case Rep, 2020; 68: 107‑110.
- Muneeb A, Nguyen NN, Iqbal F, Bhargava P. Meckel’s diverticulum leading to ileo-ileal intussusception. Radiol Case Rep, 2022; 17(5): 1579‑1582.
- Barry WE, Rosenberg DM, Warren M, Kim ES. Small bowel intussusception secondary to inverted Meckel’s diverticulum. Journal of Pediatric Surgery Case Reports, 2017; 25: 49‑51.
- Almas T, Alsubai AK, Ahmed D, Ullah M, Murad MF, Abdulkarim K, et al. Meckel’s diverticulum causing acute intestinal obstruction: A case report and comprehensive review of the literature. Ann Med Surg (Lond), 2022; 78: 103734.
- Ileo-ileal intussusception due to inverted Meckel’s diverticulum - PubMed [Internet],
- Soria-Céspedes D, Leuchter-Ibarra J, Ventura-Molina V, Mora-Constantino J. Intususcepción ileocólica en un adulto causado por divertículo de Meckel invertido. Revista de Gastroenterología de México, 2012; 77(4): 220‑223.
- Camacho-Guerrero I, Ramírez-Patiño L. Intussusception secondary to Meckel’s diverticulum in a 3-month-old girl. Case report. Rev Med Hosp Gen Mex, 2018; 81: 33‑35.
- Rana NA, Rathore MO, Khan MU. Invaginated Meckel’s diverticulum: a rare cause of small intestine intussusception in adults. J Coll Physicians Surg Pak, 2013; 23(4): 287‑289.
- Milbrandt K, Sigalet D. Intussusception associated with a Meckel’s diverticulum and a duplication cyst. J Pediatr Surg, 2008; 43(12): e21-23.
- Batura D, Saxena V, Mathai S, Sarker S. Meckel’s Diverticulum as A Cause of Ileo-Ileal Intussusception: A Case Report. Medical Journal Armed Forces India, 1998; 54(3): 262‑263.
- Combes AD, Limmer AM, Verschuer K. Small bowel intussusception secondary to Meckel’s diverticulum containing polypoid lesion in pregnancy. ANZ J Surg, 2020; 90(9): 1774‑1776.
- Kassir R, Debs T, Boutet C, Baccot S, Abboud K, Dubois J, et al. Intussusception of the Meckel’s diverticulum within its own lumen: Unknown complication. Int J Surg Case Rep, 2015; 10: 111‑114.
- Agha RA, Franchi T, Sohrabi C, Mathew G, for the SCARE Group. The SCARE 2020 Guideline: Updating Consensus Surgical CAse REport (SCARE) Guidelines, International Journal of Surgery, 2020; 84: 226-230.

