Epidermoid Carcinoma of the Pancreatic Head: An Unusual Observation
Hajri Amal, Eddaoudi Yassine, Fatine Amine*, Errguibi Driss, Boufettal Rachid, Rifki Eljay Saad and Chehab Farid
Surgical Department of Cancerology and Liver Transplantation University Hospital Center Casablanca Morocco Faculty of Medicine and Pharmacy, Hassan II University, Casablanca, Morocco
Received Date: 20/08/2023; Published Date: 10/01/2024
*Corresponding author: Fatine Amine, Surgical Department of Cancerology and Liver Transplantation University Hospital Center Casablanca Morocco Faculty of Medicine and Pharmacy, Hassan II University, Casablanca, Morocco
Abstract
Introduction: Epidermoid carcinoma of the pancreas is a rare entity, corresponding to less than 0.5% of pancreatic cancers which are dominated by adenocarcinoma. This is explained by the absence of epidermoid cells in the breast and indeed in the whole digestive system except the esophagus and the anal canal.
Materials and Methods: We report a case of a Patient aged 67 years, diabetic for 1 year on insulin, treated for COVID 19 pathology 6 months before her hospitalization Epidermoid carcinoma of the pancreas In A Patient Admitted in the department of Emergency visceral surgery.
Results: The clinical examination on admission showed a patient with a performance status of 0 and a body mass index of 22 kg/m2 with only a palpable and distended gallbladder on abdominal examination.
The biological work-up revealed a biological cholestasis syndrome with alkaline phosphatases: 1210 IU/l; gamma glutamyl transferase 659 IU/l with a disturbed hepatic work-up, ALT: 228 IU/l; total bilirubin: 266 mg/l; conjugated bilirubin >170 mg/l; free bilirubin: >96 mg/l; on the other hand, ASAT were normal at 48 IU/l. In addition, the tumor marker assay showed a CA 19-9 level >1995 IU/ml.
An abdominal MRI was performed before admission and showed a lesion process centered on the pancreas (Winslow's pancreas) with a discrete T1 hypo signal and a discrete homogeneous T2 hyper signal with little enhancement after injection of contrast medium modifying the contours of the pancreas and measuring 40 x 45 mm. This process is accompanied by a slight infiltration of the adjacent fat with envelopment of the superior mesenteric vein in 1/3 of its circumference without visible endoluminal bud. With presence of invasion of the superior mesenteric artery and superior mesenteric vein and the rétroportal lamina is respected. Moderate dilatation of the Wirsung. Distended gallbladder with dilatation of the intrahepatic bile ducts and the main bile duct to 20 mm. Homogeneous liver without focal lesions, absence of deep adénopathies and absence of ascites classified T2N0Mx
The patient benefited during her hospitalization of an anterograde cholecystectomy with choledoco-duodenal anastomosis side by side L-L and biopsy of a pancreatic tumor with at the exploration: presence of an ascites of weak distended gall bladder with thickened wall, gangrenous with pré-perforative lesions and the main biliary tract dilated to 2 cm. On examination by the anapathomopathologist: Epidermoid carcinoma of the pancreas.
Conclusion: Epidermoid carcinoma represents a rare histological type with a poor prognosis. The mechanisms are so far not represented by theories and the therapeutic conduct is not codified due to the little information we have and this is due to its rarity.
Keywords: Epidermoid carcinoma; Pancreatic location; Curative resection
Introduction
Epidermoid carcinoma of the pancreas is a rare entity, corresponding to less than 0.5% of pancreatic cancers which are dominated by adenocarcinoma [1]. This is explained by the absence of epidermoid cells in the breast and indeed in the whole digestive system except the esophagus and the anal canal.
We will study the observation of a case of Epidermoid carcinoma of the pancreas confirmed by anatomopathological study of a pancreatic biopsy performed intraoperatively of a choledochodenal diversion.
Patient and Observation
Patient aged 67 years, diabetic for 1 year on insulin, treated for COVID 19 pathology 6 months before her hospitalization
Having been hospitalized on March 2021 for epigastric pain evolving for 2 months, radiating to the back associated with a generalized cutaneous-mucosal jaundice, of progressive aggravation, permanent with a clinical cholestasis syndrome made of dark urine and discolored stool with pruritus and without other associated signs in particular no vomiting nor externalized digestive hemorrhages. The whole evolving in a context of weight loss of 25 kg in 5 months.
The clinical examination on admission showed a patient with a performance status of 0 and a body mass index of 22 kg/m2 with only a palpable and distended gallbladder on abdominal examination.
The biological work-up revealed a biological cholestasis syndrome with alkaline phosphatases: 1210 IU/l; gamma glutamyl transferase 659 IU/l with a disturbed hepatic work-up, ALT: 228 IU/l; total bilirubin: 266 mg/l; conjugated bilirubin >170 mg/l; free bilirubin: >96 mg/l; on the other hand, ASAT were normal at 48 IU/l. In addition, the patient had an anemia of 10.9 g/dl; a hyperleukocytosis of 32370 elements/mm3 with a predominance of neutrophils and hypoalbuminemia of 25 g/l. The hydroelectrolytic and renal balance sheets were unremarkable. The tumor marker assay showed a CA 19-9 level >1995 IU/ml.
An abdominal MRI was performed before admission and showed a lesion process centered on the pancreas (Winslow's pancreas) with a discrete T1 hypo signal and a discrete homogeneous T2 hyper signal with little enhancement after injection of contrast medium modifying the contours of the pancreas and measuring 40 x 45 mm. This process is accompanied by a slight infiltration of the adjacent fat with envelopment of the superior mesenteric vein in 1/3 of its circumference without visible endoluminal bud. With presence of invasion of the superior mesenteric artery and superior mesenteric vein and the rétroportal lamina is respected. Moderate dilatation of the Wirsung. Distended gallbladder with dilatation of the intrahepatic bile ducts and the main bile duct to 20 mm. Homogeneous liver without focal lesions, absence of deep adénopathies and absence of ascites classified T2N0Mx surgical exploration showed invasion of the superior mesenteric artery and superior mesenteric vein which made complete resection impossible.
The patient benefited during her hospitalization of an anterograde cholecystectomy with choledoco-duodenal anastomosis latero-lateral and biopsy of a pancreatic tumor with at the exploration: presence of an ascites of weak distended gall bladder with thickened wall, gangrenous with pré-perforative lesions and the main biliary tract dilated to 2 cm.On examination by the anapathomopathologist: Epidermoid carcinoma of the pancreas.
Vascular invasion is not a contraindication for pancreatic tumor resection according to recent studies, but the age of the patient and the general condition do not allow to perform a heavy procedure lateral choledochoduodenal anastomosis, was chosen in this patient who will present a pancreatic process with free duodenum without obstruction preoperative transparietal hepatic biliary drainage is not available in our context.
There is no specific chemotherapy protocol for this case and radiotherapy has a negligible effect on tumor reduction and control.

Figure 1: Axial section of an abdominal MRI showing the lesion process.
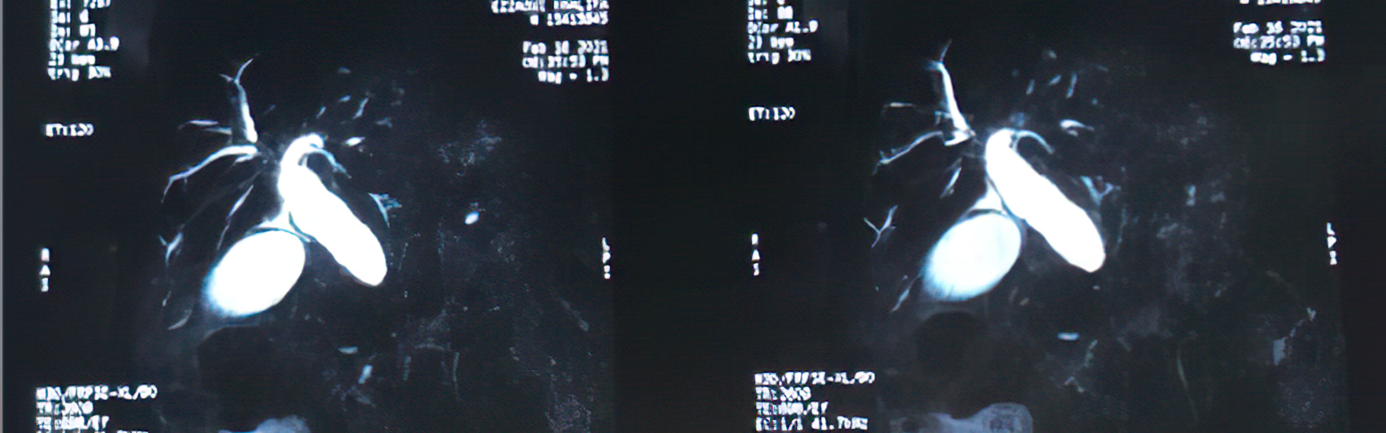
Figure 2: Frontal section of a biliary MRI showing dilatation of the main bile duct with stenosis at its distal part.
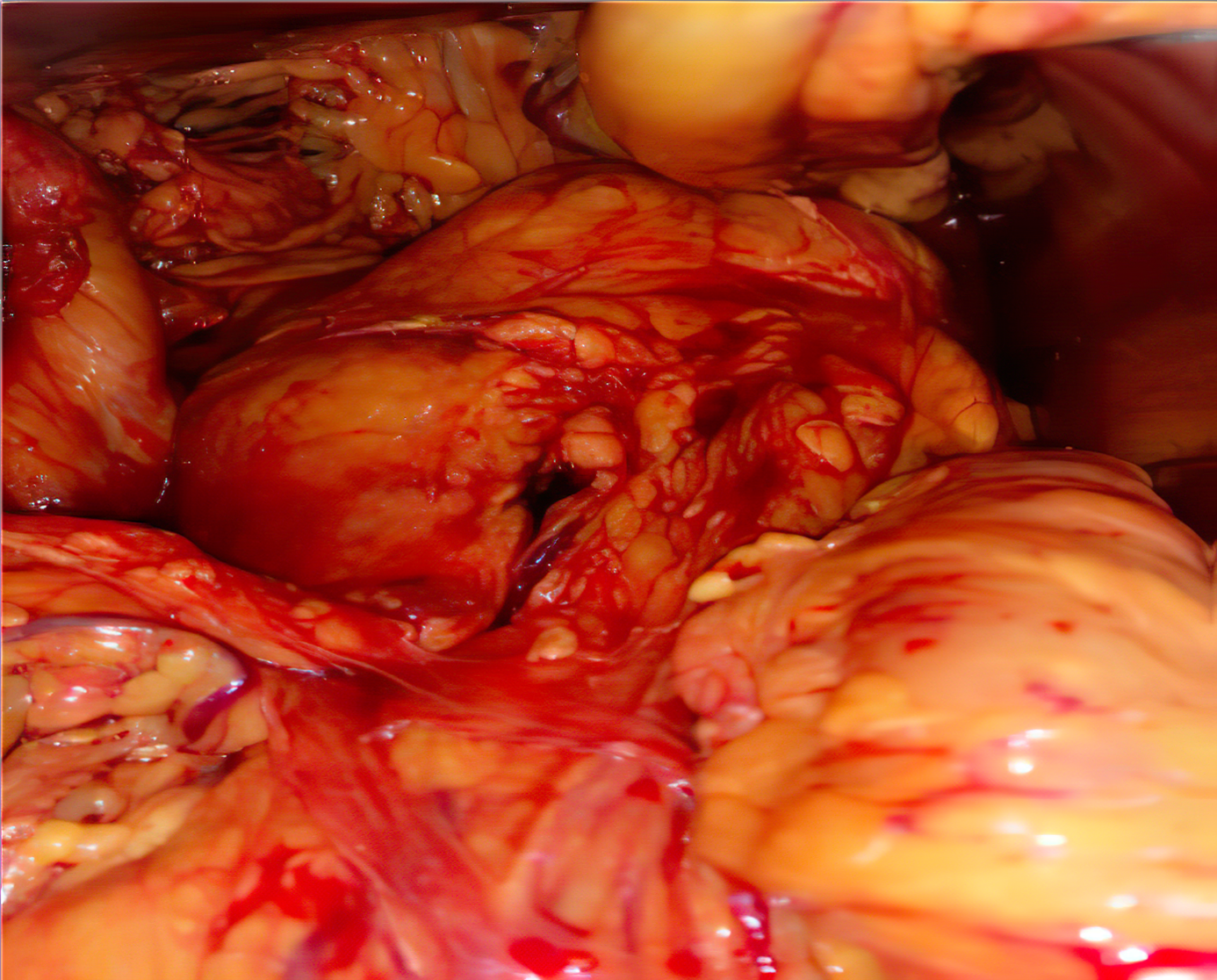
Figure 3: Intraoperative image showing the lesion process of the head of the pancreas.
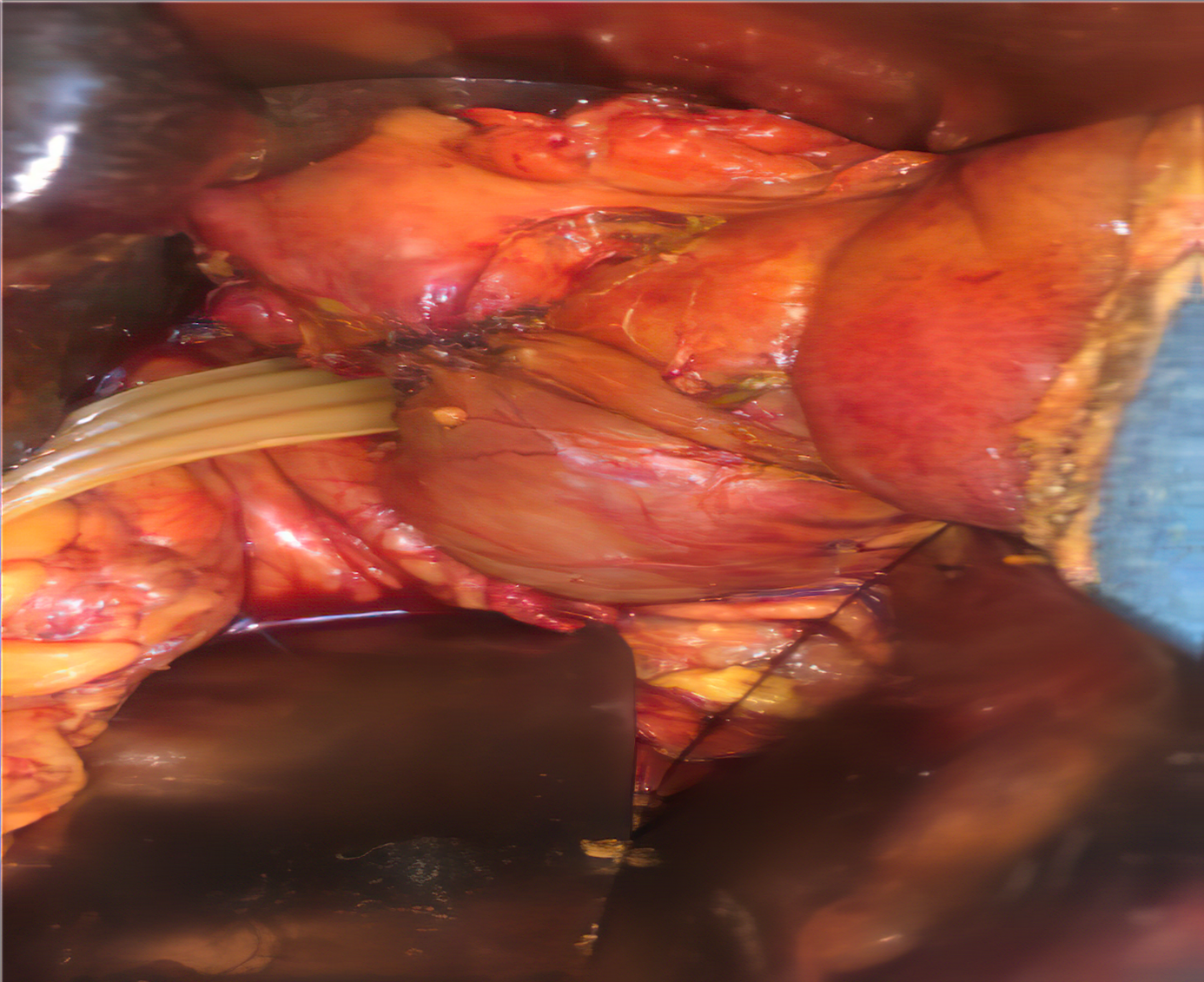
Figure 4: intraoperative image showing the choledoco-duodenal anastomosis side by side latero-laterally, the surgical procedure was performed on a scheduled date with a correct pre-anesthetic assessment; the procedure was performed by an assistant professor in general surgery and two residents in the same specialty.
The operation was performed in the operating room of the visceral emergency department. The patient was satisfied with the intervention and the improvement of his health in the short and long term, The evolution was marked by the disappearance of jaundice, the patient was seen in good general condition after 3 months and 5 months.
Discussion
Epidermoid carcinoma of the pancreas has several similarities with adenocarcinoma but also some particularities, especially when it comes to evolution, since it is more aggressive, prognosis and also therapeutic management.
According to the new WHO classification of 2020, Epidermoid carcinoma is a subtype of ductal adenocarcinoma of the pancreas, the latter being part of the malignant tumors affecting this organ and also including ductal carcinomas, pancreatoblastomas and high-grade pseudo papillary solid tumors [2].
In a 2019 study of 114,166 cases of pancreatic cancer, only 356 cases had Epidermoid carcinoma (0.3%) [1]. Another study conducted in 2020 with a total of 73,074 cases compared adenocarcinoma cases with those with Epidermoid carcinoma of the pancreas, which constituted only 0.2% [3].
Explanatory theories have been proposed to explain the origin of these squamous cells. The diagnosis of a primary Epidermoid carcinoma of the pancreas is made only after eliminating the presence of an Epidermoid carcinoma located elsewhere, in particular the ENT sphere or the anal canal for example, but also eliminating an adenosquamous carcinoma which is characterized by a variable proportion of glandular cells and squamous cells which must constitute more than 30% of the tumor [4].
The normal pancreas is histologically devoid of epidermoid cells. However, benign squamous metaplasia has been noted in 9-64% of pancreases examined postmortem. Squamous metaplasia may be associated with chronic inflammation such as in chronic pancreatitis or pancreatic/biliary stenting. It is also identified in the adjacent ducts of 4% of pancreatic adenocarcinoma surgical specimens [5] and rarely in benign mucinous tumors of the pancreas [6]. It is suggested that these malignant squamous cells of the pancreas pass through various mechanisms, degeneration of a squamous metaplasia of the ductal epithelium, transformation of an adenosquamous tumor from which the adenocarcinomatous component has completely disappeared and differentiation with malignant transformation of the primitive multipotent cells [7,8]. The rarity of Epidermoid carcinoma of the pancreas has led many investigators to question whether it is really a distinct pathological entity, a primary pancreatic adenosquamous underdiagnosed as Epidermoid carcinoma or most likely a metastasis of a primary occult tumor [5,9].
Clinically and comparing with a study of 54 patients with Epidermoid carcinoma of the pancreas, the average age was 61.9 years vs. 67 years. Our patient reported a history of alcohol-smoking, in this study and among the 23 patients with a history of alcohol-smoking, 11 (47.8%) reported alcohol use, seven (30.4%) smoked, five (21.7%) both, while 10 (43.5%) reported no toxic habit. A large majority presented with pain (77.8%) and weight loss (57.4%), while 15 patients (27.8%) presented with jaundice. On diagnostic imaging findings, the average size of the tumor was 6.9 cm vs 4.5 cm, among these 51 cases, more than half (52.9%) the lesion were located in the head of the pancreas, the case also of our patient, three (5.9%) in the body, 11 (21.6%) in the tail and 10 (19.6%) in multiple locations. Biologically, 11 out of 40 (27.5%) had normal blood test values and tumor markers in 16/21 patients (76.2%) were within normal limits, unlike our patient who had a disturbed biological workup, notably a biological cholestasis syndrome, hyperleukocytosis which may be part of the paraneoplastic syndrome and also a very high CA 19.9 which is more or less specific to the pancreas [10]. In another study of 356 cases of Epidermoid carcinoma of the pancreas, the average age was 68.3 years, 55.9% were male, the tumor was located in the head in 54.4% of cases with an average size of 5.7 cm. The tumor was classified as stage III or IV in 71.8% of the cases, while only 28.2% were classified as stage I or II at diagnosis (the case of our patient) [1].
Surgically, the tumor was resectable in only 31.5% of the cases [10], this is explained by the delay in diagnosis but also the proximity of vessels whose invasion contraindicates surgery, the case of our patient who presented an envelopment of the superior mesenteric vein in 1/3 of its circumference without visible endoluminal bud.
The therapeutic course of action is still not codified. In general, the prognosis is poor, several studies have been performed evaluating the efficacy of surgical treatment, chemotherapy, radiotherapy or their combinations. In a study of a total of 155 cases of Epidermoid carcinoma, the median survival of patients who received surgical treatment was much higher than those who did not (21.3 vs. 6.8 months) [11]. Katz et al. reported that the use of radio-chemotherapy could improve prognosis in the palliative, but not adjuvant setting [12]. During this time no chemotherapy protocol has been proven to be effective to date.
The choice of surgical treatment in our case instead of endoscopic treatment given the lack of means and resources in developing countries and the lack of easy access to care, as well as the surgical option is associated with less recurrence of jaundice and postoperative readmissions but the problem that it has more postoperative mortality [13].
Conclusion
Epidermoid carcinoma represents a rare histological type with a poor prognosis. The mechanisms are so far not represented by theories and the therapeutic conduct is not codified due to the little information we have and this is due to its rarity.
Consent Written: Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors' Contributions: This work was carried out in collaboration among all authors. All authors contributed to theconduct of this work. They also declare that they have read and approved the final version ofthe manuscript.
Provenance and Peer Review: Not commissioned, externally peer-reviewed
Conflicts of interest: None
Sources of funding: None
Ethical approval: As per international standard written ethical approval has been collected and preserved by the author(s).
Consent: Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution: This work was carried out in collaboration among all authors. All authors contributed to the conduct of this work. They also declare that they have read and approved the final version of the manuscript.
Research registration (for case reports detailing a new surgical technique or new equipment/technology): None
References
- Zacharia G, Levine J, Winstead NS, Antillon MR, Davis NK. Primary squamous cell carcinoma of the pancreas diagnosed by endoscopic ultrasound-guided fine needle aspiration. J Gastrointestin Liver Dis, 2012; 21: 321-323.
- Qiangpu C, Kun O, Qing-hai G, Fan Z. Squamous cell carcinoma of the pancreas with liver metastasis: a case report. Chinese Medical Journal, 2008; 121: 853-854.
- De Souza AL, Muhammad WS. Squamous cell carcinoma of the Pancreas. JOP, 2014; 15(6): 630-631.
- Beyer KL, Marshall JB, Metzler MH, Poulter JS, Seger RM, Diaz-Arias AA. Squamous cell carcinoma of the pancreas. Report of an unusual case and review of the literature. Dig Dis Sci, 1992; 37: 312-318.
- Nakashima H, Hayakawa T, Hoshino M, Kamiya Y, Ohara H, Yamada T, et al. Squamous cell carcinoma of the pancreas with massive invasion of the retroperitoneum. Intern Med, 1995; 34: 61-64.
- Saitou Y. The investigation of registering carcinoma of the pancreas in Japan. Suizou, 1993; 8: 559-564.
- Lai LH, Romagnuolo J, Adams D, Yang J. Primary squamous cell carcinoma of pancreas diagnosed by EUS-FNA: A case report. World J Gastroenterol, 2009; 15(34): 4343-4345.
- Winter JM, Brody JR, Abrams RA, Lewis NL, Yeo CJ. Cancer of the pancreas. DeVita VT Jr, Lawrence TS, Rosenberg SA. Cancer: Principles and Practice of Oncology. 10th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2015; 49: 657-684.
- Anagnostopoulos GK, Aithal GP, Ragunath K, Kaye P, Rowlands BJ Squamous Cell Carcinoma of the Pancreas: Report of a Case and Review of the Literature. JOP 2006; 7(1):47-50.
- Kodavatiganti R, Campbell F, Hashmi A, Gollins SW. Primary squamous cell carcinoma of the pancreas: a case report and review of the literature. J Med Case Rep, 2012; 6: 295.
- About pancreatic cancer. Macmillan Cancer Support. Macmillan Cancer Support. London, UK: Macmillan Cancer Support, 2013.
- Wexler A, Waltzman RJ, Macdonald, JS. Unusual pancreatic tumors. Raghavan, E., Brecher, M. L., Johnson, D. H., et al. (Eds.). Textbook of Uncommon Cancer. 3rd ed. Chichester, England: John Wiley & Sons; 2006; 6: 32: pp. 367-382.
- Tidjane A, et al. Influence of Blood Bilirubin Level on Prolongation of Postoperative Stay after Performance of Palliative Surgery for Pancreas Head Cancer, Analysis of a Series of 63 Patients. European Journal of Surgical Oncology, 2020; 46(2): e118. https://doi.org/10.1016/j.ejso.2019.11.298

