Digestive Complications Revealing Trechobezoard
Bouali Mounir, Kamal Khadija, Azhari Fadwa*, lbakouri Abdelilah, Elhattabi Khalid, Bensardi Fatimazahra and Fadil Abdelaziz
Surgical Department of Cancerology and Liver Transplantation University Hospital Center Casablanca Morocco, Faculty of Medicine and Pharmacy, Hassan II University, Morocco
Received Date: 20/08/2023; Published Date: 08/01/2024
*Corresponding author: Azhari Fadwa, Surgical Department of Cancerology and Liver Transplantation University Hospital Center Casablanca Morocco, Faculty of Medicine and Pharmacy, Hassan II University, Casablanca, Morocco
Abstract
A bezoar is defined as an intraluminal conglomerate of difficult or non-digestible material that accumulates in the gastrointestinal (GI) tract. They can give rise to complications like gastroduodenal ulceration, haemorrhage, perforation, peritonitis, or obstruction, with a high rate of mortality. The treatment is endoscopic, or surgical removal and usually followed by psychiatric opinion.
Nous rapportons ici deux cas de trichobézoard se présentant l’un comme une perforation gastrique et le deuxiéme dans un tableau d’occlusion grelique.
Keywords: Trichobezoar; Perforation; Women; Psychiatric; Occlusion
Introduction
Trichobezoar is defined as the accumulation in the stomach of non-absorbable human hair [1].
Trichobezoars are often associated with psychiatric illnesses usually occurs in young and adolescent girls [2].
Gastric Trichobezoar (GT) is the most common variety of bezoar found in the stomach.2 On the basis of their contents, bezoars are classified into phytobezoars (composed of nondigestible food materials such as seeds and pits), trichobezoars (composed of hair), lactobezoars (composed of lactose), and pharmacobezoars (composed of medications) [2].
Laparotomy is the gold standard treatment. Surgical treatment should be followed by behavioral and psychiatric treatment.
Case Report 1
A 44-year-old woman, reported to the emergency department with the complaints of pain in middle abdomen, not passing flatus or motion (obstipation) and abdominal distension for the past 7 days. There was generalized tenderness in abdomen with guarding and rigidity. On examination, the patient was pyrexial, tachycardic and with low blood pressure. After initial resuscitation, an abdominal CT scan was performed showing a bulky trichobezoar measuring 17X15X8cm with abnormal contrast enhancement of the gastric wall and parietal pneumatosis.doubt about gastric perforation with extra-luminal air bubble (Figure 1, 2). An emergency exploratory laparotomy was performed and around two liters of pyoperitoneum was removed. On exploration a 3×2 cm perforation was identified in the anterior wall of the prepyloric region of stomach. A large mass could also be felt in the stomach extending from fundus to the pylorus. Visible through the perforation was a large mass of hair (Figure 3, 4). A separate gastroenterotomy was made and the mass was removed. The mass was foul smelling and contained densely wound bunch of hair, threads and bits of plastic. The gastroenterotomy was repaired mainly in a single layer with a suture of the perforation. The postoperative period was uneventful and the patient is under psychiatric treatment. The patient was diagnosed with a scarred area of alopecia.
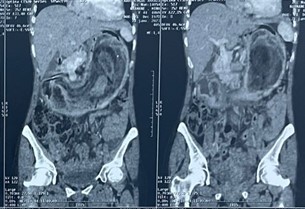
Figure 1: Scannographic aspect of trichobezoar.
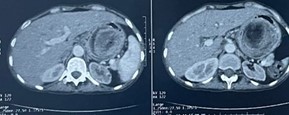
Figure 2: Scannographic aspect of trichobezoar.

Figure 3: Appearance of gastric perforation.

Figure 4: Trichobezoar appearance.
Case Report 2
17-year-old female patient, followed for anaemia under martial treatment, presenting for five days with an occlusive syndrome consisting of cessation of feces and gas associated with diffuse abdominal pain and bilio-food vomiting without HDE. All this evolving in a context of apyrexia and AEG.
On examination: conscious patient, hemodynamically and respiratorily stable BP 110/60 mmHg, FR: 17 cpm, FC: 91 bpm T: 37.5°C with generalized abdominal tenderness accentuated in the hupogastric region. Abdomen without preparation: colonic and giliac hydroaeric levels. Abdominal and pelvic CT (Figure5: a, b): Distension of the small intestines with watery aera, measuring 41 mm at maximum dilatation, upstream of endoluminal material at the level of the last loop, heterodense with concentric bands and air bubbles.This is associated with a voluminous intragastric formation of the same characteristics, responsible for distension of the lumen of the stomach. Appearance in favour of a bezoar. the patient underwent extraction of 2 trichobezoars, one in the gastric region and the other in the last ileal anses, and subhepatic drainage and drainage of the cul de sac of Douglas using 2 salem probes with exploitation: (Figure 6 A, B and 7) Presence of a bezoar in the gall bladder located 30 cm from the last ileal loop responsible for an occlusion with upstream dilatation to 4 cm without signs of distress and another occupying the entire stomach. The postoperative period was uneventful and the patient is under psychiatric treatment.
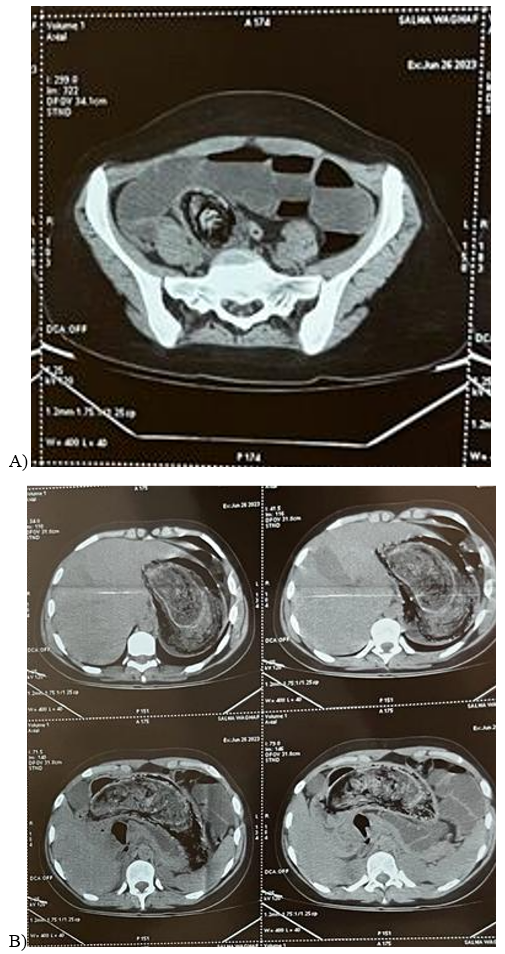
Figure 5A, 5B: Scannographic aspect of trichobezoar.

Figure 6A, 6B: Bezoard grelique.

Figure 7: Trichobezoar appearance.
Discussion
Bezoar" comes from the Persian "Panzehr", or the Arabic "Badzehr", meaning antidote or anti-poison [3].
Trichobezoar occurs in 80% of cases under the age of 30, with a peak between the ages of 10 and 19 [5].
Females predominate (90% of cases). Trichobezoar is often seen in emotionally disturbed or depressed patients and prisoners [1]. Trichobezoar may remain asymptomatic for a long time or manifest as vague epigastric discomfort (80%), abdominal pain (70%), nausea or vomiting (65%), asthenia with weight loss (38%) or transit disorders (33%) such as diarrhoea or constipation [6]. In our case, it was revealed by digestive perforation.
The most common complications reported over the years, include gastric mucosal erosion, ulceration, and perforation of the stomach or the small intestine, gastric outlet obstruction, intussusception, obstructive jaundice, protein-losing enteropathy, pancreatitis and death [7].
Diagnosis is based on oesophageal-gastro-duodenal fibroscopy, which remains the gold standard. It has a dual purpose, firstly diagnostic, allowing visualisation of a process composed of tangled hairs, pathognomonic of trichobezoar, and secondly therapeutic, allowing endoscopic extraction of the latter [8]. Ultrasound is diagnostic in 25% of cases, showing a superficial, hyperechoic, curvilinear band with a clear posterior shadow cone [9].
if unsuccessful, endoscopic extraction [10]. The treatment of choice remains conventional or laparoscopic surgery [14], which allows exploration of the entire digestive tract, extraction of the gastric trichobezoar through a gastrotomy, and extraction of any extension (tail) or fragments of the trichobezoar blocked at a distance from the stomach through one or more enterotomies and psychiatric management of patients is also often required [11,12].
Conclusion
The Trichobezoar remains a pathological curiosity, due to its nature and its rarity. Its simple diagnosis and treatment should not, however, obscure the possible psychiatric care of patients, which remains difficult to apply and acceptable in our context.
References
- Harrabi F, Ammar H, Ben Latifa M, Gupta R, Ben Ali A. Gastric Trichobezoar Causing Gastrointestinal Bleeding: A Case Report. Cureus. 2022.
- Ahmad Z, Sharma A, Ahmed M, Vatti V. Trichobezoar Causing Gastric Perforation: A Case Report. 41(1).
- Koh AZY, Nyanti LE, Lim S, Luk TL, Tang ASO, Leong TS, et al. Trichobezoar masquerading as massive splenomegaly: Rapunzel’s syndrome revisited. Radiol Case Rep, 2022; 17(6): 2243‑2246.
- Giant gastric trichobezoar in a young female - PubMed, 2023.
- Szor DJ, Dias AR. Gastric trichobezoar. Clin Case Rep, 2017; 5(11): 1907.
- Haggui B, Hidouri S, Ksia A, Oumaya M, Mosbahi S, Messaoud M, et al. Management of Trichobezoar: About 6 Cases. Afr J Paediatr Surg AJPS, 2022; 19(2): 102‑104.
- Edwards M, Kaz A, Wander PL. Trichobezoar Without Trichotillomania-a Case Report. J Gen Intern Med. mars, 2022; 37(4): 962‑965.
- Tidswell TH. -Chronic Lymphatic Letkaemia ’in Mat of 84.
- De Melio J, Debrouwere T, Herman M. Trichobezoar. J Belg Soc Radiol. 105(1): 31.
- Ohnesorge S, Skari H, Zochowski K, Pekrun EM, Schistad O, Næss PA. Trichobezoar. Tidsskr Den Nor Laegeforening Tidsskr Prakt Med Ny Raekke, 2020; 140(17).
- Hassani K, El Bouhaddouti H, Benamar Y, Mazaz K, Taleb K. Trichobezoar gastrique - à propos de deux cas. Pan Afr Med J, 2013; 6(1).
- Gastric trichobezoar with duodenal and jejunal extension | Elsevier Enhanced Reader, 2023.

