Intestinal Non-Hodgkinien Lymphoma Revealed by Abdominal Mass
Amal Hajri1,2, Fadwa Azhari2, Soukaina Khafif2,* Driss Errguibi1,2, Rachid Boufettal1,2, Saad Rifki El Jai1,2 and Farid Chehab1,2
1Surgical Department of Cancerology and Liver Transplantation University Hospital Center, Morocco,
2Faculty of Medicine and Pharmacy, Hassan II University, Morocco
Received Date: 23/08/2023; Published Date: 12/01/2024
*Corresponding author: Soukaina Khafif, Faculty of Medicine and Pharmacy, Hassan II University, Morocco
Abstract
Introduction: Primary lymphomas of the digestive tract are non-Hodgkin's lymphomas (NHL). Their most frequent site is the stomach, followed by the small intestine.
Presentation of Case: A 62-year-old patient presented with an abdominal mass associated with digestive bleeding, transit disorders and altered general condition. Intestinal GIST was suspected in abdominal CT. Resection of two tumor masses and appendectomy were performed. Histological examination and immunohistochemical revealed a diffuse non-Hodgkin's lymphoma with large B cells.
Discussion and Conclusion: The gastrointestinal tract is the most common site of extra-ganglionic DLBCL. Symptoms are variable, it can be revealed by its complications. Endoscopy and CT scan are necessary to orient the diagnosis. The diagnosis is based on histopathological examination . Treatment consists mainly of surgical resection and/or chemoradiotherapy.
Keywords: Lymphoma; Intestinal lymphoma; Diffuse large cell B-cell lymphoma; Abdominal mass
Introduction
Primary lymphomas of the gastrointestinal tract are non-Hodgkin's lymphomas (NHL), and include different anatomical and clinical entities. They are rare and correspond to 1% of gastrointestinal tumors. B lymphomas (90%) are more frequent than T lymphomas (10%).
The most common site of gastrointestinal NHL is the stomach (60-75%), followed by the small intestine and ileocecal region [1].
We report the case of a patient with a diffuse large cell non-Hodgkin's B lymphoma with a double localization; small bowel and appendicular.
Observation
Patient aged 62 years, with no particular pathological history. Presented 7 months before his admission an abdominal mass associated with moelena and constipation, evolving in a context of altered general condition
Clinical examination on admission found a conscious patient stable on the HD and respiratory plan. BMI=16,22 kg/m².PS=0. Apyretic. Discolored conjunctiva. On abdominal examination: Mass straddling the hypogastrium and FIG measuring 24 cm long axis, mobile in relation to the deep and superficial planes, painful to palpation, without inflammatory signs opposite. The rest of the somatic examination was unremarkable.
The abdominal CT scan showed a heterodense median abdominal-pelvic mass with a lumen continuous with that of a bowel loop, poorly limited, with calcification. It measures 124.5x85.5x122.8 mm. Presence of deep adenopathies and probable peritoneal carcinosis, suggesting a lymphomatous or GIST origin.
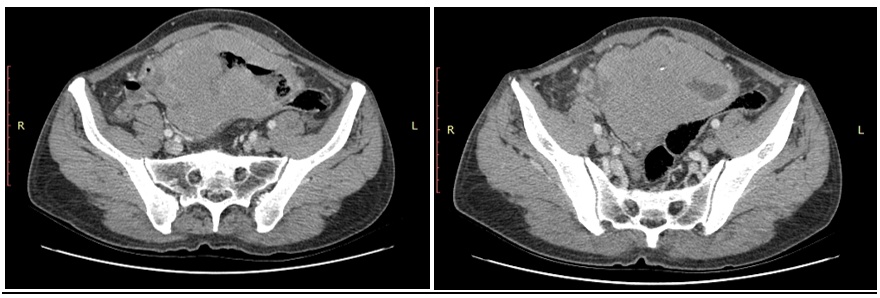
Figure 1: Scannographic appearance of the bowel mass.
Colonoscopy had revealed two millimetric polyps at 3 cm from the AM resected with cold forceps. At pathology, adenomatous polyps with low grade dysplasia were found in the rectum.
The carcinoembryonic antigen (CEA) assay was negative and the blood count showed a microcytic hypochromic anemia with a hemoglobin of 7g/dl. After preoperative preparation, the patient underwent resection of two tumor masses, one of the greaves and the other of the mesentery, with a terminal greaves-terminal anastomosis, a retrograde appendectomy and a drainage of the CDS of Douglas by SS.
The surgical exploration had objectified the presence of 2 solid-cystic tumor masses, one at the mesenteric level measuring 5 cm in diameter, and the other one at the small bowel measuring 20 cm in diameter located at 2m80 from the duodenojejunal angle and at 30 cm from the ileo-coecal junction with several vegetations located at the level of the appendix, of the upper rectum and of the CDS of Douglas, without ascites, nor carcinosis or hepatic nodules. The stomach, the duodenum and the rest of the colonic frame were without particularities (Figure 2, 3).
The immediate postoperative follow-up was simple with resumption of transit on Day 2. Feeding was allowed at D3. The patient was declared discharged at D5 postoperatively.
The anatomopathological examination coupled with the immunohistochemical study of the small bowel, mesenteric and appendix masses had concluded to a diffuse non-Hodgkin's lymphoma with large B cells.

Figure 2: Intraoperative appearance of the mass.
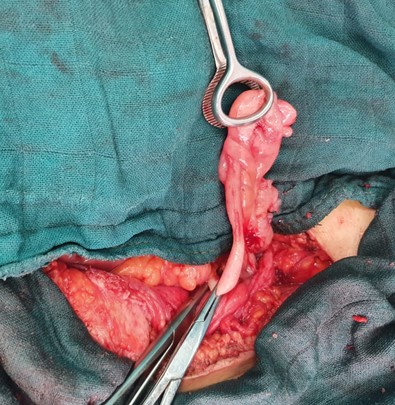
Figure 3: Appendix with vegetations.
Discussion
Non-Hodgkin's lymphomas are rare, their incidence varies according to the country between 0.58 and 1.31/100,000 inhabitants and the average age of their occurrence is between 50 and 70 years [2].
Accounting for 25-30% of non-Hodgkin's lymphomas, diffuse large cell B-cell lymphoma (DLBCL) is the most common lymphoma. The gastrointestinal tract is the most common site of extra-ganglionic DLBCL [3]. Discreetly more frequent in men, it is classically diagnosed after the age of 60, but can occur in children and young adults [4].
Symptoms are variable and may include dyspepsia, epigastralgia, abdominal pain, nausea, vomiting, diarrhea, weight loss, malabsorption, anemia, intussusception or abdominal mass. Severe manifestations such as perforation, obstruction and bleeding are less common [1,5].
In our case, the symptoms were abdominal miasma with moelena and weight loss.
Endoscopy is a fundamental examination for the diagnosis of gNHL. It can reveal a wide variety of different forms: enlarged lymph nodes and lymphoid follicles, which may sometimes appear reactive, polyps or infiltrating and necrotic lesions.
GNHLs may also manifest as mucosal ulceration or hyperplasia [1,5].
On abdominal CT, small bowel B-cell lymphoma may appear as a circumferential mass in the bowel wall, often with mesenteric and regional lymph node extension [6,7].
The tumor may involve a relatively long segment of the small bowel, and may ulcerate and perforate into the adjacent mesentery, resulting in a sterile abscess [6]. Bulky mesentery and/or retroperitoneal adenopathy is demonstrated in small bowel lymphoma in approximately 50% of cases. Atypical small bowel lymphomas present in solid form: polypoid or eccentric masses, making differentiation with small bowel adenocarcinoma mandatory [7].
The diagnosis is based on histopathological examination . Treatment consists mainly of surgical resection and/or chemoradiotherapy [7].
Conclusion
As with other cancers, but perhaps even more so, the management of digestive lymphomas requires a multidisciplinary consultation involving specialists in imaging, anatomopathology of lymphomas, onco-haematologists, radiotherapists and gastroenterologists.
Classically, the three therapies that can be administered to patients with digestive lymphoma are surgery, chemotherapy and radiotherapy.
References
- Magdalena Olszewska-Szopa, Tomasz Wróbel. Gastrointestinal non-Hodgkin lymphomas. Adv Clin Exp Med, 2019; pp. 1119-1124.
- Lepage C, Bouvier AM, Manfredi S, Dancourt V, Faivre J. Incidence and management of primary malignant small bowel cancers: a well-defined French population study. Am J Gastroenterol, 2006; 101: pp. 2826-2832.
- Hee Sang Hwang, Dok Hyun Yoon, Cheolwon Suh, Chan-Sik Park, Jooryung Huh. Intestinal Diffuse Large B-Cell Lymphoma: An Evaluation of Different Staging Systems. The Korean Academy of Medical Sciences, 2014; pp. 53-60.
- Bonnet C, De Prijck B, Lejeune M, Fassotte M-F, Van Den Neste E, Beguin Y. Prise en charge du lymphome B diffus à grandes cellules en 2012. Revue Médicale Suisse, 2012.
- Marnelli A Bautista-Quach, Christopher D Ake, Mingyi Chen, Jun Wang. Gastrointestinal lymphomas: Morphology, immunophenotype and molecular features. Gastrointest Oncol, 2012; 3: pp. 209-225.
- Sangeet Ghai, John Pattison, Sandeep Ghai, Martin E O’Malley, Korosh Khalili, Mark Stephens. RadioGraphics, 2007; 27: 5.
- Hustings N, Feyaerts F. Large B-cell Lymphoma of the Jejunum. Journal of the Belgian Society of Radiology, 2019; 103(1).
- Chuang-bo Yang, Nan Yu, Yong-jun Jian, Yong Yu, Hai-feng Duan, Xi-rong Zhang, et al. Spectral CT Imaging in the Differential Diagnosis of Small Bowel Adenocarcinoma From Primary Small Intestinal Lymphoma. Academic Radiology, 2019; 26: 7.

