A Ciruclar Rash in A Moroccan Patient: Think of Pityriasis Rotunda
Kenza Tahri Joutei Hassani*, Meryem Soughi, Zineb Fajri, Hiba Essoulaimani, Hanane Baybay, Sara Elloudi, Zakia Douhi and Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II, Morocco
Received Date: 07/08/2023; Published Date: 20/12/2023
*Corresponding author: Dr. Tahri Joutei Hassani Kenza, Department of Dermatology, University Hospital Hassan II, Fes, Morocco
Abstract
Pityriasis rotunda is an uncommon cutaneous disorder that exhibits a distinct geographic distribution, predominantly reported in Japan, Italy, and South Africa. The condition is characterized by the manifestation of scaly, circular, well-defined, hypo- or hyperpigmented plaque, with no inflammatory changes, on the trunk and extremities. Although the etiology of the disorder remains largely idiopathic, it has been associated with certain systemic diseases or malignancies. We report the case of an otherwise healthy 30-year-old male of Moroccan origin diagnosed with pityriasis rotunda presenting a colonic polyposis.
Keywords: Pityriasis rotunda; Ichthyosiform scaling; Colonic polyposis
Introduction
Pityriasis rotunda is a rare dermatological condition distinguished by the presence of circular or oval-shaped, distinctly demarcated, and pigmented patches that lack any associated inflammatory changes [1]. This scaly disease, also referred to as pityriasis circinata and acquired pseudoichthyosis, was originally reported by Toyama in Japan in 1906 [1], and is characterized by hyper- or hypopigmented circular patches that are marked by dry, ichthyosiform scaling [2]. Pityriasis rotunda most commonly manifests on the buttocks, thighs, abdomen, trunk, and upper and lower extremities. Grimalt suggested two distinct types of the disease: Type I predominantly affects individuals of black and Asian descent and is frequently linked to internal diseases or malignancies but lacks any family history. On the other hand, Type II is more prevalent among Caucasians and patients under 40 years of age, and tends to occur in multiple members of the same family [3]. We report the case of a 30-year-old Moroccan patient diagnosed with pityriasis rotunda type I that revealed the presence of a colonic polyposis.
Observation
This is a 30-year-old patient with no significant medical history except a severe weight loss (35 kg weight) and no similar family history, who has been experiencing asymptomatic pigmented lesions on the trunk for the past 10 years. On dermatological examination, multiple finely scaly, well-defined, perfectly rounded pigmented plaques were observed, sometimes merging into polycyclic patches, measuring 3 to 10 cm in diameter. These lesions were located on the back and the roots of the limbs (Figure 1). Dermoscopy revealed the presence of a pigmented linear network (Figure 2). Histological analysis showed perivascular lymphocytic infiltrates with orthokeratosis and pigmentation. Periodic Acid-Schiff (PAS) staining was negative. These findings were indicative of Pityriasis rotunda. Routine investigations including complete blood count, urine analysis, liver function tests, renal function and thyroid panel tests were within normal limits. Chest X-ray, abdomino-pelvic ultrasonography and TAP -CT were normal. Considering the significant and unexplained weight loss, we proceeded to conduct a faecal calprotectin test, which returned elevated results at 700. To further investigate the matter, we sought a gastroenterologist's opinion. Subsequently, the patient underwent an FOGD, which revealed chronic gastritis with fibrous remodelling but no metaplasia and rarefaction of parietal cells, raising suspicions of an autoimmune etiology. To explore this possibility, an autoimmune work-up was conducted, yielding normal results. Additionally, the patient underwent colonoscopy, which showed the presence of a tubular adenoma with low-grade and high-grade dysplasia.

Figure 1: Multiple, well-defined, perfectly rounded, scaly pigmented plaques, confluent in places to form polycyclic plaques.
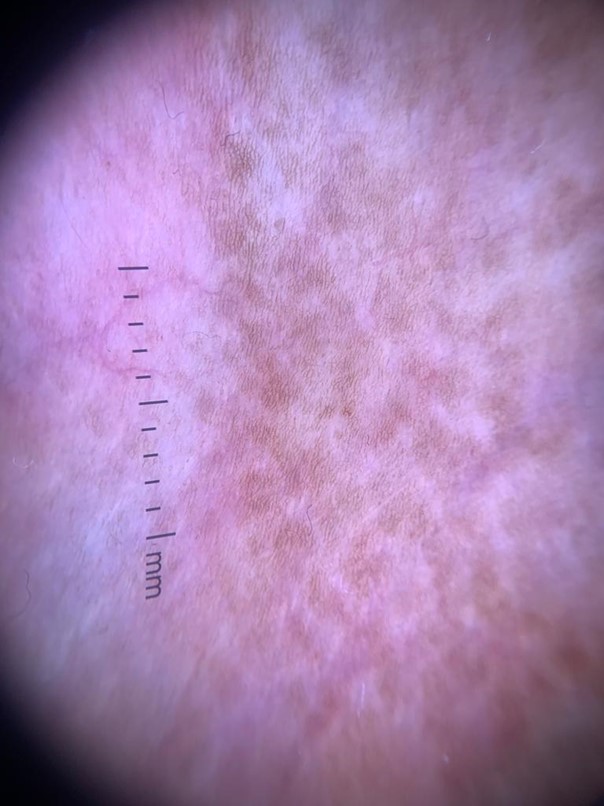
Figure 2: Dermoscopy: a patchy linear pigmented network.
Discussion
Pityriasis rotunda, previously known as pityriasis circinata and historically referred to as tinea circinata, manifests as large circular scaly thin plaques, measuring between 10 to 30 cm. These plaques can appear hypo- or hyperpigmented and are typically found on the trunk and extremities [4]. The number of lesions has been observed to increase during the winter and decrease during the summer. The exact pathophysiology of pityriasis rotunda remains unknown. However, it is believed to involve reduced expression of filaggrin-2, particularly in the granular layer, resembling a type of acquired ichthyosis. This decreased filaggrin expression leads to increased skin thickening, resulting in the formation of scaly circles [5]. Although the term "tinea circinata" suggests a fungal origin, dermatophytes and other fungal species are not found in pityriasis rotunda lesions. The differential diagnosis for pityriasis rotunda includes tinea corporis, tinea versicolor, leprosy, and erythrasma. Potassium hydroxide testing of the scale yields negative results in pityriasis rotunda. Although the diagnosis of pityriasis rotunda is mainly clinical, histopathological examination often reveals hyperkeratosis, hypogranulosis, and sometimes a pigmented basal layer with a mild perivascular lymphocytic infiltrate [3]. These histological features closely resemble those observed in ichthyosis vulgaris.
There are two types of pityriasis rotundas; however, some cases may not fit neatly into these categories [6]. Class 1 pityriasis rotunda presents as hyperpigmented lesions in elderly Asian or African patients, often associated with an underlying infection or malignancy, particularly gastrointestinal malignancies like hepatocellular carcinoma. Usually, fewer than 30 lesions are observed, and about 30% of cases are linked to malignancy [7]. There have been a few reported cases associated with various other cancers, including multiple myeloma [8], as well as systemic illnesses like malnutrition [9], anorexia nervosa [10], and mycobacterial diseases. Our case describes a type 1 pityriasis rotunda associated with colonic polyposis. On the other hand, class 2 pityriasis rotunda manifests as hypopigmented lesions in young adult Northern Europeans, showing a strong hereditary component and lying within the spectrum of congenital ichthyoses. In this type, more than 30 lesions are commonly seen, but it is not associated with any underlying disease. Treatment approaches for pityriasis rotunda can be conservative since the lesions are typically asymptomatic and may resolve spontaneously. Some reported effective treatments include tretinoin cream, anti-fungal agents, lactic acid, and salicylic acids [11]. For extensive disease in type 2 pityriasis rotunda, systemic vitamin A can be used. For cases of type 1 pityriasis rotunda, it is crucial to treat any underlying disease, as it may lead to clinical improvement of the rash.
Conclusion
Pityriasis rotunda is an extremely uncommon condition, and our patient represents only the second reported case in Morocco. The underlying mechanisms of this disease remain unidentified, and its clinical features are highly characteristic. However, the dermoscopic description of the disease remains vague due to limited dermoscopic publications. Moreover, it is frequently associated with other conditions that warrant thorough investigation, particularly in young individuals.
Consent: The examination of the patient was conducted according to the Declaration of Helsinki principles.
Conflicts of interest: The authors do not declare any conflict of interest.
References
- Oji V, Metze D, Traupe H. Inherited disorders of cornification. In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D, eds. Rook’s Textbook of Dermatology, 9th edn. Oxford: Wiley Blackwell, 2016; 2: 65.41–65.42.
- Hasson I, Shah P. Pityriasis rotunda. Indian J Dermatol Venereol Leprol, 2003; 69: 50–51.
- Grimalt R, Gelmetti C, Brusasco A, Tadini G, Caputo R. Pityriasis rotunda: report of a familial occurrence and review of the literature. J Am Acad Dermatol, 1994; 31(5 Pt 2): 866-871.
- SHIH, Allen F. et SHEN, Lisa Y. A Circular Rash in a Teenager. The Journal of Pediatrics, 2022; 242: p. 253-254.
- Makino T, Mizawa M, Seki Y, Hayashi M, Shimizu T. Decreased filaggrin- 2 expression in the epidermis in a case of pityriasis rotunda. J Dermatol Sci, 2016; 84: e138.
- Lefkowitz EG, Natow AJ. Pityriasis rotunda: a case report of familial disease in an American-born black patient. Case Rep Dermatol, 2016; 8: 71-74.
- Zur RL, Shapero J, Shapero H. Pityriasis rotunda diagnosed in Canada: case presentation and review of the literature. J Cutan Med Surg, 2013; 17: 426-428.
- Van Heerden T, Webb MJ, Barrett CL. Pityriasis rotunda as an incidental paraneoplastic finding in two patients with multiple myeloma. Clin Exp Dermatol, 2014; 39: 734-737.
- Swift P, Saxe N. Pityriasis rotunda in South Africa-a skin disease caused by undernutrition. Clin Exp Dermatol, 1985; 10: 407-412.
- Jung SY. A case of pityriasis rotunda with anorexia nervosa. Hong Kong J Dermatology Venereol, 2018; 26: 75-79.
- Al-Refu K, Al-Tarawneh A, Odeibat H. Pityriasis rotunda. A clinical study in Jordan: experience of 10 years. Int J Dermatol, 2018; 57: 759-762.

