A Peculiar Reticular Rash of The Extremities: Think of Reticular Erythematous Mucinosis
Kenza Tahri Joutei Hassani*, Zakia Douhi, Bouayad K, Hanane Baybay, Sara Elloudi, Meryem Soughi and Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II, Morocco
Received Date: 05/08/2023; Published Date: 19/12/2023
*Corresponding author: Dr. Tahri Joutei Hassani Kenza, Department of Dermatology, University Hospital Hassan II, Fes, Morocco
Abstract
Reticular erythematous mucinosis is a type of primary cutaneous mucinosis characterized by the presence of erythematous macules, papules, or plaques that merge together to form a reticular pattern. This condition typically affects the midline of the chest or back in middle-aged women, earning it the name "midline mucinosis." While there have been reports of the disease manifesting in atypical locations, these cases have always been accompanied by involvement of the midline. We report a case of reticular erythematous mucinosis that exclusively affected the extremities and we describe its dermoscopic and histological aspects.
Keywords: Mucinosis; Reticular erythematous mucinosis; Cutaneous mucinoses
Introduction
Reticular Erythematous Mucinosis (REM) is a rare condition classified as one of the midline primary cutaneous mucinoses. It is characterized by the presence of net-like confluent macules and patches or poorly-defined plaques, typically distributed on the anterior chest and upper back [1–3]. These lesions are generally asymptomatic and tend to persist over time. REM has been more commonly reported in younger to middle-aged women, with its occurrence in children being relatively rare [1–3]. While most reported cases are sporadic, there have been a few isolated reports of familial occurrences [4,5]. The precise etiology of REM remains unclear. Factors such as heat exposure, radiotherapy, hormonal status (menstruation, pregnancy, oral contraceptives), viral infections, and immunologic dysfunction have been suggested as potential promoters or exacerbators of REM [6,7]. However, the pathogenesis of REM remains poorly understood [6,7]. The relationship between REM and inflammatory autoimmune disorders is not fully elucidated. Nevertheless, REM has been more consistently associated with autoimmune diseases such as Hashimoto thyroiditis, SLE/lupus tumidus, diabetes, and idiopathic thrombocytopenic purpura [6,7]. We report the case of a 30-year-old woman presenting a REM exclusively on the extremities and we describe its clinical, dermoscopic and histological aspects.
Case Report
We report the case of an otherwise healthy 30-year-old woman who presented 5 months prior to consultation a non-pruritic erythematous rash of the upper and lower limbs without involvement of the trunk or face, diagnosed as Pityriasis rosea of and put under topical corticosteroids during 1 month without improvement. The patient reported exacerbation of the rash with heat, a photosensitivity without any other systemic signs. She didn’t take any form of hormonal contraception. Clinical examination found erythematous macular plaques slightly infiltrated sometimes with reticulated arrangement of the upper and lower limbs (Figure 1). There were no lesions on the face, trunk or mucosis. Dermoscopy showed dotted vessels on a slightly erythematous background with perifollicular distribution in some areas (Figure2). Histology found a perivascular, and occasionally perifollicular, mononuclear cell infiltrate without epidermal changes. Alcian blue-PAS staining showed a minimal amount of mucin deposition among dermal collagen bundles confirming the diagnosis of REM (Figures 3a, 3b). Blood tests including complete blood count,liver, renal, and thyroid panel were within normal ranges. Tests for antinuclear antibodies ANA were also negative. The preferred treatment for REM is antimalarial drugs like hydroxychloroquine [8]. However, due to the patient's concerns regarding systemic treatment, we opted to avoid such an approach. As of now, there is no established alternative therapy for REM. Hence, we decided to pursue a topical treatment using bethametasone ointment 0.5%, which resulted in complete remission within 3 months.

Figure 1: Erythematous plaques with a reticular pattern of the thigh.
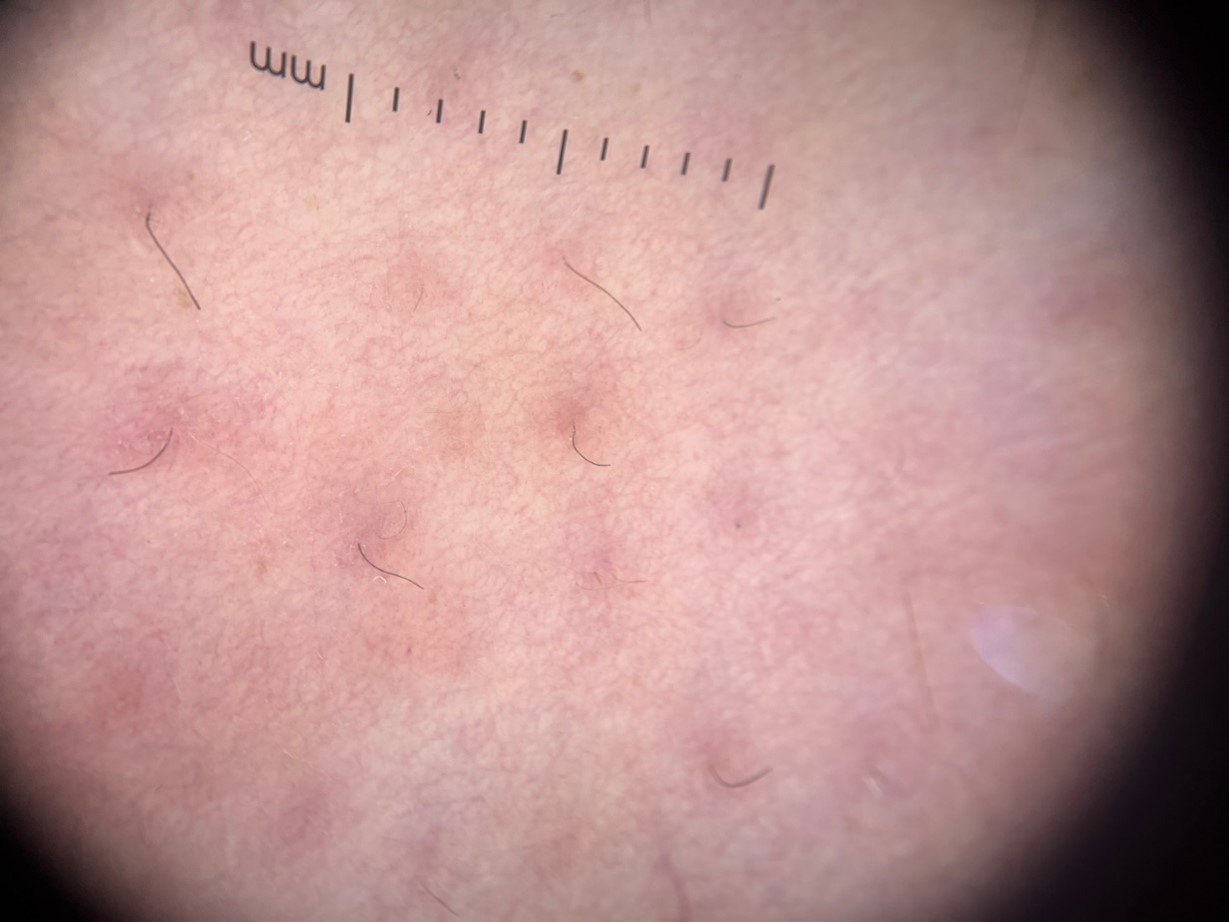
Figure 2: Dermoscopy showing dotted vessels on a slightly erythematous background with perifollicular distribution.
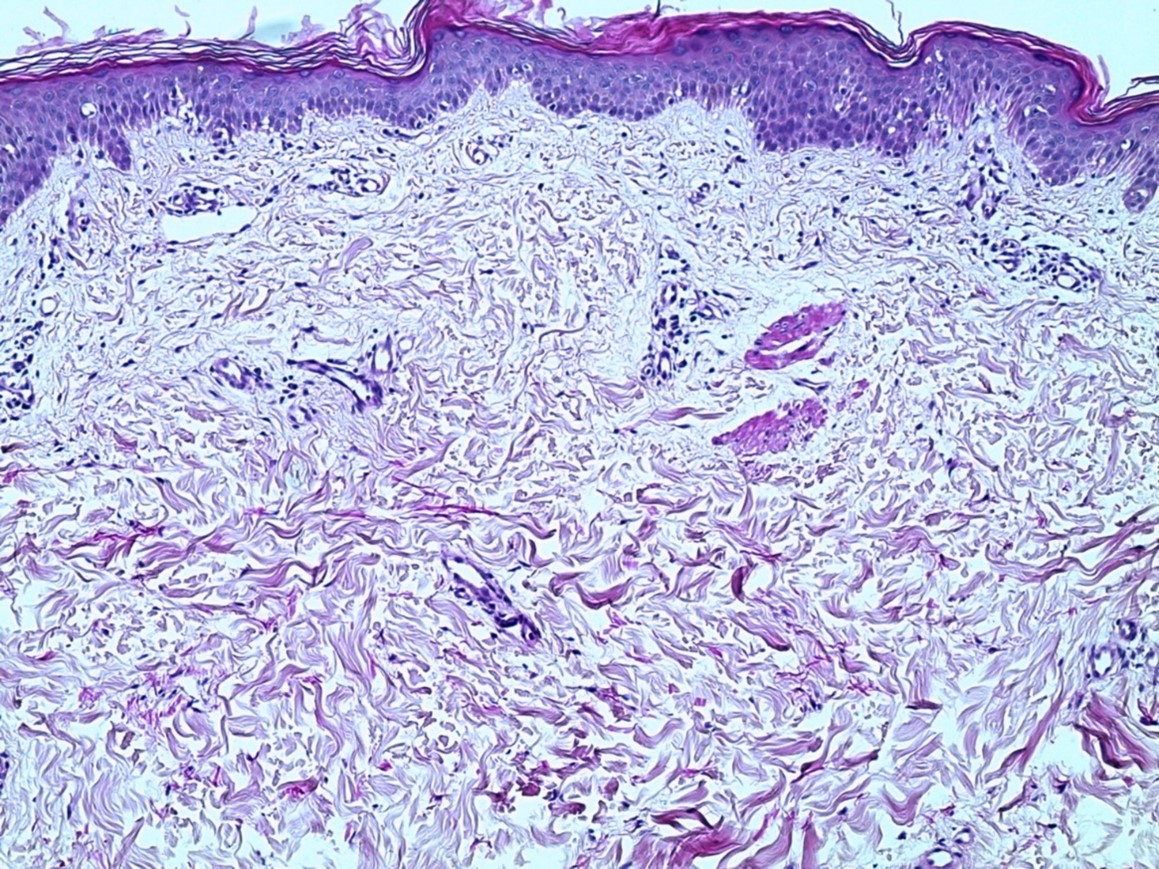

Figure 3: a- Hematoxylin and eosin stain demonstrates very aerated collagen bundles of the dermis separated by optically empty HES deposits at the level of the dermis + discrete perivascular lymphocytic infiltrates, no fibrosis or fibroblast hyperplasia(x50). b- Alcian Blue stain Moderate deposits of alcianophilic mucin at the level of the dermis, especially superficial and middle(x100).
Discussion
REM, also known as midline mucinosis, primarily affects sun-exposed areas of the skin, particularly the midline of the chest or upper midback in young and middle-aged females. The typical clinical presentation involves pink to red macules, papules, or plaques that merge to form a reticulated pattern. Usually, these lesions are asymptomatic or cause only mild itching [9].
The exact etiopathogenesis of REM remains uncertain; however, several factors have been hypothesized to contribute to the onset or exacerbation of the disease, including viral infections, immunological disturbances, or exposure to sunlight [7]. Some associated conditions, such as breast, lung, and colon carcinoma, as well as hematological or hormonal dysfunction like thyroid diseases, have been reported in patients with REM [11].
Aside from the typical areas, REM has been reported in the literature to appear in less common sites such as the face, legs, arms, abdomen, or surgical scars [7,9,10]. However, such occurrences were always accompanied by simultaneous lesions on the midline.
Conclusion
Reticular erythematous mucinosis is a rare dermatological condition characterized by distinctive clinical and histopathological features. While its exact etiology and pathogenesis remain elusive, advancements in diagnostic techniques and therapeutic options have contributed to better understanding and management of REM. Increased awareness among healthcare professionals is crucial for early recognition, accurate diagnosis, and appropriate treatment of this uncommon condition.
Consent: The examination of the patient was conducted according to the Declaration of Helsinki principles.
Conflicts of interest: The authors do not declare any conflict of interest
References
- Kucukunal A, Altunay I, Demirci GT, Sarikaya S, Sakiz D. Reticular erythematous mucinosis on the midline of the back. Cutis, 2014; 93(6): 294–296.
- Cohen PR, Rabinowitz AD, Ruszkowski AM, DeLeo VA. Reticular Erythematous Mucinosis Syndrome: review of the world literature and report of the syndrome in a prepubertal child. Ped Dermatol, 1990; 7(1): 1–10.
- Sidwell RU, Francis N, Bunker CB. Hormonal influence on reticular erythematous mucinosis. Br J Dermatol, 2001; 144(3): 633–634.
- Caputo R, Marzano AV, Tourlaki A, Marchini M. Reticular Erythematous Mucinosis occurring in a brother and sister. Dermatol, 2006; 212(4): 385–387.
- Fühler M, Ottmann K, Tronnier M. Reticular erythematous mucinosis (REM syndrome) in twins. J Dtsch Dematol Ges, 2009; 7(11): 968–970.
- Wriston CC, Rubin AI, Martin LK, Kossard S, Murrell DF. Plaque-like cutaneous mucinosis: case report and literature review. Am J Dermatopathol, 2012; 34(4): e50–54.
- Thareja S, Paghdal K, Lien MH, Fenske NA. Reticular erythematous mucinosis: a review. Int J Dermatol, 2012; 51(8): 903–909.
- Dick J, Kroehl V, Enk AH, Toberer F. Reticular erythematous mucinosis in a young woman: complete remission following oral hydroxychloroquine. Australas J Dermatol, 2019; 60(4): e343–345.
- Rongioletti F, Merlo V, Riva S, Cozzani E, Cinotti E, Ghigliotti G, et al. Reticular erythematous mucinosis: a review of patients’ characteristics, associated conditions, therapy and outcome in 25 cases. Br J Dermatol, 2013; 169(6): 1207–1211.
- Atci T, Polat Ekinci A, Buyukbabani N, Baykal C. Reticular erythematous mucinosis on a mastectomy scar and relapse after mammary reconstruction. J Eur Acad Dermatol Venereol, 2017; 31(1): e13–15.
- Leon-Mateos A, Ginarte M, León L, Toribio J. Reticular Erythematous Mucinosis (REM) with telangiectasias associated with essential thrombocytosis and lung carcinoma. Eur J Dermatol, 2005; 15(3): 179–181.

