A Successful Single Early Hemodialysis Treatment for a Late-Onset Lactic Acidosis After Metformin Poisoning in a Type 2 Diabetes Patient with Advanced Diabetic Nephropathy
Ayane Nishida1, Osamu Sekine1, Yukako Yamamoto1, Jun Ito-Kobayashi1, Masanori Iwanishi1, Akira Shimatsu1, Ken Kitamura2, Toshiki Nishio2, Daisuke Sato3, Masahiro Fujita3 and Atsunori Kashiwagi1,*
1Department of Diabetes and Endocrinology, Omi Medical Center, Japan
2Department of Nephrology and Dialysis Center, Omi Medical Center, Japan
3Department of Medicine, Division of Diabetology and Nephrology, Shiga University of Medical Science, Japan
Received Date: 28/08/2023; Published Date: 15/01/2024
*Corresponding author: Dr. Atsunori Kashiwagi, Department of Diabetes and Endocrinology, Omi Medical Center, 1660 Yabase, Kusatsu, Shiga 525-8585, Japan
Abstract
We report a case of metformin-induced lactic acidosis from a suicide attempt. At 6:30 am, the patient ingested 35 g metformin (MET) in his hotel room. At 10:00 am he contacted the hotel front desk because of severe nausea and chest discomfort and was transported to our emergency room in a state of disturbed consciousness (GCS 8 points). He had type 2 diabetes (T2DM) with advanced diabetic nephropathy (stage G3aA3). The first laboratory tests at 11:00 am in the emergency room showed poor glycemic control (HbA1c 9.1%) with impaired renal function (eGFR 33.3 mL/min/1.73 m2) without acidosis (pH 7.46) and with a slight increase in plasma lactate (5.8 mmol/L). Fluid infusion and gastric lavage were performed. At 1:00 pm, he was admitted to our intensive care unit. MET-associated lactic acidosis (MALA) was first recognized in laboratory results received at 6:30 p.m.: pH was 7.25, with high (13.1 mmol/L) lactate and low (16.3 mmol/L) bicarbonate. Although those values did not reach the published criteria for introducing hemodialysis therapy, we initiated hemodialysis therapy at 10:00 pm. After a 4-hour-hemodialysis session, the patient’s blood chemistry was stabilized at pH 7.40, 5.1 mmol/L lactate, 19.9 mmol/L HCO3-, and 4.4 m Eq/L K+. This case suggests unsettled questions regarding the clinical criteria and initiation timing for hemodialysis in a high-risk case of MALA. We successfully treated a T2DM patient with a late-onset lactic acidosis using early induction of a single hemodialysis treatment before the recommended timing.
Keywords: Metformin poisoning; Lactic acidosis; Hemodialysis
Introduction
The MET-Associated Lactic Acidosis (MALA) is reported to be a rare complication of MET use. However, this clinical condition is associated with a high mortality rate in T2DM patients, especially those with advanced hepatorenal and pulmonary diseases in conjunction with dehydration, acute infection, cardiac dysfunction, alcohol drinking, and/or old age [1,2]. In view of the clinical severity of MALA, it is crucial to closely monitor patients until any likelihood of the development of lactic acidosis has passed. However, previous reviews have settled on no clear definition regarding the observational period following acute MET overdose [3-5]. Here, we reported a T2DM patient who took a large amount of MET in a suicide attempt. His late-onset MALA was successfully treated by a single early hemodialysis treatment.
Case Presentation
The patient was a 69-y-old non-obese male T2DM patient with an 18-yrs diabetes duration complicated with stage IIIa diabetic nephropathy. Recently, he had been prescribed 1,000 mg MET, 20 mg teneligliptin, and 1 mg glimepiride daily at his family physician’s clinic. However, he had not taken any medication for about 2 months. At around 6:30 am on July 3 (Figure 1), he took 70 tablets (35 g) of MET in attempted suicide while staying at a hotel. He felt severe nausea and chest discomfort and contacted the front desk. Hotel staff immediately requested emergency medical assistance, and he was transported to the emergency outpatient clinic in our hospital in consciousness disturbance (GCS 8 points).
At the emergency room, his blood pressure was 179/109 mmHg with 36.3°C body temperature, and 98% SpO2 on room air. He had spontaneous abdominal pain with persistent nausea and vomiting. Blood laboratory findings are summarized in Table 1. Venous gas analysis showed a pH of 7.46 with blood lactate concentration of 5.7 mmol/L. He showed HbA1c of 9.1% and worsening of renal function with an eGFR of 33 mL/min/1.73 m2 with serum creatinine (s-Cr) of 1.65 mg/dl. However, there were no signs of cardiac failure, infectious diseases, electrolyte imbalance, anemia, or malnutrition.
Table 1: Laboratory data at the time of emergency transport to our hospital.
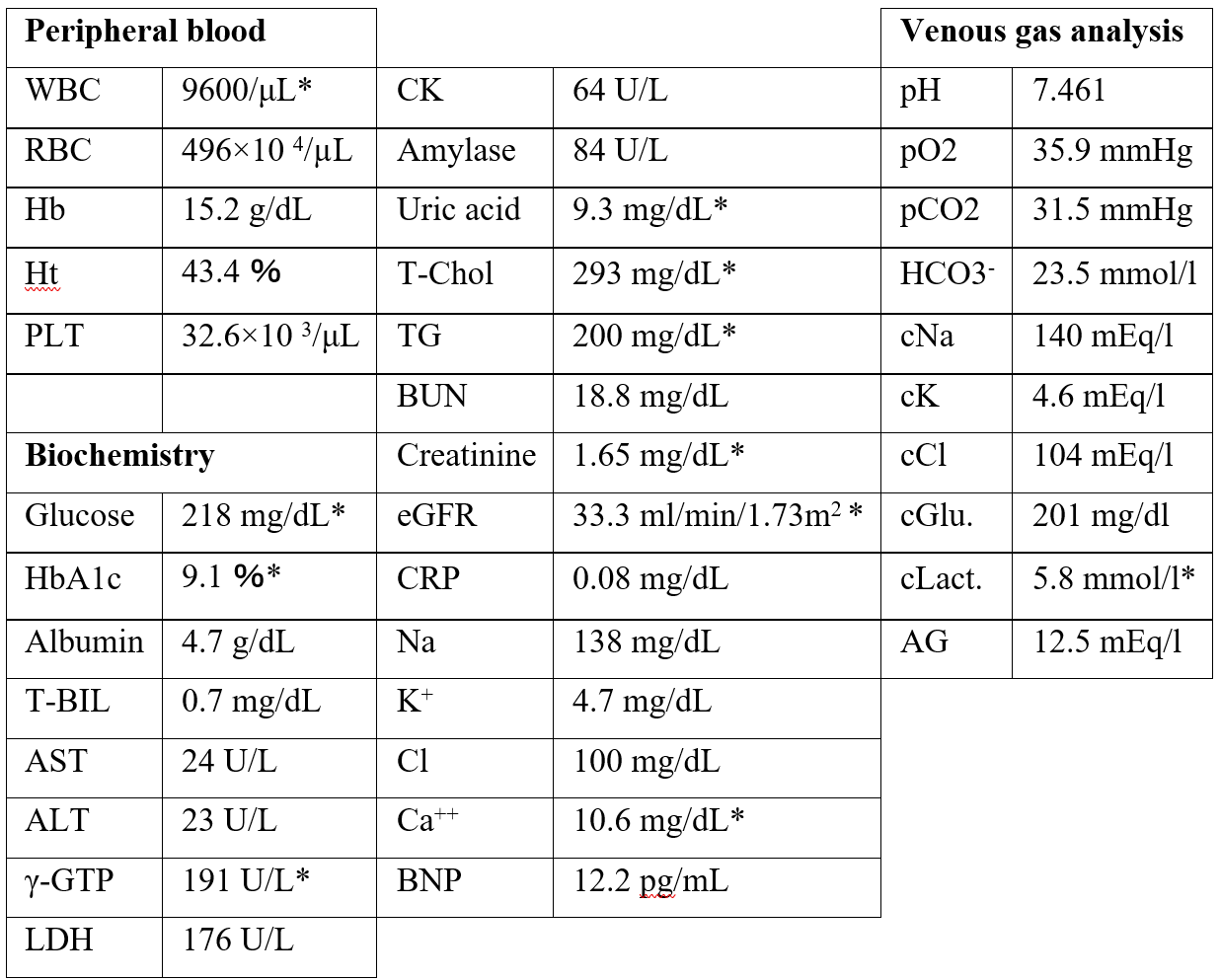
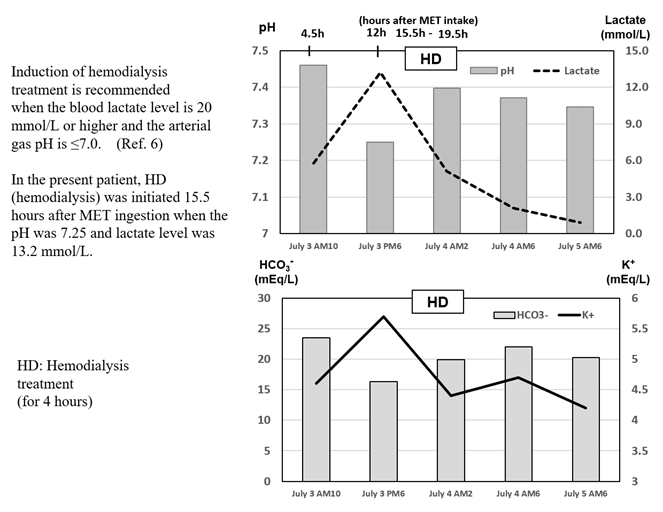
Figure 1: Clinical course of lactic acidosis before and after hemodialysis treatment.
Clinical courses of lactic acidosis before and after hemodialysis treatment
Soon after the initial laboratory test, we started an infusion for fluid management and gastric lavage. The patient was transferred to the Intensive Care Unit at approximately 1:00 p.m. At about 12 hrs. after MET ingestion, we received new lab findings of a pH 7.25 with a markedly increased lactate level (13.1 mmol/L), a low HCO3- level (16.3 mmol/L: a normal range 22–29 mEq/L), an increased anion gap (20.7 mEq/L) along with an elevated K+ level of 5.7 mEq/L, indicating rapid progression to a serious condition. We initiated hemodialysis treatment at 15.5 hrs. after the MET ingestion. Hemodialysis was carried out at the flow rate 500 mL/min using a polysulfone high-performance membrane to treat metabolic acidosis and remove lactate and MET. The 4 hour-hemodialysis treatment was completed successfully, after which his pH had increased to 7.397 and blood lactate level improved to 5.0 mmol/L; the lactate level decreased further to less than 3.0 mmol/L thereafter (Figure 1).
Discussion and Conclusion
MALA is usually suspected by a blood lactate concentration >45 mg/dl (5 mmol/L) and blood gas pH <7.35 in patients who take an overdose of MET. In this case, the patient took a very high dose of MET (35 g at once) in an attempted suicide. His lactic acidosis due to MET overdose was enhanced by impaired renal function and dehydration induced by frequent vomiting.
A basic guideline for application of hemodialysis treatment for MET poisoning was released in 2015, together with a systemic review from the Extracorporeal Treatment in Poisoning Workgroup [6]. The guideline recommends the following: 1) Discontinuation of causative drug, decontamination of gastrointestinal tract, and treatment of primary disease; 2) cardiopulmonary management including infusion of fluids and oxygen administration; and 3) administration of sodium bicarbonate. 4) If the blood lactate level is 180 mg/dl (20 mmol/L) or higher or the arterial gas pH is ≤7.0 after such treatment, hemodialysis treatment should be initiated. The treatment can be terminated if the blood lactate falls to 27 mg/dL (3.0 mmol/L) or below or if arterial gas pH>7.35 is achieved.
Under the careful monitoring of vital signs in the ICU, the patient’s blood lactate level reached 119 mg/dL (13.2 mmol/L) at about 12 hours after MET ingestion with venous blood pH was 7.250. Hemodialysis was initiated immediately, despite blood chemistry not meeting the criteria [6], in consideration of this patient’s stage IIIa diabetic nephropathy combined with the dehydration-related prerenal failure. In this case, a single hemodialysis treatment for 4 hrs. efficiently improved MALA. A similar case report of MALA after attempting suicide in a T2DM patient with schizophrenia has been successfully treated using early introduction of high-flow high-volume intermittent hemodiafiltration [7].
The association of increased lactate levels with renal dysfunction in patients with and without MET intake has been shown in a multicenter cohort study from Denmark [8]. Increased blood lactate levels are observed in relation to the low-eGFR (below 45 ml/min/1.73m2) compared to normal-eGFR group. The time to onset of acute MALA after high doses of MET intake is reported by Theobald et al [9]. In total 40 case between 2001 and 2014, the 40% cases result in lactic acidosis more than 6 hours after ingestion. Although the blood MET concentration usually reaches the maximum 2–3 hours after ingestion at the treatment doses and is maintained for a half-life of 3–4 hours, MET excretion is delayed due to renal impairment, dehydration, and a decreased absorption due to the reduced gastrointestinal transit caused by the metformin itself, which is a cause of delayed onset of lactic acidosis [9]. In fact, we firstly recognized lactic acidosis at about 12 hours after massive MET ingestion.
Another study from Thailand investigating the 30-day mortality rate in 105 patients diagnosed with MALA shows the rate of 36.2%, with a higher proportion of survivors receiving hemodialysis within 6 hours (hazard ratio 0.31; 0.14–0.69; 0.004) [10]. A meta-summary of case reports regarding MET toxicity has been reported using a PRISMA 2009 checklist. Despite severe MALA and the need for multiple organ support, they may have good outcomes, especially when renal replacement therapy is used [11].
In conclusion, a single early hemodialysis therapy initiated at levels not reaching the published standard was effective for treatment of lactic acidosis caused by a high dose of metformin poisoning in a type 2 diabetes patient with advanced renal impairment. Thus, it may be important to re-assess the MALA-treatment guideline to help physicians determine the optimal introductory criteria and initiation timing for extracorporeal treatment in the critical care unit.
Competing interests: All authors have no competing interests to disclose in this case study.
Copyright transfer: The authors have agreed that the copy right for this article is transferred to the Journal of Clinical Images and Medical Case Reports (IJCMCR), if and when the article is accepted for publication.
References
- DeFronzo R, Fleming GA, Chen K, Bicsak TA. Metformin-associated lactic acidosis: current perspectives on causes and risk. Metabolism, 2016; 65: 20-29.
- Lalau J-D, Kajbaf F, Protti A, Christensen MM, DeBroe ME, et al. Metformin-associated lactic acidosis (MALA): Moving towards a new paradigm. Diabetes Obes Metab, 2017; 19: 1502-1512.
- 3. Barrueto F, Meggs WJ, Barchman MJ. Clearance of metformin by hemofiltration in overdose. J Toxicol Clin Toxicol, 2002; 40: 177-180.
- Kopec KT, Kowalski MJ. Case files of the Einstein Medical Center medical toxicology fellowship. J Med Toxicol, 2013; 9: 61-66.
- McNamara K, Isbister GK. Hyperlactataemia and clinical severity of acute metformin overdose. Intern Med J, 2015; 45: 402-408.
- Calello DP, Liu KD, Wiegand TJ, Roberts DM, Lavergne V, et al. Extracorporeal Treatments in Poisoning Workgroup. Extracorporeal treatment for metformin poisoning: Systematic review and recommendations from the extracorporeal treatments in poisoning workgroup. Critical Care Med, 2015; 43: 1716-1730.
- Suzuki K, Okada H, Yoshida S, Okamoto H, Suzuki A, et al. Effect of high-flow high-volume-intermittent-hemodiafiltration on metformin-associated lactic acidosis with circulatory failure: a case report. J Medical Case Reports, 2018; 12: 280, https://doi.org/10.1186/s13256-018-1809-6
- Posma RA, Hulman A, Thomsen RW, Jespersen B, Nijsten MW, et al. Metformin use and early lactate levels in critically ill patients according to chronic and acute renal impairment Critical Care, 2020; 24: 585. http://doi.org/10.1186/s13054-020-03300-y
- Theobald J, Schneider J, Cheema N, DesLauriers C. Time to development of metformin-associated lactic acidosis. Clinical Toxicology, 2019; 58: 758-762.
- Thammavaranucupt K, Phonyangnok B, Parapiboon W, Wongluechai L, Pichitporn W, et al. Metformin-associated lactic acidosis and factors associated with 30-day mortality. PLOS ONE, 2022; 17: e0273678. https://doi.org/10.1371/journal.pone.0273678
- Juneja D, Nasa P, Jain R. Metformin toxicity: A meta-summary of case reports. World Journal of Diabetes. 2022; 13: 654-664.

