Holocord Abscess with Bulbo-Medullary Extension Associated with a Congenital Dermal Sinus in an 18-Month-Old Child
Ashwin Rai1 and Aditya Rai2,*
1Department of Neurosurgery, Jawaharlal Institute of Post-graduate Medical Education and Research (JIPMER), Puducherry, India
2Sri Lakshmi Narayan Institute of Medical Sciences (SLIMS), Puducherry, India
Received Date: 06/07/2023; Published Date: 29/11/2023
*Corresponding author: Aditya Rai, MBBS, Sri Lakshmi Narayan Institute of Medical Sciences (SLIMS), Puducherry, India
Abstract
Holocord abscess is a rare occurrence and one with bulbo-medullary extension is even rarer. Till date only a handful of case reports of holocord abscess with bulbo-medullary extension has been reported. We describe a rare case of intramedullary abscess with bulbo-medullary extension in an 18-month-old child, stemming from a congenital dermal sinus communicating with the spinal canal in the sacral region. We have described the presenting signs and symptoms, evaluation and multi-modal management of intramedullary abscess which resulted in gradual improvement of the patient’s clinical condition leading to subsequent discharge from the hospital with considerable neurological improvement. An acute febrile disease associated with acute or rapid onset neurological deficit that is associated with dermal sinus or spinal dysraphism indicates an intramedullary abscess which should be investigated with relevant radiological imaging (MRI). The treatment involves a combination of surgical abscess evacuation and antimicrobial therapy along with intensive care and support.
Keywords: Congenital dermal sinus; Holocord abscess; Bulbo-medullary abscess; Case Report
Introduction
Congenital Dermal Sinuses (CDS) are squamous–epithelium lined tracts and form due to disorders of neural disjunctions resulting from incomplete separation of cutaneous ectoderm from the underlying neuroectoderm [1]. The incidence of CDS is approximately 1 in 2,500 live births without gender predilection [2]. They could be located along the length of midline neuraxis but are most commonly found in the lumbosacral and occipital regions. The reason for less frequent localization in the cervical region appears to have embryological basis, wherein the fusion of the neural tube begins in the cervical region and then proceeds both cranially and caudally, closing at the cephalic end. Usually, the tract from CDS courses cephalad and extends for a variable course and could end blindly in the subcutaneous tissues, dura, spinal cord, or nerve roots [3]. The majority of CDS present clinically in the first decade, usually below 5 years, because of high risk of infection [2,3]. Clinical manifestations range from being asymptomatic to a discharging sinus, local inflammation, recurrent meningitis or neurological dysfunction [4]. Cutaneous markers of a CDS could be abnormal cutaneous pigmentation, angiomas, subcutaneous lipoma, hairy nevus, and skin tags [3,5]. Intramedullary spinal cord abscess (ISCA) is the rarest and the most serious complication of a CDS and may lead to permanent neurological deficits. ISCA are rare central nervous system infections in children and a holocord abscess involving the entire length of spinal cord is even rarer. First described by Hart in 1830, fewer than 150 cases ISCA have been reported since then [6,7]. Intramedullary abscess in the spinal cord commonly occurs secondary to a primary focus of infection The infective foci commonly seen are pneumonitis, genitourinary tract infection, peripheral skin infections, endocarditis and meningitis. Abscesses are also associated with dermoids, epidermoids, infected dermal sinus tract, ependymomas and spinal dysraphism. Common presenting features include fever and acute onset/rapidly progressive neurological deficits. Standard management consists of combined medical and surgical treatment.
History and Examination
An 18-month-old male child, with normal development and no prior hospital admissions, presented to paediatric emergency with complaints of fever for 7 days, for which he was receiving oral antibiotics. On the 4th day of fever, child’s mother noticed weakness in both lower limbs as the child was not able to walk or stand by himself, which he would otherwise normally do. This was associated with poor feeding, lethargy and reduced interaction with parents.
At arrival patient’s temperature was 98°F, had tachycardia of 140/minute and blood pressure of 100/60. A primary physical evaluation at the emergency department revealed a poorly compliant and uncooperative child with no spontaneous movements of the lower limbs. A pre-sacral sinus with frank purulent discharge was also noted. Central nervous system (CNS) examination revealed reduced tone reduced in all 4 limbs. The lower limbs were flaccid and areflexic; muscle strength was Medical Research Council (MRC) grade 0/5 in lower limbs and MRC grade 3/5 in upper limbs. Intercostal muscle weakness was present. There was graded sensory loss to pain below T-10 level. Progressive ascending paralysis was noted during the course of illness as the patient developed progressive shallow breathing with paradoxical breathing pattern which was suggestive of intercostal muscle weakness. He was intubated in view of impending respiratory failure. He also had a poor gag reflex.
Evaluation and Treatment
The history, examination and the course of the illness, was suggestive of an ascending infection from the pre-sacral sinus leading to infectious myelitis. Lumbar puncture was performed, which yielded frank purulent discharge. Exudate cultures showed Klebsiella pneumoniae growth and antibiotics sensitive to K. pneumoniae were started. MRI brain and whole spine revealed the sinus tract communicating with the spinal canal with holocord abscess in the sacral segment, extending to the bulbo-medullary junction. Ballooning of the spinal cord throughout its length was also observed (Figures 1- 3).
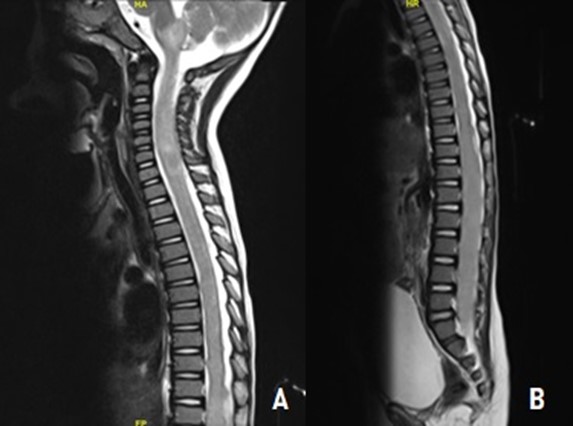
Figure 1: A - MRI spine sagittal view showing extension of holocord abscess into the bulbo-medullary junction. B - MRI spine sagittal view with holocord abscess showing ballooning of spinal cord throughout its length.
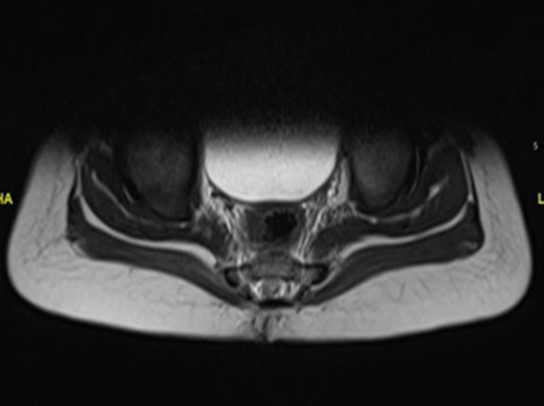
Figure 2: Axial view showing dermal sinus in the sacral region with spinal canal communication.

Figure 3: Sagittal view of the dermal sinus with spinal canal communication.
The patient underwent urgent neurosurgical intervention. A midline skin incision was made from L3 to S1, encircling the dermal sinus ostium. Spina bifida was noted at L5 level and the dermal sinus was seen communicating with a defect between L5 and S1. L3 to L5 laminectomy was performed, followed by durotomy from L3 to L5. Around 30 ml of pus drained after opening thecal sac. Thorough wash was given with the help of a drain placed in thecal sac. After abscess drainage, dissection of the sinus was performed followed by water tight closure of the dura, subcutaneous tissue and skin in layers over the indwelling drain. Bacterial culture specific antibiotics were continued. Post-operative MRI showed adequate drainage of abscess from the thoracolumbar segments, but the cervical cord abscess which was extending into the medulla was still persisting (Figure 4). The patient showed mild improvement in the motor power in both upper and lower limbs, but not in the intercostal muscle weakness.
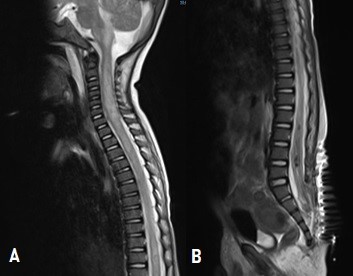
Figure 4: A - Post lumbar laminectomy and abscess evacuation MRI showing residual abscess in the cervical cord and medulla. B - MRI showing adequate abscess drainage in the thoraco-lumbar segments.
A second surgery was done to address the residual abscess in the cervical cord and medulla. Skin incision was made from inion to C7 spinous process. A 1x3 cm sub-occipital craniotomy with C1 arch excision and C2 to C5 laminectomy was done for adequate exposure Dura was thickened and inflamed sub-occipital and cervical region. Dura was opened up in linear fashion, following which 20 ml of pus was drained from cisterna magna and the cervico-medullary region. Yellowish coloured cyst wall was seen lining cisterna magna along with arachnoid adhesions, which were released. Intra-operative ultrasound was used to localise the abscess in the cervical cord region, following which a midline myelotomy was made from cervico-medullary junction to C5 level. A lengthy myelotomy was required for adequate pus drainage. Around 20 ml of pus was drained, following which thorough wash was given using a drain which was not kept in-situ. Water tight closure of the dura, subcutaneous tissue and skin was done in layers. Post-operative MRI showed adequate drainage of abscess from the medullary and cervical cord segments (Figure 5). Bacterial culture sensitive antibiotics were continued in the post-operative period for another 6 weeks.

Figure 5: A - Post cervical laminectomy and abscess drainage MRI showing adequate abscess drainage from the cervical and medullary segments. B - MRI showing reduction in the cord thickness in thoraco-lumbar segments.
Course of illness and outcome
In view of prolonged ventilator requirement due to intercostal muscle weakness, the patient underwent tracheostomy and was subsequently weaned off ventilator support as the intercostal muscle function improved and he was able to maintain oxygenation on room air with a tracheostomy. In due course of time, the patient was de-cannulated and no longer required tracheostomy. The patient also had neurogenic hypertension which was managed with calcium channel blockers and alpha-blockers (Amlodipine and Prazosin). The antihypertensive drugs were tapered gradually as the blood pressure normalized. The patient had also developed neurogenic bladder. Urodynamic study revealed findings suggestive of overactive bladder, which was managed with oxybutynin. Upper and lower limb muscle strength had improved to MRC 4/5 and 3/5 respectively. Intercostal muscle strength had also improved. He did not have respiratory distress and was able to take feeds by himself. He was later stepped down from the pediatric intensive care unit to ward and was discharged after a hospital stay of 2 months.
Discussion
ISCA is a rare form of spinal cord infection, especially in children [8]. The most common mode of spread of infection is hematogenic spread, however, contiguous spread due to Congenital Dermal Sinus (CDS) can be seen in around half the cases reported [9]. CDS is an uncommon form of spinal dysraphism, that can be significantly morbid if left untreated and can lead to CNS infections ranging from recurrent meningitis to holocord abscess [3,10]. The microbiology of ISCA is diverse and various microorganisms have been isolated, namely; Staphylococcus, Streptococcus pneumonia, Hemophilus, Proteus, Listeria, Actinomyces, Pseudomonas, Klebsiella and Mycobacterium tuberculosis [11]. High degree of clinical suspicion is crucial for diagnosis of ISCA. The diagnostic triad for ISCA; fever, pain, and neurological deficits, is present in most of the cases. However, it’s absence does not exclude the diagnosis of ISCA [12]. Prompt clinical examination with radiological investigations in the form of MRI spine and surgical intervention coupled with a longer duration of antibiotic therapy remains the gold standard of management to achieve good neurological outcome [7]. Recurrence of ISCA is seen in about 25% of the cases [13]. In our case, an 18-month-old child presented with acute febrile illness with noticeable neurological deficit with a congenital dermal sinus. Radiological and microbiological evaluation led to the diagnosis of ISCA with bulbo-medullary extension. Prompt neurosurgical intervention and antimicrobial treatment along with careful intensive care unit management resulted in a satisfactory neurological outcome.
Conclusion
In conclusion, an acute febrile disease associated with acute or rapid onset neurological deficit, that is associated with spinal defects should be investigated with proper radiological imaging to rule out ISCA and treated with a combination of surgical abscess evacuation and antimicrobial therapy along with intensive care and support.
Conflict of Interest Statement
Dr Ashwin Rai has been working as a Senior Resident in the Department of Neurosurgery at JIPMER for the last 3 years. Dr Aditya Rai has been working as an intern at SLIMS for the last 1 year, before which he was in Medical School at the same institution. The authors have no conflicts of interest to declare.
Funding Sources: No funding was required for the production of this manuscript.
Author Contributions: Dr Ashwin Rai contributed towards conceptualizing the manuscript and gathering the data. Dr Aditya Rai and Dr Ashwin Rai both contributed towards compiling, writing and editing the manuscript.
Patient Informed Consent: The necessary patient informed consent was obtained in this case.
References
- Ackerman LL, Menezes AH, Follett KA. Cervical and Thoracic Dermal Sinus Tracts: A Case Series and Review of the Literature. Pediatr Neurosurg, 2002; 37: 137–147. https://doi.org/10.1159/000064399.
- Dev R, Husain M, Gupta A, Gupta RK. MR of multiple intraspinal abscesses associated with congenital dermal sinus. Am J Neuroradiol, 1997; 18: 742–743.
- Al Barbarawi M, Khriesat W, Qudsieh S, Qudsieh H, Loai AA. Management of intramedullary spinal cord abscess: experience with four cases, pathophysiology and outcomes. Eur Spine J, 2009; 18: 710–717. https://doi.org/10.1007/s00586-009-0885-0.
- Morandi X, Mercier P, Fournier H-D, Brassier G. Dermal sinus and intramedullary spinal cord abscessReport of two cases and review of the literature. Childs Nerv Syst, 1999; 15: 202–207. https://doi.org/10.1007/s003810050370.
- Benzil DL, Epstein MH, Knuckey NW. Intramedullary Epidermoid Associated with an Intramedullary Spinal Abscess Secondary to a Dermal Sinus. Neurosurgery, 1992; 30: 118.
- J H. Case of encysted abscess in the center of the spinal cord. Dublin Hosp Rep 1830; 5: 522–524.
- Simon JK, Lazareff JA, Diament MJ, Kennedy WA. Intramedullary abscess of the spinal cord in children: a case report and review of the literature. Pediatr Infect Dis J, 2003; 22: 186–192. https://doi.org/10.1097/01.inf.0000048910.19136.49.
- Chan CT, Gold WL. Intramedullary Abscess of the Spinal Cord in the Antibiotic Era: Clinical Features, Microbial Etiologies, Trends in Pathogenesis, and Outcomes. Clin Infect Dis, 1998; 27: 619–626. https://doi.org/10.1086/514699.
- Bunyaratavej K, Desudchit T, Pongpunlert W. Holocord intramedullary abscess due to dermal sinus in a 2-month-old child successfully treated with limited myelotomy and aspiration. Case report. J Neurosurg, 2006; 104: 269–274. https://doi.org/10.3171/ped.2006.104.4.269.
- Ramesh V, Karthikeyan K, Kitchanan S, Sriraman B. Holocord abscess in association with congenital dermal sinus. J Pediatr Neurosci, 2013; 8: 198–198.
- Erşahin Y. Intramedullary abscess of the spinal cord. Childs Nerv Syst, 2003; 19: 777. https://doi.org/10.1007/s00381-003-0803-4.
- Bavdekar SB, Rao N, Kamat JR. Intramedullary spinal cord abscess. Indian J Pediatr, 1997; 64: 428–431. https://doi.org/10.1007/bf02845220.
- Mohindra S, Sodhi HB, Aggarwal A. Management problems of intramedullary holocord abscess: An illustration in a pediatric case. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg, 2011; 28: 637–640. https://doi.org/10.1007/s00381-011-1645-0.

