Strategy for the Management of Ischemic Heart Disease in the Elderly Subject: Study of a Series Of 42 Cases and Review of the Literature
Salma Sayarh*
Vascular surgery and cardiology departments of Ibn Sina Hospital, University Mohamed V, Morocco
Received Date: 03/07/2023; Published Date: 20/11/2023
*Corresponding author: Salma Sayarh, Vascular surgery and cardiology departments of Ibn Sina Hospital, University Mohamed V, Morocco
Introduction
With the continuous increase in life expectancy at birth, the proportion of elderly people, exceeding 70 years, has increased significantly.
As a result, the management of patients over the age of 70 has now become frequent in our cardiology units.
The objective of this study is to highlight the particularity of the coronary proCil of elderly coronary patients, as well as the therapeutic strategy to be undertaken.
Materials and Methods
We therefore conducted a retrospective observational study lasting one year, and collected during this study period, 42 patients with an age greater than or equal to 70 years.
Results
1. Socio-demographic data and risk factors of the study population:
Table 1: Socio-demographic data and risk factors of the study population.

-The median age of patients was 75± 2 years (range: 70 to 90 years) with female predominance (54.8 %).
-The most common cardiovascular risk factor was high blood pressure with a percentage of (76.2%), followed by dyslipidemia (38%), diabetes (33.3%) and tobacco (26.1%).

-(28.5%) of our patients had previously had angioplasty, (2.4%) coronary aorto bypass graft, (26.2%) had a history of infarction and enCin (4.7%) had a stroke.
2. Indications:
Table 2: Indications for coronary angiography (n=42).
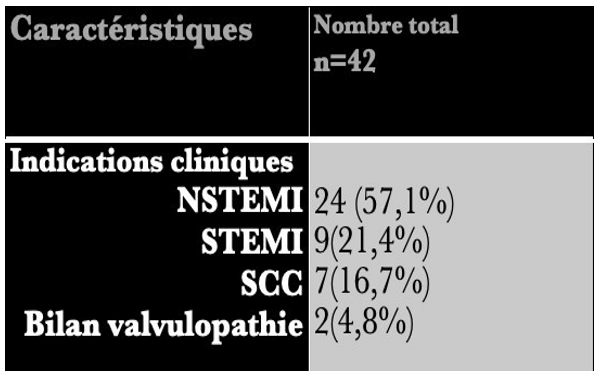
- The main indication was ACS with (57.1%) of patients admitted for the management of ACS without ST segment elevation, (21.4%) of patients were admitted for ST segment elevation infarction ( ST+ MI),(16.7%) explored in the context of chronic coronary syndrome and enCin (4.8%) of patients received coronary angiography as part of the preoperative assessment of valvular heart disease.
3. Materials and procedures:
Table 3: Description of the procedure (n=42).
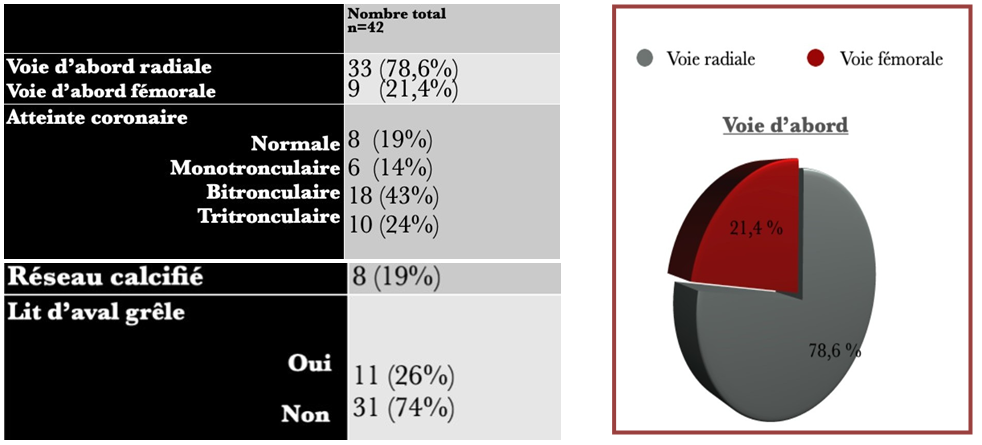
- (78,6%) Procedures were performed radially (33/42), 9 were performed femorally. Of the 33 procedures performed by radial, (25 were performed by right radial, and 8 by left Arterial puncture or tube progression failure with the need for pathway conversion first was noted for 3 procedures.
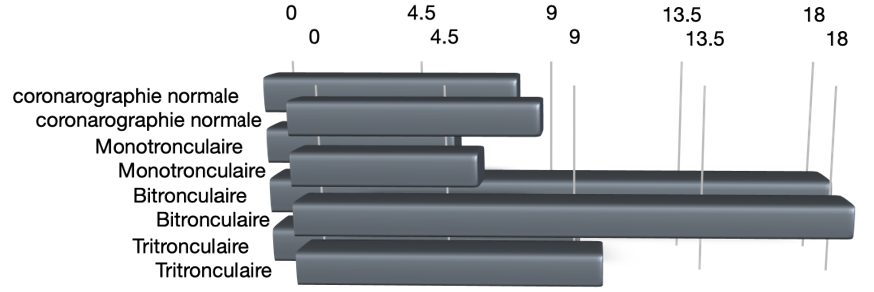
- Of the 42 coronary angiograms performed, 8 were normal (19%).
*34 of our patients were coronary, of which 28 were multi-truncal (67%) divided into (43%)bitruncal and (24%)tritruncal .
* Only 14% were monotruncular.
Number of patients
- Of all coronary angiography performed, (19%) of the coronary networks were calciciated, and in (26%) of cases the downstream bed was hail.

Figure 1: Coronary network of the elderly.

Figure 2: InGiltated and diffuse coronary network of the elderly.
4. Score Syntax et stratégie thérapeutique:
Table 4: Syntax score in multitruncal patients (n=28).
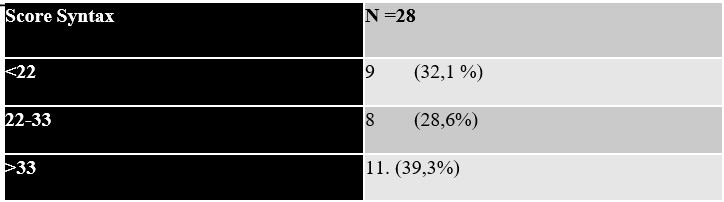
- The syntax score was calculated in our 28 multi-truncal patients, and therefore (39.3%) had a high syntax score above 33, (28.6%) had an intermediate score between 22 and 33 and enCin, (32.1%) had a low syntax score <22.
Table 5: Therapeutic strategy in coronary patients (n=34).
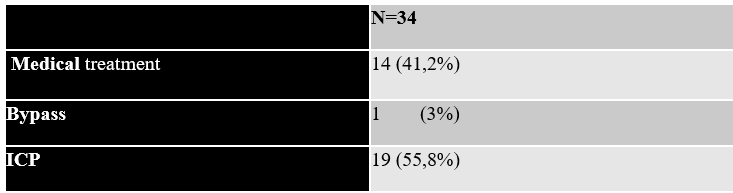
- Aa the outcome of coronary angiography, of our 34 patients confirmed coronary, only 19 benefited from coronary angioplasty (55.8%), only one patient benefited from coronary aorto bypass graft (3%), and 14 patients in our series (41.2 %) received medical treatment.
5. Angioplasty equipment and complications s in hospital:
Table 6: Description of coronary angioplasty(n=19)

- Our angioplasty procedures were mostly performed by EBU probes concerning the left network with a percentage of (63.1%) while for the right network RJ was the most used probe, a JL only and an AL were used on our 19 angioplasties.
- (79%) hydrophobic guides were used and (21%) hydrophilic guides.
- FFR was performed in 5 patients in our series, a percentage of (26.3%).
- Of the 30 implanted stents, (96.7%) were active
- On average 2 balloons were used per procedure, the semi-compliant balloon (51.3%) was used for pre-dilation purposes and the non-compliant balloon (48.7%) was used in some pre-dilation procedures to remove stenosis after failure of the semi-compliant balloon and in post dilation for a better Cinal result after stenting.
- Of our 19 angioplasties, two patients had a highly calciciated network in whom the rotablator was required (10.5%).
- The contrast volume for angioplasty on average was 150 ml [130-205 ml].
Table 7: Cardiac and extra-cardiac complications during the hospital period.

-Cardiac complications were represented by a massive OAP having progressed well after management, 1 cardiogenic shock of fatal evolution having led to death and a refractory VF following a recovery for ATL having now evolved in the same direction .
- Extracardiac complications were represented by ischemic A VC, one case of transient visual nail, and 1 case of transient renal insufcisance of favorable course without dialysis.
- 5 percent died during the hospital period following the interventional act, one coronary artery initially for pre-hospital cardiac arrest, which was complicated by cardiogenic shock in post-procedure and the other hospitalized initially for SCAST-, and resumed on d5 for IDM ST+ complicated by a refractory VF.
Discussion
This study allows us to circumscribe the data of the literature, because indeed the elderly coronary patients of our series present on the whole a severe coronary artery disease with for the most part a pluri truncal (67%), a calciciated coronary network in (19%) of cases, and diffuse involvement in Ciltrée with a small network of the entire coronary tree in (26%) of cases, thus limiting the choice of treatment option.
Comparing us to the study carried out by the NICE University Hospital team (50%) of the patients in their series had multitruncal involvement with a calciciated network in (47.9%) of which (21.6%) tritruncal lesions which is in line with the data of our study with (24%) of tritruncal patients. truncal.
At the end of coronary angiography, we treated in our series 19 patients by coronary angioplasty (55.8%), one patient benefited from coronary aorto bypass surgery, and (41.2%) were medically managed because we found in our series (19%) of calcined coronary disease incinerated and diffuse throughout the network, hasa small downstream bed in (26%) of cases thus limiting the possibility of performing angioplasty and coronary bypass surgery.
This diffuse inciltration can be explained in our series by the frequency of diabetes
(33.3%), which is described in the literature as being associated with diffuse incinerated and multitruncal involvement.
The choice of therapeutic strategy depended in our series on the mode of presentation of coronary artery disease as well as the syntax score. In the series of Kanwar et al and a 2017 study, NSTEMI was the most encountered with respectively (32%) and (39.1%) [46,47], in the FAST MI 2010 register (25%) of patients had a infarction with elevation and 38% an infarction without elevation)
Similar to our study, the main indication was NSTEMI (57.1%).
All our monotruncal patients (14%) benefited from angioplasty, while for multi-truncal patients we guided the therapeutic strategy by the SYNTAX score.
Surgical revascularisation should therefore not be systematically excluded in this population, although angioplasty seems to be a good choice in most cases, in view of the high comorbidities in this population. and also, the improvement of coronary angioplasty equipment allowing complete revascularization [48].
The eleven patients in our series with a high syntax score above 33 should be proposed for surgery but only one diabetic patient according to the recommendations truncal tri benefited from a CABG and we performed an ATL in four of these patients in front of their refusal of surgery and faced with the operative risk which was high, for the other 6 patients we opted for a medical treatment in front of the diffuse inciltration of the coronary network and the bad bed downstream therefore not allowing invasive treatment by either PAC or PCI.
In addition, 19 patients in our series were managed by angioplasty, including 6 monotruncle, 9 multi-truncal with low or intermediate syntax score and 4 multi-truncal with high syntax score.
Two patients with calciciated coronary lesions were treated with rotablator because the calciCications did not yield to non-compliant balloons.
Some procedures have required the use of more than one balloon for both pre-dilation and post-dilation.
In the studies of Parkih et al. [49] and From et al. [50], PKI was reported respectively in (64 %) and (91%) of patients, and in our series in (55.8%) of cases.
The complications of coronary angiography and angioplasty in the elderly are mainly local, hemorrhagic and related to the puncture site. This risk should be well assessed in elderly subjects [51]. The general complications found in our series are also consistent with the data in the literature, these were stroke and renal insufCis [52].
Conclusion
Invasive treatment of myocardial ischemia can be performed via interventional catheterization or surgery. For a long time, these two modes of revascularization were opposed. It will therefore be necessary to clearly mark out the choice between these two possibilities in the best interest of the patient, without forgetting the need for multidisciplinary cardio-surgical care ("Heart team") in order to offer the best therapeutic ace for each patient.
The decision of revascularization in tri-truncal patients must be discussed on a case-by-case basis taking into account, in addition to the anatomical scores (SYNTAX score), and the operative risk via the STS score and Euroscore 2, the comorbidities as well as the overall fragility of each patient (Charlson Index, MMSE, the MNA scale…).
Medical treatment will represent an adequate therapeutic option for the patient in whom the indication for surgery or angioplasty will be limited as much by the fragility of the terrain or by their high operative risk, as by their inCiltré coronary network and the poor quality of their downstream bed.

