A Rare Case of Non-24-hour Sleep-Wake Rhythm Disorder in A Sighted Patient
Xinhang Tu1,*, Victor Peng2 and Jennifer So3
1MedStar Health, Baltimore, MD, US
2Sleep Disorders Center, University of Maryland Medical Center, Baltimore, MD, US
3University of Maryland Sleep Laboratory, Division of Pulmonary, Critical Care and Sleep Medicine, University of Maryland School of Medicine, Baltimore, MD, US
Received Date: 06/07/2023; Published Date: 28/11/2023
*Corresponding author: Xinhang Tu, MBBS, MedStar Health, Baltimore, MD, US
Abstract
Non-24-hour sleep-wake rhythm disorder (N24SWD) occurs when the circadian rhythm does not match the natural 24-hour period, leading to a shifting sleep-wake schedule which inevitably causes great disturbance of daily activities. It was first recognized in and is most prevalent in blind individuals. Although the prevalence of N24SWD is unknown in sighted people, it is thought to be rare [1]. Also, it is related to psychological diseases and the use of certain medications. We present a case of a sighted patient with psychiatric comorbidity who presented with excessive sleepiness since preadolescence, was found to have N24SWD.
Keywords: Non-24-hour sleep-wake rhythm disorder; N24SWD; Circadian sleep-wake rhythm disorders; Circadian dysfunction; Circadian rhythm; Sighted patient
Introduction
Like most mammals, humans utilize an intrinsic clock that controls daily physical, mental and behavioral cycles, known as the circadian rhythm. For most people, a normal circadian rhythm is about 24.2 hours long, which aligns with earth's natural light-dark cycle. When there is dysychrony between the intrinsic clock and the desired sleep-wake times, circadian sleep-wake rhythm disorders may arise. These include delayed sleep-wake phase disorder, advanced sleep-wake phase disorder, non-24-hour sleep-wake rhythm disorder, irregular sleep-wake rhythm disorder, jet lag disorder and shift work disorder. Non-24-hour sleep-wake rhythm disorder (N24SWD) occurs when the circadian rhythm does not match the natural 24 hour period, leading to a shifting sleep-wake schedule which inevitably causes great disturbance of daily activities. It was first recognized in and is most prevalent in blind individuals.It is reported that over half of fully blind patients may have N24SWD [1]. In a study of 127 blind women, 39% had N24SWD among the 41 participants without light perception, and 9% had N24SWD in those with light perception.[2] We present a case of a sighted patient who has N24SWD since preadolescence with concurrent bipolar disorder.
Report of Case
A twenty-nine-year-old woman with bipolar disorder on Bupropion and Lamotrigine presented to sleep clinic for excessive daytime sleepiness and irregular sleep schedule. She has been struggling with irregular sleep schedule since age 12, with continued worsening symptoms over time. During her teenage years she often fell asleep at school, and she felt the sleepiness could be associated with psychotropic medication regimen. She was not able to finish college due to untreated depression and bipolar disorder. The patient also had difficulty focusing during daytime which severely interfered with her work as a computer graphics artist. She denies cataplexy, hypnagogic hallucinations or sleep paralysis, no symptoms concerning for restless leg syndrome. No history of shift work or abnormal movement/behavior problems during sleep. According to the sleep App on her phone, her bedtime is variable, shifting about 1-2 hours/day. Her rise time maintains a consistent interval with her bedtime (Figure 1- sleep diary). Her daily total sleep time varies between 7-12 hours. It has been challenging for her to maintain a consistent sleep routine for greater than 2-3 days due to excessive daytime sleepiness requiring naps, although she has been able to function normally at nighttime. She has previously been evaluated by several doctors with trials of multiple stimulants without significant improvement, and currently remains off all stimulants or sedatives. She has previously tried to keep a stable schedule, but with significant difficulty.

Figure 1: Sleep diary.
Patient's prior sleep work up involved multiple sleep latency test (MSLT) (Figure 2) and polysomnogram (PSG) (Table 1), after which she was diagnosed with idiopathic hypersomnia. She has been treated with methylphenidate, amphetamine, and combination of lisdexamfetamine and methylphenidate, prescribed by her psychiatrist for excessive sleepiness. However, none of these medications helped. She was subsequently started on modafinil, which was initially helpful but the effects did not persist causing patient to fall asleep during all odd hours at the maximum dose (300mg).
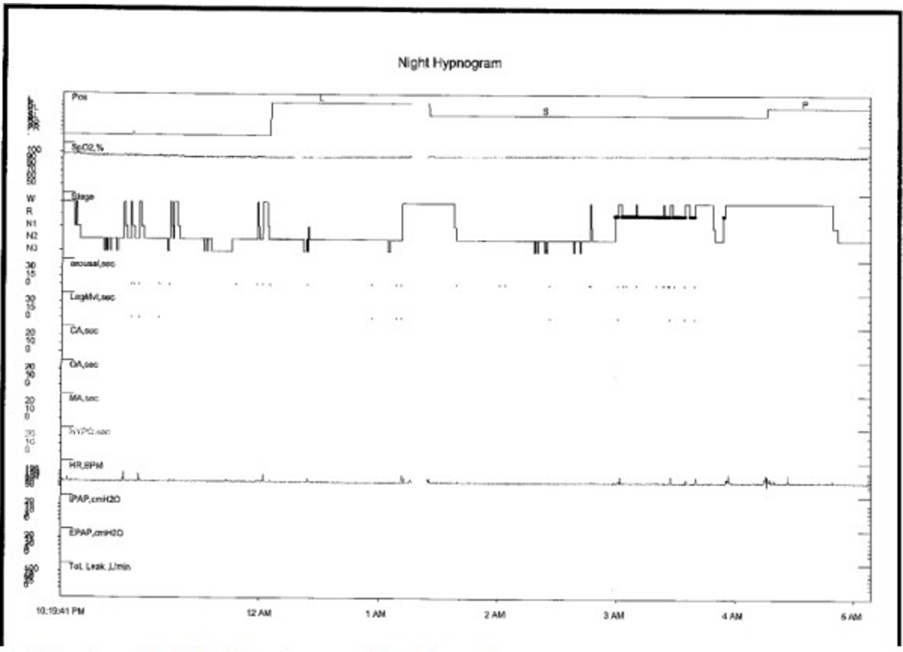
Figure 2: Previous Multiple Sleep Latency Test 6 months ago.
On presentation to the clinic, the patient's STOP-BANG [3] [The snoring, tiredness, observed apnea, high BP, BMI, age, neck circumference, and male gender (STOP-Bang)] score was 1/8, and Epworth sleepiness scale (ESS) [4] was 21/24. Her initial physical exam showed thin, well appearing, with Mallampati Il, no macroglossia or retrognathia. Heart and lung exam were unremarkable and she had flat affect. Body mass index (BMI) was 22.3kg/m2 and blood pressure was 112/76, heart rate 89.
Prior PSG showed no Obstructive Sleep Apnea (OSA)/ periodic limb movement disorder (PLMD), total sleep time 295.7 min, MSLT: fell asleep in 3 out of 5 naps; no sleep-onset REM period (SOREMP)s; mean sleep onset latency (SOL)=13min. PSG showed Respiratory Disturbance Index (RDI) 0/hour, minimum sat 92%, 0 Periodic Limb Movement (PLM)s, arousal index 6.7/hour with some spontaneous leg movements. Wake after sleep onset (WASO) 107 minutes (Table 1).
Table 1: Initial MSLT and PSG results.

Patient was advised to keep a sleep diary and was offered Cognitive behavioural therapy for insomnia (CBT-I) to achieve a regular sleep schedule. However, patient failed the trial of standardized schedule and found it stressful. Her bedtime advanced and cycled through a 24-hour period according to her sleep diary. She feels fine when she follows her rotating sleep schedule. Her ESS improved to 4/24.
Patient tried melatonin and light therapy to be taken same time daily for a short period of time without much of success. She continued to feel sleepy and fatigued when she tried a fixed sleep schedule, and inevitably shifted back to shifting sleep-wake schedule. She felt well with her regular shifting circadian schedule with 7-8 hour of sleep on average, however wished to be able to keep consistent schedule to be able to keep her job and engage in social activities. Due to lack of improvement on melatonin and light therapy, she was prescribed with a trial of tasimelteon 20mg to be taken 30minutes before sleep desired sleep time and to keep a sleep diary. Unfortunately, patient was not able to obtain tasimelteon due to insurance issue, however her sleep time is becoming towards more stabilized between 11pm -1 am to 10am-11am with increased bright light exposure during the daytime and using melatonin at night time.
Discussion
Non-24-hour sleep-wake disorder, also known as free running disorder, is a circadian rhythm sleep disorder when a patient's endogenous circadian rhythm cycles fail to synchronize to a 24-hour day. It was first found in, and is common in, blind individuals without light perception and it is relatively rare in sighted individuals [5]. In mammals, the circadian rhythm is regulated by the suprachiasmatic nucleus ((SCN)) of the hypothalamus. It receives direct input from the retina, which detect and signal light to the central nervous system [6].
The rods and cones that function as photoreceptors in the eyes relay light to our central neural system, by which they play a role in circadian photoentrainment. Also, there is a group of photosensitive, specialized retinal ganglion cells distributed throughout the retina with similar function, projecting to the SCN, and contain melanopsin as their photopigment [7][8]. The light regulates our sleep-wake cycle via sequential nerve conduction to the central circadian pacemaker, and in blind patients, whose light reception is disrupted, the prevalence of N24SWD is much higher.
In a case series published by Emens et al., an intact internal central circadian pacemaker and circadian photoreception (proved by a positive melatonin suppression test) was observed in a sighted patient with N24SWD. And it indicates that the behavioral and environmental factors, such as daily light exposure pattern and sleep-wake timing, might contribute to the dysynchrony between a normal central circadian pacemaker with a non-24-hour sleep-wake pattern, leading to the phenotype of N24SWD in those sighted patients [24].
It is not uncommon to see altered circadian rhythms in patients with psychiatric disorders, although the mechanism between circadian rhythm disruption and psychopathology remains unclear. Rodent studies have shown that the disruption of circadian rhythms can cause affective changes [9]. There were also studies showing abnormal melatonin production/ levels in patients with schizophrenia, major depressive disorder and bipolar disease [10].
In our case, patient has concurrent bipolar disorder, which is well controlled with lamotrigine, bupropion and psychiatric counselling. It's noted that circadian rhythm dysfunction may be a trait marker of bipolar disease in mood disorders [15,16].
Studies have also has shown that irregularity of the social zeitgeber (an external or environmental cue that entrains or synchronizes an organism's biological rhythms with the natural environmental light/dark cycles) can trigger the first onset of mood episode [17]. And interestingly, the wake therapy which involves sleep deprivation was found to be antidepressant [18]. And exogenous melatonin has been shown to have antidepressant effects proved in many studies [19]. Although the causal effects remain unclear, the interaction between circadian rhythm disorder and psychiatric diseases are likely bidirectional.
Medications such as fluvoxamine, flupentixol, and haloperidol were also found to have a potential role in causing iatrogenic circadian rhythm sleep disorders [20-22], although our patient is on none of these medications. It is important to be cautious with the use of these medications if possible while evaluating and treating circadian rhythm sleep disorders. Our patient is started on a trial of Tasimelteon, which has some evidence of entraining totally blind people with N24SWD, and the clinical response is to be followed [23].
Patients with a suspected circadian rhythm sleep disorder should be advised to use of a sleep log or diary-the diagnosis requires at least 14 days of documentation of progressively shifting sleep-wake times with sleep diaries and/or actigraphy. Actigraphy is also indicated for evaluation. Meanwhile, polysomnography is indicated to rule out other potential sleep disorders. It is noted that circadian phase markers such as melatonin can be a useful tool when determining the circadian phase and also confirm the diagnosis. The evidence behind the Morningness-Eveningness Questionnaire (MEQ) [11] is insufficient.
According to 2015 American Academy of Sleep Medicine (AASM) guidelines, timed oral melatonin agonists have a weak recommendation in blind adults but no recommendation in sighted patients. There is no recommendation for other treatment including prescribed sleep-wake scheduling, light therapy, sleep-promoting medications and wakefulness-promoting medications [12].
Yet, timed light exposure, exogenous melatonin or the combination of both are suggested to be probably useful in sighted patients [13]. There are also cases in which patients achieved successful phase advancement with the use of timed melatonin (the most commonly used dose was 3 mg) [14]. Notably in patients with circadian rhythm disorder who have concurrent bipolar disorder, social rhythm therapy such as interpersonal and social rhythm therapy (IPSRT) which aims to address medication noncompliance, social rhythm dysfunction, and stressful experiences, has been shown to improve stabilizing social rhythms and daily routines, as well as occupational functioning [25].
Conclusion
Non-24-hour sleep-wake rhythm disorder is a relatively rare disease in sighted individuals. Currently bright light therapy and scheduled melatonin remain the most effective treatment. There is some evidence indicating that circadian rhythm sleep disorders may predispose patients to personality disorders, and it may be a manifestation of the iatrogenic effect of certain medications. Psychosocial interventions that target stabilizing the daily rhythms as part of the psychotherapy in patients with concurrent psychiatric illness can be helpful.
Declarations:
Statement: All authors have seen and approved this manuscript. No financial disclosure for all the authors listed above. Patient consent was obtained in person.
Ethical Approval: No ethical approval/ IRB approval required for this case report
Availability of data and materials: Data including prior sleep study result and sleep diary can be accessed on patient's electronic medical records.
Authors' contributions: Xinhang Tu drafted the main manuscript and created the table, Victor Peng and Jennifer So obtained figures and all authors revised, modified and finalized the manuscript. All authors reviewed the manuscript.
Funding: No fundings involved in this case report
Conflict of interest: None
References
- Quera Salva MA, Hartley S, Léger D, Dauvilliers YA. Non-24-Hour Sleep-Wake Rhythm Disorder in the Totally Blind: Diagnosis and Management. Front Neurol. 2017:8:686. Published 2017 Dec 18. doi:10.3389/fneur.2017.00686
- Flynn-Evans EE, Tabandeh H, Skene DJ, Lockley SW. Circadian Rhythm Disorders and Melatonin Production in 127 Blind Women with and without Light Perception. J Biol Rhythms. 2014 Jun;29(3):215-224. doi: 10.1177/0748730414536852. Epub 2014 Jun 10. PMID: 24916394.
- Chung F, Abdullah HR, Liao P. STOP-Bang Questionnaire: A Practical Approach to Screen for Obstructive Sleep Apnea. Chest. 2016 Mar;149(3):631-8. doi: 10.1378/chest.15-0903. Epub 2016 Jan 12. PMID: 26378880.
- Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep, 1991; 14: 50-55.
- Uchiyama M, Lockley SW. Non-24-Hour Sleep-Wake Rhythm Disorder in Sighted and Blind Patients. Sleep Med Clin. 2015 Dec;10(4):495-516. doi: 10.1016/j.jsmc.2015.07.006. PMID: 26568125.
- Duffy JF, Czeisler CA. Effect of Light on Human Circadian Physiology. Sleep Med Clin. 2009;4(2):165-177. doi: 10.1016/j.jsmc.2009.01.004
- Victoria L. Revell & Debra J. Skene (2007) Light-Induced Melatonin Suppression in Humans with Polychromatic and Monochromatic Light, Chronobiology International, 24:6, 1125-1137, DOI: 10.1080/07420520701800652
- Reddy S, Reddy V, Sharma S. Physiology, Circadian Rhythm. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-Available from: https://www.ncbi.nlm.nih.gov/books/NBK519507/
- Walker, W.H., Walton, J.C., DeVries, A.C. et al. Circadian rhythm disruption and mental health. Transl Psychiatry 10, 28 (2020). https://doi.org/10.1038/s41398-020-0694-0
- Asarnow LD, Soehner AM, Harvey AG. Circadian rhythms and psychiatric illness. Curr Opin Psychiatry. 2013;26(6):566-571. doi:10.1097/YCO.0b013e328365a2fa
- Horne JA, Östberg O. (1976). A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms". Int J Chronobiol 4 (2): 97-110.
- pii: jc-00358-15 http://dx.doi.org/10.5664/jcsm.5100 Clinical Practice Guideline for the Treatment of Intrinsic Circadian Rhythm Sleep-Wake Disorders: Advanced Sleep Wake Phase Disorder (ASWPD), Delayed Sleep-Wake Phase Disorder (DSWPD), Non-24-Hour Sleep-Wake Rhythm Disorder (N24SWD), and Irregular Sleep-Wake Rhythm Disorder (ISWRD). An Update for 2015, Journal of Clinical Sleep Medicine
- Diagnostic and Treatment Challenges of Sighted Non-24-Hour Sleep-Wake Disorder. Roneil G. Malkani, MD, MS, Sabra M. Abbott, MD, PhD, Kathryn J. Reid, PhD, and Phyllis C. Zee, MD, PhD
- Morgenthaler TI, Lee-Chiong T, Alessi C, Friedman L, Aurora RN, Boehlecke B, Brown T, Chesson AL Jr, Kapur V, Maganti R, Owens J, Pancer J, Swick TJ, Zak R; Standards of Practice Committee of the American Academy of Sleep Medicine. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep. 2007 Nov;30(11):1445-59. doi: 10.1093/sleep/30.11.1445. Erratum in: Sleep. 2008 Jul 1;31(7): table of contents. PMID: 18041479; PMCID: PMC2082098.
- Takaesu, Y. (2018), Circadian rhythm in bipolar disorder: A review of the literature. Psychiatry Clin. Neurosci., 72: 673-682. https://doi.org/10.1111/pcn.12688
- Gold AK, Kinrys G. Treating Circadian Rhythm Disruption in Bipolar Disorder. Curr Psychiatry Rep. 2019;21(3):14. Published 2019 Mar 2. doi:10.1007/s11920-019-1001-8
- Alloy LB, Boland EM, Ng TH, Whitehouse WG, Abramson LY. Low social rhythm regularity predicts first onset of bipolar spectrum disorders among at-risk individuals with reward hypersensitivity. J Abnorm Psychol. 2015 Nov;124(4):944-952. doi: 10.1037/abn0000107. PMID: 26595474; PMCID: PMC4662076.
- Wirz-Justice A, Benedetti F, Berger M, Lam RW, Martiny K, Terman M, Wu JC. Chronotherapeutics (light and wake therapy) in affective disorders. Psychol Med, 2005; 35(7): 939-944. doi: 10.1017/s003329170500437x. PMID: 16045060.
- Ye-qing Wang, Ya-jie Jiang, Man-shu Zou, Jian Liu, Hong-qing Zhao, Yu-hong Wang. Antidepressant actions of melatonin and melatonin receptor agonist: Focus on pathophysiology and treatment, Behavioural Brain Research, Volume 420, 2022, 113724, ISSN 0166-4328, https://doi.org/10.1016/j.bbr.2021.113724.(https://www.sciencedirect.com/science/article/pii/S0166432821006124)
- Wirz-Justice A, Haug HJ, Cajochen C. Disturbed circadian rest-activity cycles in schizophrenia patients: an effect of drugs? Schizophr Bull. 2001;27(3):497-502. doi: 10.1093/oxfordjournals.schbul.a006890. PMID: 11596850.
- Hermesh H, Lemberg H, Abadi J, Dagan Y. Circadian rhythm sleep disorders as a possible side effect of fluvoxamine. CNS Spectr. 2001 Jun;6(6):511-3. doi: 10.1017/s1092852900008051. PMID: 15744215.
- Dagan Y, Borodkin K. Behavioral and psychiatric consequences of sleep-wake schedule disorders. Dialogues Clin Neurosci. 2005;7(4):357-365. doi:10.31887/DCNS.2005.7.4/ydagan
- Lockley SW, Dressman MA, Licamele L, Xiao C, Fisher DM, Flynn-Evans EE, Hull JT, Torres R, Lavedan C, Polymeropoulos MH. Tasimelteon for non-24-hour sleep-wake disorder in totally blind people (SET and RESET): two multicentre, randomised, double-masked, placebo-controlled phase 3 trials. Lancet. 2015 Oct 31;386(10005):1754-64. doi: 10.1016/S0140-6736(15)60031-9. Epub 2015 Aug 4. PMID: 26466871.
- Emens JS, St Hilaire MA, Klerman EB, Brotman DJ, Lin AL, Lewy AJ, Czeisler CA. Behaviorally and environmentally induced non-24-hour sleep-wake rhythm disorder in sighted patients. J Clin Sleep Med. 2022 Feb 1;18(2):453-459. doi: 10.5664/jcsm.9612. PMID: 34402783; PMCID: PMC8805008.
- Frank E, Soreca I, Swartz HA, Fagiolini AM, Mallinger AG, Thase ME, Grochocinski VJ, Houck PR, Kupfer DJ. The role of interpersonal and social rhythm therapy in improving occupational functioning in patients with bipolar I disorder. Am J Psychiatry. 2008 Dec;165(12):1559-65. doi: 10.1176/appi.ajp.2008.07121953. Epub 2008 Oct 1. PMID: 18829872; PMCID: PMC3308335.

