Pilocytic Astrocytoma Located in Medulla Oblongata in Pediatric Age
Paulino Insumbo*, Khouchoua S, Irineu E B Ferreira, Rabileh Y M, Kessi E, Addad
Department of radiology, Pediatric hospital, UHC IBN Sina Mohamed V University Rabat, Morocco
Received Date: 09/07/2023; Published Date: 01/12/2023
*Corresponding author: Paulino Insumbo, Department of radiology, Pediatric hospital, UHC IBN Sina Mohamed V University Rabat, Morocco
Abstract
Pilocytic astrocytoma are considered the most common benign posterior fossa brain tumors in children and adolescents. Its location on the medulla oblongata, however remains a life threatening and extremely rare entity with very poor prognosis. It represents about 30% of all posterior fossa neoplasms. Clinical presentation along with imaging findings on both Magnetic Resonance Imaging (MRI) and computed tomography with intravenous contrast agent administration are key to visualize and correctly diagnose pilocytic astrocytoma’s. In fact, imaging is particularly helpful to delineate the PA from the surrounding healthy brain tissue. Histopathological analysis and especially immuno histochemistry with identification of key genetic alterations [1] confirm the diagnosis. Surgery is the treatment of choice; resection may provide reasonable survival rates. In this article we choose to present a circumscribed and rare form of pilocytic astrocytoma located in the bulb.
Keywords: Pilocytic astrocytoma; Medulla oblongata; Brainstem; Posterior fossa
Clinical Image
Imaging plays a key role in the diagnosis of pilocytic astrocytomas. Magnetic Resonance Imaging (MRI) and computed tomography with intravenous contrast agent administration are key to visualize and correctly diagnose pilocytic astrocytomas. In fact, imaging is particularly helpful delineating the PA from the surrounding healthy brain tissue [2]. We present the case of a 5-year-old patient. Bedridden patient from rural origin, who was brought by family member complaining of loss of muscle strength in upper and lower limbs lasting two months of progressive onset, associated with a history of headaches and vomiting, accompanied with vertigo, ataxic gait, diplopia and oculomotor paralysis.
Pilocytic Astrocytoma (PA) represents the most common primary benign tumor of the posterior fossa. According to the World Health Organization (WHO) classification it is considered a low-grade brain tumor [4]. It develops from star-shaped brain cells called astrocytes. Astrocytes are found within the brain and spinal cord, forming tissue that surrounds and protects other nerve cells. Clinical presentation will vary depending on the size and the location of the tumor. Symptoms result from increased brain pressure and include headaches, nausea, vomiting, ataxia and vision disorders [3]. The emergency doctor on duty requested a cerebral TDM, without contrast, with little information, which showed a heterogeneous expansive process located in the medulla oblongata (Figure 1). The following days an MRI, demonstrating an expansile process of posterior fossa, located in the medulla oblongata, with two components: (Figure 2), solid hyper intense on T2 and FLAIR component, heterogeneously enhanced after contrast media injection and a cystic hyper intense on T2, hypo intense on T1 and intermediate signal intensity on FLAIR component, with peripheral wall enhancement after contrast media injection. Surrounding perilesional edema can be depicted in T2 and FLAIR hyper intensity. Mass effect on the adjacent structures can be identified : on the inferior aspect of the fourth ventricle which is collapsed, as well as on the cerebellar tonsils. It is responsible for an effacement of the cerebello medullary cisterns, with tonsillar herniation through the foramen magnum. Spectroscopy shows a moderate decrease of the Choline/NAA ratio, and elevation of myo inositol peak and lactates on short-echo. No associated supra tentorial hydrocephalus, midline shift or other intraparenchymal signal abnormalities were found.
A biopsy was performed and the results of the pathological anatomy confirm the radiological diagnosis, and the patient is undergoing treatment.
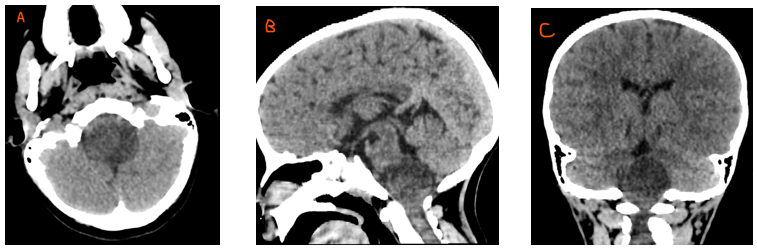
Figure 1: axial(a), sagittal (b) and coronal (c); non enhanced CT showing an expansile tumor centered on the brainstem bulb featuring a cystic and solid component. Mass effect on the fourth ventricle is present with no significant hydrocephalus.

Figure 2: Sagittal T1 weighted images, coronal FLAIR, Axial T1 fat suppressed after contrast media injection and axial T2 and DWI showing an expansile medulla oblongata mass with a cystic and solid component.
Conclusion
Pilocytic astrocytoma represents less than 15% of tumors of posterior cerebral fosse, more location in the medulla oblongata is rare [5]. present different characteristics in pediatric population. A majority of PAs have an alteration in the Ras/ERK pathway. In sporadic tumors, KIAA1549-BRAF fusion is the most [4]. The anotomo pathological diagnosis and imagering remains fundamental for the location and volume of the lesion, but the prognosis is excellent even in the long term.
References
- Alice Métais, Andrey Rousseau. Le diagnostic histo-moleculaire des tumeurs gliales et glioneuronales, departement de Pathologie cellulaire et tissulaire, CHU Angers, 2 rue larrey, 49100, Angers, France.
- Philippe Schucht, levin Hani. Astrocytome pilocytique.
- Primary spinal pilocytic astrocytoma: clinical study with long-term fallow-up in 16 patients and a literature review.
- Alice Métais, Audrey Rousseau. Le diagnostic histo-moléculaire des tumeurs gliales et glioneuronales.
- Miriam Bornhorst, Didier Frappaz, Roger J Parker. Pilocytic astrocytoma, 2016.

