Sister Mary Joseph Nodule Hiding an Unknown Metastatic Serous Ovarian Cancer: A Lesson to Learn!
Hajar El Agouri1,*, Abdelhamid Benlghazi2, Mohamed Allaoui1, Mohamed Oukabli1 and Hafsa Chahdi1
1Department of Pathology, Mohammed V Military University Hospital, Faculty of Medicine and Pharmacy, Mohammed V University, 10100 Rabat, Morocco
2Department of Obstetrics and Gynecology, Mohammed V Military University Hospital, Faculty of Medicine and Pharmacy, Mohammed V University, 10100 Rabat, Morocco
Received Date: 17/07/2023; Published Date: 08/12/2023
*Corresponding author: El Agouri Hajar, Department of Pathology, Mohammed V Military University Hospital, Faculty of Medicine and Pharmacy, Mohammed V University, 10100 Rabat, Morocco
Abstract
Sister Mary Joseph Nodule (SMJN) is a metastatic umbilical lesion that occurs as a result of a primary malignancy affecting various organs, with the stomach and colon being the most common in men, and the ovary in women.
In this article, we present a case of SMJN in an 82-year-old female patient. An urgent diagnostic workup was conducted, which included an MRI of the abdominal cavity and pelvis. The MRI revealed a large tumor located behind the uterus, along with peritoneal carcinomatosis and the presence of a nodule in the umbilical region. Following a biopsy, the morphological findings and immunohistochemical profile strongly indicated serous carcinoma of ovarian origin.
This particular case highlights the challenges encountered in diagnosing SMJN based on physical examination findings, and emphasizes the importance of employing immunohistochemistry to differentiate the primary site of cancer. Gynecological malignancies should always be considered as part of the initial differential diagnosis when dealing with SMJN.
Keywords: Sister Mary Joseph Nodule; Gynaecological malignancy; Ovarian serous carcinoma; Cutaneous metastasis
Introduction
Sister Mary Joseph’s Nodule (SMJN) is a rare physical sign of metastatic abdominopelvic malignancy, characterized by a malignant umbilical nodule. Umbilical skin metastases are relatively uncommon in clinical practice, with an incidence ranging from 1 to 3%, and they are typically associated with gastrointestinal or genitourinary cancers [1]. In approximately 30% of cases, the primary source of the neoplasm remains unidentified [2].
The presence of SMJN can occur at the time of diagnosis or during disease recurrence, and it is strongly indicative of a very poor prognosis [3]. These nodules are often a late manifestation of extensive abdominopelvic malignancy.
In this report, we present an original case of a patient who was diagnosed with metastatic serous ovarian cancer and subsequently developed periumbilical nodules during the course of the disease.
Case Report
We report a case of 82-year-old female patient, G3P3, menopaused, with a history of atrial fibrillation treated with anti-vitamin K.
There was no notion of long-term oral contraception, hormone replacement therapy for menopause, or history of vaginal bleeding.
The history of the disease goes back to 6 months by the installation of a great abundance of ascites associated with lower extremity edema with notion of generalized weakness.
The physical examination found a well-appearing woman, hemodynamically stable and afebrile. Abdominal examination revealed a distended abdomen, with collateral venous circulation and the presence of a palpable umbilical nodule. The nodule was firm, fixed, irregularly shaped, and measured 15x10mm. The patient given its painless nature and slow growth did not consider this finding. There were no evidence of hernia, bleeding or ulceration.
The remaining physical examination, including a pelvi- rectal examination, was noncontributory. An upper and lower gastroenterological endoscopy was performed and showed no major abnormalities.
The patient underwent paracentesis, which revealed exudative ascites. Blood tests were normal. However, tumor marker CA125 was markedly elevated (over 4000U/mL).
With the suspicion of a malignant umbilical tumor, a trans-vaginal pelvic ultrasound was performed and showed a mixed, heterogeneous, and hyper vascularized mass on the right side of the uterus. An atrophic uterus with a thickened endometrium was also noticed. Imaging with an abdominal CT scan showed the presence of an umbilical nodule measuring 22.5x16x13 mm (Figure 1). Additionally, pelvic MRI revealed the presence of a mixed retro-uterine mass measuring 49/22/47mm, classified ORADS 5, with peritoneal carcinomatosis and no pelvic lymphadenopathy (Figure 2). The urinary bladder was unremarkable. An additional CT of the thorax was performed for staging and did not reveal any distant secondary metastasis in the lung.
With the suspected diagnosis of a metastatic ovarian cancer, the patient underwent initially an ultrasound-guided micro-biopsy of the accessible umbilical nodule. Histopathological examination showed tumor proliferation arranged in cribriform massifs, and micropapillay structures. There were no psammoma bodies or microcalcifications. Neoplastic cells showed scant eosinophilic cytoplasm, enlarged nuclei, showing conspicuous nucleolus and mild to moderate nuclear atypia (Figure 3).
A panel of immunostains was carried out and showed intense diffuse cytoplasmic staining for cytokeratin (CK) 7 (Figure 4A), nuclear positivity for Wilm’s tumor 1 (WT-1) (Figure 4B), as well as nuclear positivity for hormone receptors (Figure 4C-4D). Tumor cells were negative for CK20. Based on the umbilical cutaneous nodule, the anti-CA-125 positivity, and the imaging methods employed (MRI and CT scan procedures), together with morphology findings and immunohistochemical profile, enabled us to diagnose metastatic serous ovarian carcinoma.
The patient’s case was discussed at the gynaecology/oncology multidisciplinary team meeting. The malignancy was judged inoperable due to the extent of the disease, and the patient was referred to the Oncology Department for palliative chemotherapy. However, the patient’s family declined further therapy for personal reasons (she was very old and will not support chemotherapy).
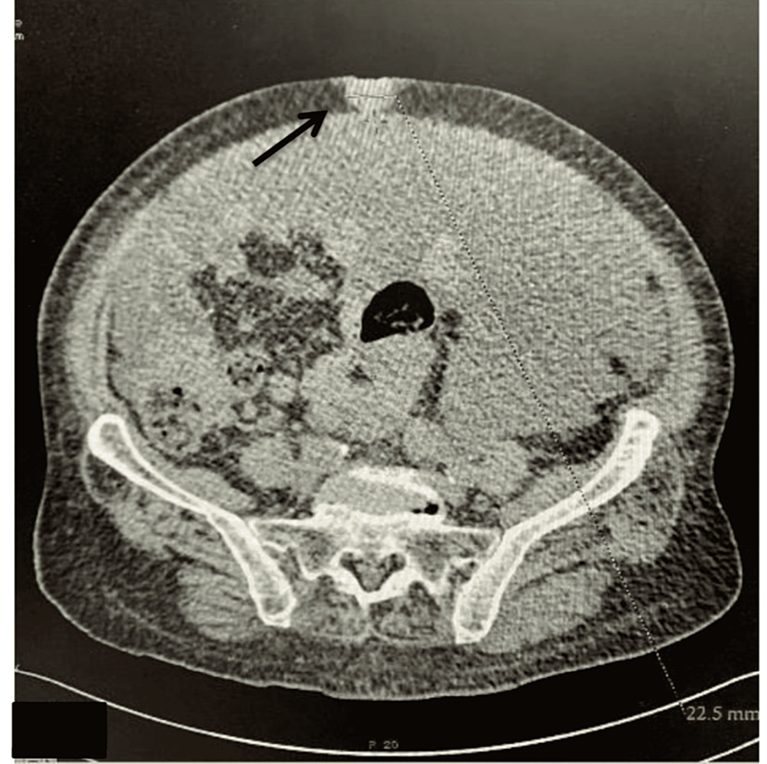
Figure 1: Transverse section of the abdominal CT showing a subcutaneous umbilical nodule of tissue density, well limited measuring 22.5x16x13 mm and very abundant ascites.

Figure 2: Sagittal section of pelvic MRI showing mixed retro-uterine mass measuring 49/22/47mm, classified ORADS 5, enhanced heterogeneously after gadolinium injection.
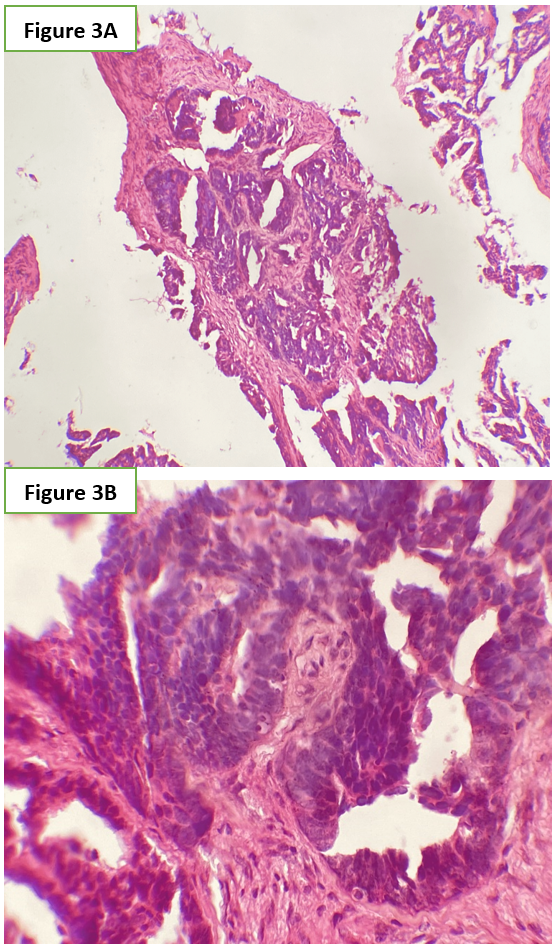
Figure 3: Microscopic examination showing tumor proliferation arranged in cribriform massifs, and micropapillary structures (Figure 3A). In higher magnification, these strictures were lined by neoplastic cells showing scant eosinophilic cytoplasm, enlarged nuclei with mild to moderate nuclear atypia (Figure 3A). (Hematoxylin and Eosin stain, original magnification 3A: ×100 and 3B: × 200).
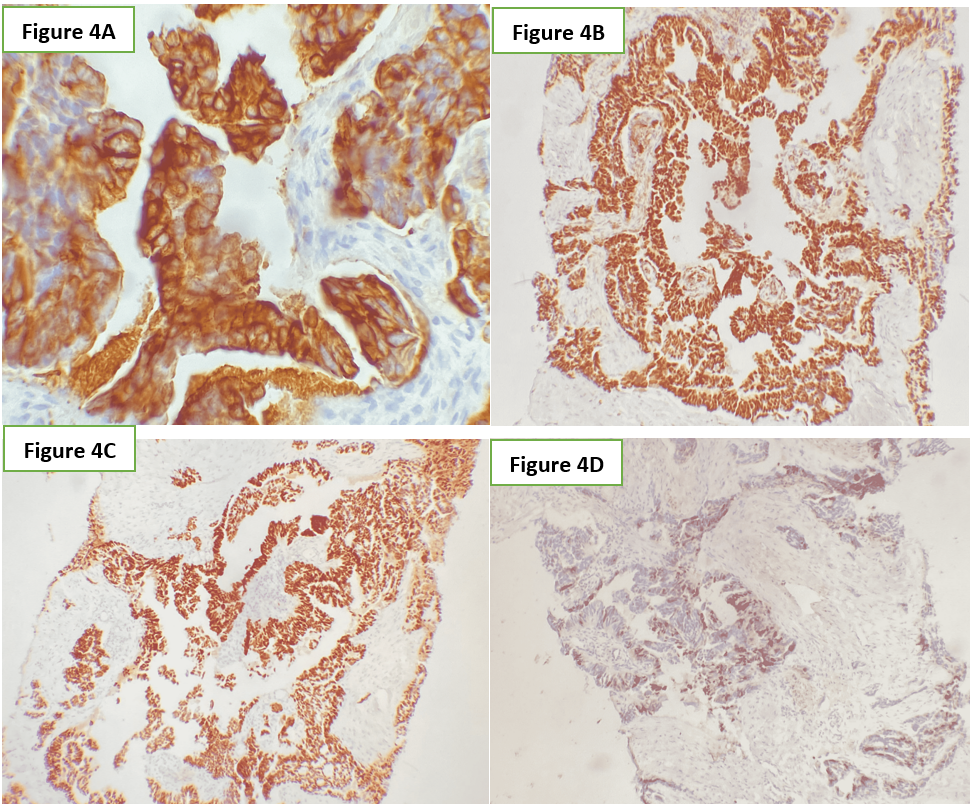
Figure 4: Tumor cells showing intense and diffuse cytoplasmic staining for cytokeratin (CK)7 (4A), nuclear positivity for Wilm’s tumor 1 (WT-1) (4B), as well as nuclear positivity for oestrogen and progesteron receptors (4C-4D). (Immunochemistry stain).
Discussion
SMJN is the term used to describe metastatic nodules found in the umbilical region, and it is most commonly seen in cases of gastrointestinal or gynecological cancers. The name "Sister Mary Joseph's nodule" originated from a nurse named Julia Dempsey, also known as Sister Mary Joseph, who worked as an assistant to Dr. William J. Mayo at Saint Mary's Hospital, which is now known as Mayo Clinic, in the United States. She was the first person to observe the connection between periumbilical nodules and intra-abdominal malignant tumors, although the first official description was documented by Hamilton Bailey in the 11th edition of his book, "Physical Signs in Clinical Surgery" [4].
The mechanism of tumor spread in this context remains poorly understood. Due to its vascularity, connections to embryological remnants, and proximity to the peritoneum, the umbilicus is predisposed to metastatic involvement. For this reason, several hypotheses regarding the pathogenesis have been proposed, including direct invasion of the peritoneum, accidental implantation following surgery, lymphatic or hematogenous spread, or via embryonic remnants in the abdominal wall [5].
The most common primary sites associated with umbilical nodules are usually gastric cancer (30%), colorectal cancer (25%), and pancreatic cancer (18%) in men. In women, the most frequent primary locations are ovarian cancer (34%), endometrial cancer (12%), and colorectal cancer (12%) [1]. Other rare causes have also been reported, such as lymphoma [6] and metastatic prostate cancer [7].
Not all umbilical nodules represent malignant tumors. In some cases, they can be present in benign conditions, and the differential diagnoses should include umbilical hernia, cutaneous endometriosis, and benign tumors like dermatofibromas, papillomas, myxoma, and foreign body granulomas [8]. Since several benign conditions can mimic umbilical metastasis, histological examination of the umbilicus is not only crucial but also guides clinicians in searching for the potential primary site.
While SMJN is a relatively uncommon clinical finding, occurring in only 3% of metastatic cancers, it has been described in recent case reports. In the largest case series involving 34 patients from a university hospital in Tanzania, males outnumbered females by a ratio of 1.4:1. Most patients (70.6%) presented with large umbilical nodules measuring more than 2 cm. The stomach (41.1%) was the most common primary tumor site, with ovarian cancer accounting for 5.9% of SMJN cases [9]. Adenocarcinoma was the most frequently observed histological type in that case series. Since all patients had advanced and metastatic disease, only palliative therapy was provided, resulting in a mortality rate of 32.4%.
Although umbilical metastasis in cases of serous ovarian cancer has been previously reported in the literature [5,10,11], our case differs in several important aspects. SMJN can be present at the time of diagnosis or manifest during disease recurrence. In our case, the umbilical mass was the initial presentation, leading to the diagnosis of metastatic serous ovarian carcinoma. This finding emphasizes the importance of vigilance among clinicians.
Typically, the clinical presentation of SMJN is characterized by an irregular palpable nodule that is often painful, rapidly growing, and of firm or elastic consistency. The nodule may be ulcerated with bloody, purulent, or serous discharge. It can also present as an induration of the subcutaneous tissue [12]. In our case, the umbilical mass appeared to be deeper and was not clinically apparent to the patient due to its painless nature and slow growth.
In cases of isolated umbilical mass, imaging plays a crucial role in establishing a diagnosis. Additionally, fine needle aspiration cytology or core biopsy is necessary as a simple, fast, accurate, and cost-effective diagnostic tool. Histological and immunohistochemical investigations are essential in confirming the diagnosis [13]. The most common histological type is adenocarcinoma (accounting for approximately 75% of cases), while epidermoid, undifferentiated, or carcinoid types are less common. Furthermore, immunohistochemical markers are crucial in determining the origin of unknown primary cancer. In our case, the positivity of monoclonal antibodies such as cytokeratin 7, WT1, and RE suggests a serous ovarian origin.
The prognosis for patients presenting with SMJN is generally poor, as its presence typically indicates advanced and disseminated malignancy, with a mean life expectancy ranging from 2 to 11 months without treatment [14].
The management of the disease should consider patient preferences, clinical condition, and the nature of the primary malignancy. Often, palliative care may be the only option for some patients, as demonstrated in our case presentation. However, in carefully selected cases, more aggressive treatments such as surgery, chemotherapy, and radiotherapy may be beneficial [2]. The patient in this case did not receive any treatment and is currently undergoing strict follow-up without complications.
Conclusion
SMJN is an uncommon clinical sign that underscores the importance of conducting a thorough physical examination of the abdomen, specifically investigating any umbilical lesions, particularly in elderly patients. It frequently indicates the presence of advanced intra-abdominal malignancies.
Due to its superficial location, a biopsy is the most reliable method for accurately diagnosing any suspicious lesion originating from the umbilicus.
The prognosis for patients with SMJN is generally poor, and survival is often limited. Consequently, early detection of the primary cancer at an early stage may improve the outlook and prognosis for patients.
Informed consent statement: Written informed consent for the paper to be published (including images, case history and data) was obtained from the patient/guardian for the publication of this paper, including accompanying images.
Financial and Competing Interests: No conflict of interests declared.
Author’s Contributions: All authors read and approved the final manuscript and were involved in the review and editing of the manuscript.
Grant Information: The authors received no specific funding for this work.
Informed Consent: Written and Verbal consent was attained from the patient for this manuscript.
Conflicts of Interest: The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- Tso S, Brockley J, Recica H, et al. Sister Mary Joseph’s nodule: an unusual but important physical finding characteristic of widespread internal malignancy. Br J Gen Pract, 2013 ; 63: 551-552. 10.3399/bjgp13X673900
- Gabriele R, Conte M, Egidi F, et al. Umbilical metastases: current viewpoint. World J Surg Oncol, 2005; 3: 13.
- De Angeli M, Carosi M, Vizza E, Corrado G. Sister Mary Joseph’s nodule in endometrial cancer: A case report and review of the literature. J Cancer Res Ther, 2019; 15: 1408-1410. 10.4103/jcrt.JCRT_523_18
- Bailey H. Demonstrations of Physical Signs in Clinical Surgery, Williams &Wilkins, Baltimore, Md, USA, 1949. 10.7326/0003-4819-68-1-271_5
- Yang L, Kinloch M, Martin V, Rashidi F. Calcified Sister Mary Joseph nodule as the presenting complaint of advanced low-grade serous ovarian cancer. Radiol Case Rep, 2020; 15: 1638-1642. 10.1016/j.radcr.2020.06.033
- O'Connor-Byrne N, Glavey S, de Freitas D, Quinn J. Sister Mary Joseph nodule in mantle cell lymphoma. Lancet Oncol, 2020; 21: 337. 10.1016/S1470-2045(20)30203-5
- Chahin M, Kogler W, Stack A, Lyons B. Sister Mary Joseph Nodule in a Patient with Advanced Prostate Cancer. J Am Osteopath Assoc, 2021; 120: 476-478. 10.7556/jaoa.2020.075
- Ha DL, Yang MY, Shin JO, Kim HS, Ko HC, Kim BS, et al. Benign Umbilical Tumors Resembling Sister Mary Joseph Nodule. Clin Med Insights Oncol, 2021; 24: 1179554921995022. 10.1177/1179554921995022
- Chalya PL, Mabula JB, Rambau PF, et al. Sister Mary Joseph’s nodule at a university teaching hospital in northwestern Tanzania: a retrospective review of 34 cases. World J Surg Oncol, 2013; 11: 151. 10.1186/1477-7819-11-151
- Mounika P, Shrivastava DS, Diwani D: Umbilical metastasis secondary to ovarian carcinoma - a rare case of sister Mary Joseph nodule. J Evolution Med Dent Sci, 2020; 9: 3343-3344. 10.14260/jemds/2020/734
- Grech A, Abela R. Sister Mary Joseph's nodule. J R Coll Physicians Edinb, 2020; 50: 162-163. 10.4997/JRCPE.2020.218
- Leyrat B, Bernadach M, Ginzac A, Lusho S, Durando X. Sister Mary Joseph Nodules: A Case Report about a Rare Location of Skin Metastasis. Case Rep Oncol, 2021; 8: 664-670. 10.1159/000515298.
- Calongos G, Ogino M, Kinuta T, Hori M, Mori T. Sister Mary Joseph nodule as a first manifestation of a metastatic ovarian cancer. Case Rep Obstetr Gynecol, 2016; 1-4. 10.1155/2016/1087513
- Chiang CH, Lin MH. Sister Mary Joseph nodule associated with pancreatic adenocarcinoma. J Formos Med Assoc, 2015; 114: 92-93. 10.2967/jnmt.119.225961.

