A Case Report on Successfully Treated Breakthrough Invasive Fungal Sinusitis with Oral Posaconazole in an Uncontrolled Type 2 Diabetes Mellitus Patient
Ambily Sahadevan1,* and Kailash Prasad Verma2
1ADMO, Department of ENT, Central Hospital, South Eastern Railway, Kolkata, West Bengal, India
2Sr.DMO (SG) and HOD, Department of ENT,Central Hospital, South Eastern Railway, Kolkata, West Bengal, India
Received Date: 04/07/2023; Published Date: 22/11/2023
*Corresponding author: Dr. Ambily Sahadevan, MBBS, DNB(ENT), Fellowship in Rhinology (Graz)ADMO, Department of ENT Central Hospital, Garden Reach, South Eastern Railway, Kolkata, West Bengal, India, Pin code: 700043
Abstract
Here we describe a case of Mucormycosis in an uncontrolled type 2 diabetes mellitus patient that was managed by surgical debridement, strict control of blood sugars and liposomal amphotericin B with a breakthrough infection of the same organism after 3 weeks of treatment. It was treated successfully by the newer triazole Posaconazole on an Outpatient Department (OPD) basis. The advantages of Posaconazole were its it’s oral route of administration, high efficacy and minimal side effects. It avoids hospital admission and helps in mental well-being. After a follow up of 5 months, there was no recurrence. Even though Posaconazole is used as a step-down therapy after amphotericin B, no other cases of breakthrough invasive fungal infection treated with oral Posaconazole have been reported in the literature. Even though amphotericin B is the gold standard, this report highlights the need for second line antifungals in the armamentarium for management of breakthrough invasive fungal sinusitis.
Introduction
Invasive fungal sinusitis is a life-threatening disease which is rare in immunocompetent individuals. The common fungal organisms causing invasive fungal sinusitis comes from Aspergillus species and Zygomycetes order [1]. Zygomycetes order contains Mucorales. During the covid era, there was a surge in the incidence of Mucormycosis, that it led to the new terminology COVID 19 associated Mucormycosis or CAM [2]. Here we report a case of breakthrough Mucormycosis in an uncontrolled type 2 diabetes mellitus patient that was managed by the newer triazole Posaconazole on an OPD basis.
Case Report
A 55year-old male with uncontrolled diabetes mellitus presented with bilateral progressive nose block, anosmia, epistaxis and swelling over the left side of face of one month duration. There was a foul-smelling discharge from the left nostril. He was on treatment elsewhere and the recent onset of nasal regurgitation of food prompted his visit to our OPD. There was no history of covid 19 infection or any other comorbidities.
On examination there was obvious asymmetry of the face with prominence of the left side of cheek. There was reduced sensation over the left nostril. On anterior rhinoscopy, the entire left nostril was filled with bloodstained debris. Endoscopic examination revealed necrosed left inferior turbinate and anterior part of left middle turbinate with eroded medial wall of left maxillary sinuses. There was an oro-nasal fistula and there was no involvement of nasal septum.
Due to the absence of pain, on suctioning, the majority of the necrosed bone including the inferior turbinate was removed in the OPD setup itself (Figure 1).
A provisional diagnosis of invasive fungal sinusitis was made and the debris was sent for fungal staining and culture. Strict control of blood sugars was achieved. Empirically liposomal amphotericin B was started at an initial dose of 1 mg/kg body weight per day and escalated to 3 mg/kg/day. Microbiological examination showed presence of nonstate ribbon-like hyphae suggestive of Mucormycosis.
Ct nose and Paranasal sinuses revealed involvement of entire left sided sinuses. It was abutting the left orbit without breach of lamina papyracea. All walls of the left maxillary sinus were involved with nasal floor erosion. MRI showed the oronasal fistula and confirmed absence of orbital and intracranial involvement (Figure 2).
Patient was taken up for surgical debridement. For better precision navigation assisted image guided endoscopic surgery was done. Modified Denker's approach was used and the floor of the left maxillary antrum was flushed with the nasal floor. Complete surgical clearance of the disease was attained. Debridement was done till healthy bleeding tissue was reached. The repair of the oro-nasal fistula was planned as a second stage surgery. Histopathological examination confirmed Mucormycosis (Figure 3).
Liposomal amphotericin B which was started earlier continued at a dose of 3 mg /kg body weight. Regular monitoring of renal function and other blood tests were done. Patient was started with saline nasal irrigation and weekly endoscopic suctioning.
After 3 weeks of intravenous liposomal amphotericin B, he developed a small whitish necrotic area near the anterior end of the nasal septum on the left side (Figure 4).
A punch biopsy of the doubtful area was taken and histopathology revealed Mucormycosis. This breakthrough infection prompted the use of second line antifungal therapy. We started with oral Posaconazole at a dose of 200 mg twice daily. The patient was clinically stable and discharged on oral Posaconazole. He reviewed every two weeks and after one month the cavity was cleared without any evidence of any recurrent disease. He continued the Posaconazole for another couple of weeks and then the drug was stopped. Now 5 months have been completed and he is in good condition. There is no asymmetry of face (Figure 5) and nasal endoscopy showed complete clearance without any fungal disease (Figure 6).
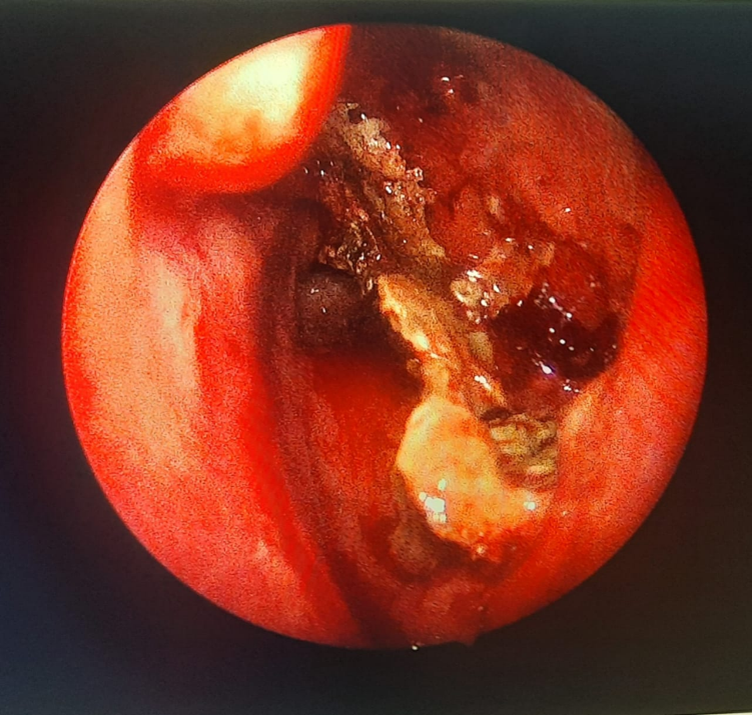
Figure 1: Endoscopic picture after removal of necrotic bone from left nasal cavity.

Figure 2: MRI showing left oronasal fistula.

Figure 3: Microscopic picture of mucormycosis.

Figure 4: Endoscopic image showing necrotic area near the anterior end of left side of nasal septum.
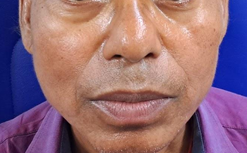
Figure5: Figure showing the symmetry of face.
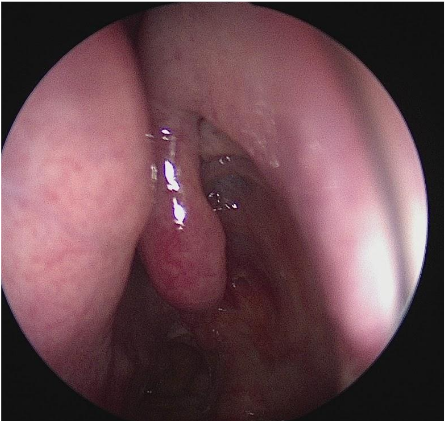
Figure 6: Endoscopic image on follow up showing complete clearance of the disease.
Discussion
Invasive fungal sinus disease is defined as the presence of fungal hyphae within the mucosa, submucosa, bone or blood vessels on histopathology [3]. The cornerstone in management of invasive fungal sinusitis are control of comorbidities, surgical debridement and intravenous antifungals. The significance of the disease is its high morbidity and mortality of about 50% [4].
The surgical debridement was initially considered as debulking of the disease and reducing the fungal load, but complete clearance of the disease has better prognosis. Also, there are case reports of invasive Mucormycosis which was completely cured with intravenous antifungals alone without any surgical debridement [5,6]. But here in this case, in spite of the complete surgical clearance and intravenous amphotericin B there was a breakthrough Mucormycosis infection.
Breakthrough Invasive Fungal Infection (IFI) was defined as any invasive fungal infection occurring during exposure to an antifungal drug, including fungi outside the spectrum of activity of an antifungal [7]. The time of breakthrough IFI was defined as the first attributable clinical sign or symptom, mycological finding or radiological feature [7]. Usually, it occurs in immunocompromised individuals in association with voriconazole therapy [8,9]. Victoria et al have reported a risk of breakthrough IFI in patients with haematological malignancies receiving Venetoclax plus Voriconazole [10]. Breakthrough (IFI)in association with liposomal amphotericin B is not reported in the literature, when on treatment with intravenous liposomal amphotericin B.
As per the expert view point by Slavin et al a change of drug is indicated in invasive fungal disease when a new clearly distinct site of infection is detected [11]. Moreover, there were clear advantages of Posaconazole over the Liposomal amphotericin B, which includes its oral route, high efficacy [12] and minimal side effects [13]. It doesn’t require regular blood tests and hospital admission. But one concern is regarding its bioavailability, as it is only 8 to 47% [14]. But it can be improved with a high fat diet.
Despite its toxic potential, Amphotericin B remains useful due to its broad spectrum of activity, low resistance rate and excellent clinical and pharmacological action [15]. Its lipid associated formulation liposomal amphotericin b is more commonly used, as it has a lower incidence of infusion-related adverse events and nephrotoxicity than conventional amphotericin B [16]. The other oral antifungal agents used in management of invasive fungal sinusitis are Isavuconazole and Itraconazole. Complete cure of the disease needs prolonged treatment that may take many months.
Conclusion
Here we highlight the need for prolonged antifungal therapy and the need for second line antifungals in the armamentarium for management of breakthrough invasive fungal sinusitis.
Authorship: First is responsible for concept and acquisition of data and drafting the article(guarantor). The second author is the main surgeon and have done the interpretation and revision of the article.
Conflict of interest: Authors declare no conflict of interest
Acknowledgements: Authors would like to acknowledge Dr. Mahamaya Sharma ACHD/Pathology and Dr.Ratan Prabha Dhanwar Sr.DMO/Microbiology Central Hospital, South Eastern Railway.
Grant Information: Authors received no specific funding for the work.
References
- Deutsch PG, Whittaker J, Prasad S. Invasive and Non-Invasive Fungal Rhinosinusitis-A Review and Update of the Evidence. Medicina (Kaunas), 2019; 55(7): 319. doi: 10.3390/medicina55070319.
- Pal R, Singh B, Bhadada SK, Banerjee M, Bhogal RS, Hage N, et al. COVID-19-associated mucormycosis: An updated systematic review of literature. Mycoses, 2021; 64(12): 1452-1459. doi: 10.1111/myc.13338.
- deShazo RD, O'Brien M, Chapin K, Soto-Aguilar M, Swain R, Lyons M, et al. Criteria for the diagnosis of sinus mycetoma. J Allergy Clin Immunol, 1997; 99(4): 475-485. doi: 10.1016/s0091-6749(97)70073-3. PMID: 9111491.
- Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis, 2005; 41(5): 634-653. doi: 10.1086/432579.
- Gollard R, Rabb C, Larsen R, Chandrasoma P. Isolated cerebral mucormycosis: case report and therapeutic considerations. Neurosurgery, 1994; 34(1): 174-177. doi: 10.1097/00006123-199401000-00026.
- Elzein F, Kalam K, Mohammed N, Elzein A, Alotaibi FZ, Khan M, et al. Treatment of cerebral mucormycosis with drug therapy alone: A case report. Med Mycol Case Rep, 2018; 23: 4-7. doi: 10.1016/j.mmcr.2018.10.005.
- Cornely OA, Hoenigl M, Lass-Flörl C, Chen SC, Kontoyiannis DP, Morrissey CO, et al. Mycoses Study Group Education and Research Consortium (MSG-ERC) and the European Confederation of Medical Mycology (ECMM). Defining breakthrough invasive fungal infection-Position paper of the mycoses study group education and research consortium and the European Confederation of Medical Mycology. Mycoses, 2019; 62(9): 716-729. doi: 10.1111/myc.12960.
- Kim SB, Cho SY, Lee DG, Choi JK, Lee HJ, Kim SH, et al. Breakthrough invasive fungal diseases during voriconazole treatment for aspergillosis: A 5-year retrospective cohort study. Med Mycol, 2017; 55(3): 237-245. doi: 10.1093/mmy/myw067.
- Trifilio S, Bennett C, Yarnold P, et al. Breakthrough zygomycosis after voriconazole administration among patients with hematologic malignancies who receive hematopoietic stem-cell transplants or intensive chemotherapy. Bone Marrow Transplant, 2007; 39: 425–429. https://doi.org/10.1038/sj.bmt.1705614
- Victoria G Hall, Kenny Tang, Deepali Kumar, Coleman Rotstein, Signy Chow, Steven M Chan, et al. Breakthrough Invasive Fungal Infection After Coadministration of Venetoclax and Voriconazole, Open Forum Infectious Diseases, 2023; 10(3): ofad134, https://doi.org/10.1093/ofid/ofad134
- Monica A Slavin, Yee-Chun Chen, Catherine Cordonnier, Oliver A Cornely, Manuel Cuenca-Estrella, J Peter Donnelly, et al. When to change treatment of acute invasive aspergillosis: an expert viewpoint, Journal of Antimicrobial Chemotherapy, 2022; 77(1): Pages 16–23, https://doi.org/10.1093/jac/dkab317
- Wong TY, Loo YS, Veettil SK, Wong PS, Divya G, Ching SM, et al. Efficacy and safety of posaconazole for the prevention of invasive fungal infections in immunocompromised patients: a systematic review with meta-analysis and trial sequential analysis. Sci Rep. 2020; 10(1): 14575. doi: 10.1038/s41598-020-71571-0.
- Leung S, Poulakos MN, Machin J. Posaconazole: An Update of Its Clinical Use. Pharmacy (Basel), 2015; 3(4): 210-268. doi: 10.3390/pharmacy3040210.
- Lipp HP. Clinical pharmacodynamics and pharmacokinetics of the antifungal extended-spectrum triazole posaconazole: an overview. Br J Clin Pharmacol, 2010; 70(4): 471-480. doi: 10.1111/j.1365-2125.2010.03680.x.
- Cavassin FB, Baú-Carneiro JL, Vilas-Boas RR, et al. Sixty years of Amphotericin B: An Overview of the Main Antifungal Agent Used to Treat Invasive Fungal Infections. Infect Dis Ther, 2021; 10: 115–147. https://doi.org/10.1007/s40121-020-00382-7
- Moen MD, Lyseng-Williamson KA, Scott LJ. Liposomal amphotericin B: a review of its use as empirical therapy in febrile neutropenia and in the treatment of invasive fungal infections. Drugs, 2009; 69(3): 361-392. doi: 10.2165/00003495-200969030-00010.

