Retroperitoneal Hemangiopericytoma: Case Report and Literature Review
Mauricio Javier Cardona Tobón and Isabel Cristina Brito Rojas*
1General Surgeron, Clínica Universitaria Colombia, Colombia
2General surgery resident, Department of General Surgery, Clínica Universitaria Colombia, Colombia
Received Date: 13/07/2023; Published Date: 06/12/2023
*Corresponding author: Isabel Cristina Brito Rojas, General surgery resident, Department of General Surgery, Clínica Universitaria Colombia, Colombia
Summary
Introduction: Hemangiopericytoma, which is currently included in the category of solitary fibrous tumors, is a rare vascular neoplasm derived from pericytes that is located mainly in the lower extremities, with rare occurrences in the greater omentum or retroperitoneum.
Clinical Case: We present the case of a 50-year-old woman with abdominal pain in whom a hypervascular retroperitoneal mass was documented by imaging, and the pathology report revealed a hemangiopericytoma.
Discussion: Solitary fibrous tumor is a mesenchymal tumor composed of spindle cells, with its origin being poorly understood, and it presents a varied clinical spectrum. Retroperitoneal location is uncommon, and surgical resection is the treatment of choice whenever possible.
Keywords: Hemangiopericytoma; Solitary fibrous tumor; Retroperitoneum; Surgical resection
Introduction
Solitary fibrous tumor is a mesenchymal tumor composed of spindle cells, whose origin is poorly understood. It exhibits fibroblastic and myofibroblastic differentiation, as well as intermediate malignant potential, known to present a broad histopathological spectrum [1]. It was first mentioned by Wagner in 1870 in the pleura; however, the first description was made by Klemperer in 1931, who named it fibrous mesothelioma [2]. Subsequently, in 1942, Stout and Murray were the first to discuss hemangiopericytoma [3].
Solitary fibrous tumors represent less than 2% of all soft tissue tumors, less than 1% of vascular tumors, and approximately 5% of all sarcomatous tumors [4]. The age of presentation varies, with an average age at diagnosis of 45, and the distribution is equal in both sexes [4]. Retroperitoneal location is extremely rare, with evidence of only 9 published cases in literature [5].
Lesions can present as painless, slow-growing masses or may cause symptoms due to mass effect and pressure on adjacent structures [6]. Since these tumors can arise in various locations, the differential diagnosis is broad and largely depends on the location [7].
Primary surgical resection is the treatment of choice whenever possible, and no benefit has been shown from systemic chemotherapy [3]. Radiation therapy can improve local control rates postoperatively but may not achieve complete disease remission [4].
Case Report
A 50-year-old female patient with a history of hypercholesterolemia, vitamin D deficiency, and osteoporosis presented with a complaint of lower right-sided abdominal pain associated with nausea, dizziness, a single episode of vomiting, and a sensation of dry mouth. Physical examination revealed tenderness on palpation in the right iliac fossa with a perceived mass in said area and in the mesogastrium, without signs of peritoneal irritation.
In light of these findings, total abdominal ultrasound studies were initiated, which showed a heterogeneous mass apparently dependent on the right adnexa with dimensions of 80 x 60 x 83 mm (Figure 1). Further imaging studies were requested. Magnetic nuclear resonance imaging demonstrated a solid mass occupying the right iliac fossa with a diameter of 9 x 9.5 x 5 cm (L x T x AP), predominantly low intensity signal on T1 and high intensity on T2, with intense enhancement after the administration of contrast agent in the arterial phase. It was associated with multiple serpiginous vascular dilations around it and contacting the inferior contour of liver segment VI (Figure 2). Abdominal computed tomography with contrast documented a retroperitoneal mass image measuring 96 x 62 mm on the right psoas muscle, exerting compressive effects on adjacent structures. It had an adequate cleavage plane with the right colon and iliac vessels (Figure 3). No masses nor adenomegalies were found on the chest tomography.
Based on the imaging results, it was decided to perform open resection of the lesion. During the procedure, a highly vascularized retroperitoneal mass measuring 9 x 9 x 5 cm was identified, extending to the right iliac fossa, the lower part of the ipsilateral flank and the lateral wall. It was in close proximity to the psoas muscle, right ureter, and lower pole of the right kidney, without compromising vascular structures nor the liver. The surgery was completed without complications, and the patient had an uneventful postoperative recovery.
The pathology report of the surgical specimen revealed a diagnosis of solitary fibrous tumor / hemangiopericytoma, with low histological grade and no vascular or perineural invasion. The surgical margins were free from tumor involvement.

Figure 1: Total abdominal ultrasound. Mass apparently dependent on the right adnexa.
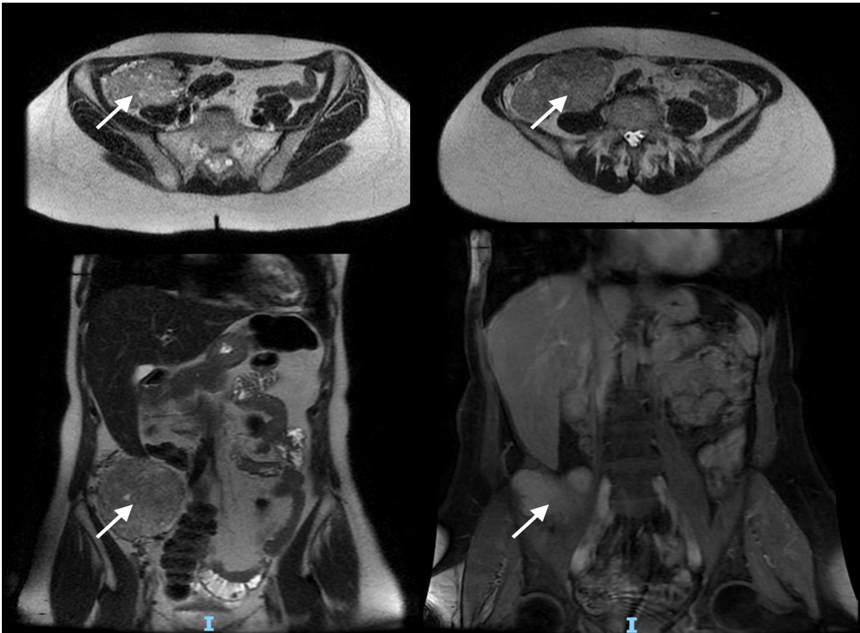
Figure 2: Abdominal magnetic resonance imaging. Mass in the right iliac fossa measuring 9x9.5x5 cm in contact with hepatic segment IV, with multiple serpiginous vascular dilations around it.
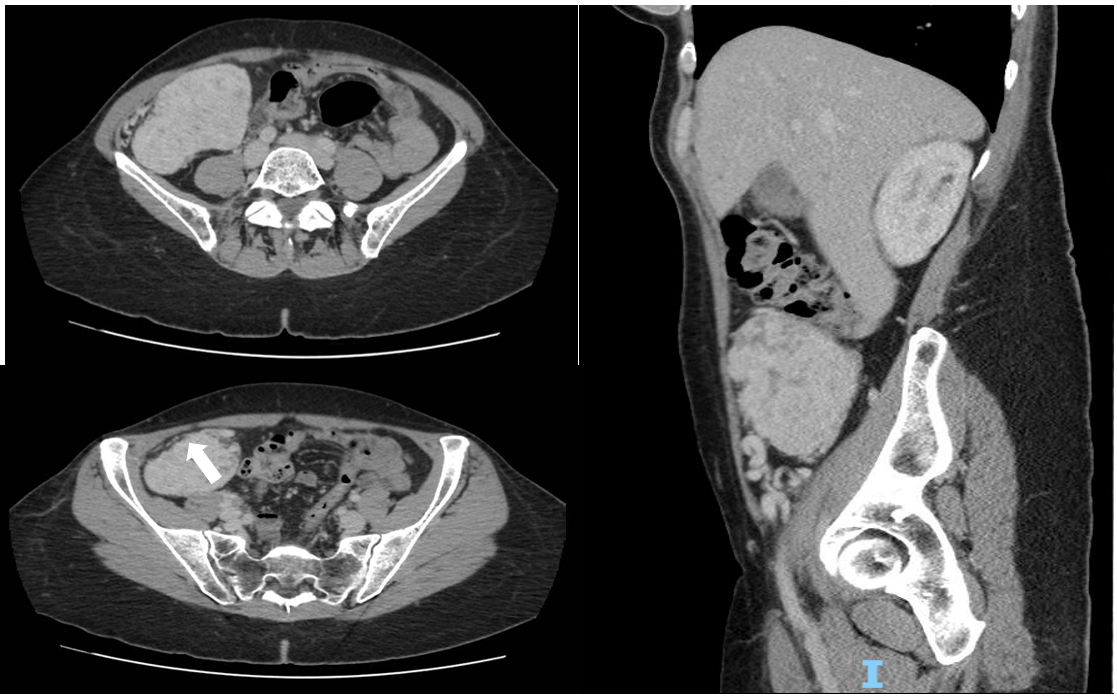
Figure 3: Contrast-enhanced abdominal tomography. Hypervascular retroperitoneal mass measuring 96x62 mm on the psoas muscle, exerting compressive effects on adjacent structures.
Discussion
Hemangiopericytomas are rare vascular neoplasms derived from Zimmerman pericytes, smooth muscle cells that line capillaries, post-capillary venules, and sinusoidal spaces [8]. Most neoplasms previously called hemangiopericytomas are now included in the category of solitary fibrous tumors, although some strictly defined categories of hemangiopericytoma are still recognized as distinct pathological entities [6]. The fourth edition of the World Health Organization's Classification of Tumors of Soft Tissue and Bone, published in February 2013, merged these two entities into a single tumor. However, some pathologists continue to maintain the old classification, despite the morphological and pathological characteristics of the lesions being related [9].
These tumors can be located in the lower extremities (34.9%) and the pelvic cavity (24.5%). The greater omentum is an uncommon site of occurrence, with approximately 20 cases described in the literature [4].
They rarely present with symptoms of hypoglycemia due to the secretion of insulin-like growth factors [6]. In particular, intra-abdominal and cerebromeningeal locations are associated with an aggressive clinical course. Conversely, those located in the pleuropulmonary region show a lower tendency for distant metastasis, which may be related to microenvironmental and epigenetic factors [1].
Macroscopically, solitary fibrous tumors appear as a well-circumscribed rubbery mass with clear evidence of fibrotic qualities. Occasionally, a fish flesh appearance is described [10]. Histologically, they exhibit a combination of hypercellular and collagenous areas. In cases where assessing malignancy based solely on morphology and immunohistochemical characteristics is difficult, markers such as CD34, CD99, Bcl-2, and STAT6 can be useful [9]. Occasionally, they may be positive for Epithelial Membrane Antigen (EMA) and Smooth Muscle Actin (SMA), and generally negative for cytokeratin, S100, and desmin.
The NAB2-STAT6 fusion genes are specific to solitary fibrous tumors, and their detection can be useful in challenging diagnostic cases. Immunohistochemistry for STAT6 has recently been introduced as a substitute for detecting the fusion gene. The intense and diffuse nuclear staining of STAT6 is an important characteristic of these tumors, observed in over 90% of cases. Less than 10% of other spindle cell tumors in different body locations have tested positive for STAT6, most of which do not exhibit the same diffuse and intense staining as seen in solitary fibrous tumors [2].
Imaging in these patients typically shows a mass with heterogeneous enhancement on computed tomography, appearing isointense on magnetic resonance imaging. In some cases, the feeding vessels of the lesion can be visualized on angiography. Some of these tumors have shown muscle and nearby vascular structure invasion, as well as destruction of ethmoid cells and nasal turbinates [7].
According to the literature, these tumors have favorable long-term outcomes following primary surgical resection, and systemic chemotherapy has not shown any benefit. However, when they are located in sites such as the greater omentum, they tend to have a higher recurrence rate in local or distant sites [3]. Due to their characteristics, anti-angiogenic inhibitors have emerged as a therapeutic alternative [3]. Diffuse expression of platelet-derived growth factor, as well as expression of basic fibroblast growth factor and transforming growth factor-alpha, has been observed, suggesting that various factors responsible for endothelial and vascular proliferation may contribute to angiogenesis in these patients [11].
Radiation therapy can improve local control rates postoperatively but may not achieve complete disease remission. It may be recommended for tumors that exhibit criteria for malignancy and as an alternative treatment for patients with criteria for irresectability or recurrence [4]. In a study conducted by Krengli et al., it was concluded that the addition of radiation therapy could improve both local control and disease-free survival rates in patients who underwent surgery for extracranial pathology. However, subgroup analysis showed that the advantage of adding radiation therapy was more significant for patients with extremity and superficial trunk locations than for intrathoracic or retroperitoneal tumors [12].
Conclusion
Solitary fibrous tumors are uncommon soft tissue tumors with a predominant involvement of the lower extremities, while retroperitoneal localization is rare. Clinical manifestations are varied and may be secondary to mass effect and compression of adjacent structures. Surgical resection is the cornerstone of treatment, with chemotherapy being of limited usefulness and reserving radiation therapy for special cases.
Authorship Criteria
Concept and design of study or acquisition of data or analysis and interpretation of data:
Dr Mauricio Javier Cardona Tobon
Dra Isabel Cristina Brito Rojas
Drafting the article or revising it critically for important intellectual content:
Dra Isabel Cristina Brito Rojas
Final approval of the version to be published:
Dr Mauricio Javier Cardona Tobon
Dr Isabel Cristina Brito Rojas
Conflicts of Interest/ Competing Interests: The authors declared that they had no conflict of interest
Grant Information: There was no funding for the development of the project.
References
- Yamada Y, Kohashi K, Kinoshita I, Yamamoto H, Iwasaki T, et al. Clinicopathological review of solitary fibrous tumors: dedifferentiation is a major cause of patient death. Virchows Archive, 2019; 475(4): 467-477.
- Geramizadeh B, Marzban M, Churg A. Role of Immunohistochemistry in the Diagnosis of Solitary Fibrous Tumor, a Review. Iran J Pathol, 2016; 11(3): 195-203.
- Archid R, Schneider C, Adam P, Othman A, Zieker D, Königsrainer A. Hemangiopericytoma/solitary fibrous tumor of the greater omentum: A case report and review of the literature. International Journal of Surgery Case Reports, 2016; 23: 160-162.
- Vasdeki D, Bompou E, Diamantis A, Anagnostou A, Tepetes K, Efthimiou M. Haemangiopericytoma of the greater omentum: a rare tumor requiring long-term follow-up. Journal of Surgical Case Reports, 2018; 5: 1–3.
- Zhou Y, Chu X, Yi Y, Tong L, Dai Y. Malignant solitary fibrous tumor in retroperitoneum. A case report and literature review. Medicine, 2017; 96: 11-14.
- Thway K, Ng W, Noujaim J, Jones R, Fisher C. The Current Status of Solitary Fibrous Tumor: Diagnostic Features, Variants, and Genetics. Int J Surg Pathol, 2016; 24(4): 281-292.
- Olson N, Linios K. Dedifferentiated Solitary Fibrous Tumor. Arch Pathol Lab Med, 2018; 142: 761-766.
- Ratneswaren T, Hogg F, Gallagher M, Ashkan K. Surveillance for metastatic hemangiopericytoma-solitary fibrous tumors-systematic literature review on incidence, predictors and diagnosis of extra-cranial disease. J Neurooncol, 2018; 138(3): 447-467.
- Biddau C, Cereser L, Paliogiannis P, Terrosu G, Uzzau A. Solitary Fibrous Tumor of the Omentum: Presentation of a Case and Literature Review. Surgery, Gastroenterology and Oncology, 2020; 25(3): 155-162.
- Yalcin C, Tihan T. Solitary Fibrous Tumor/Hemangiopericytoma Dichotomy Revisited: A Restless Family of Neoplasms in the CNS. Adv Anat Pathol, 2016; 23: 104–111.
- Park M, Araujo D. New insights into the hemangiopericytoma/solitary fibrous tumor spectrum of tumors. Current Opinion in Oncology, 2009; 21: 327–331.
- Krengli M, Cena T, Zilli T, Jereczek -Fossa B, De Bari B, et al. Radiotherapy in the treatment of extracranial hemangiopericytoma/solitary fibrous tumor: Study from the Rare Cancer Network. Radiotherapy and Oncology, 2020; 144: 114-120.

