Erector Spinae Plane Block in a Case of Right Laparoscopic Surrenalectomy
Giulia Montori1,*, Giuseppa Procida1, Flavio Badii2, Agostino De Venanzi3, Federica Salemi1, Alberto Grassetto2, Giorgio Mazzarolo1, Edelweiss Licitra1, Irene Recchia1 and Ferdinando Agresta1
1General Surgery Dpt, ULSS 2 Marca Trevigiana, Vittorio Veneto Hospital, Vittorio Veneto (TV), Italy
2Anesthesiology Dpt, ULSS 2 Marca Trevigiana, Vittorio Veneto Hospital, Vittorio Veneto (TV), Italy
3Internal Medicine Dpt, ULSS 2 Marca Trevigiana, Vittorio Veneto Hospital, Vittorio Veneto (TV), Italy
Received Date: 15/06/2023; Published Date: 06/11/2023
*Corresponding author: Giulia Montori MD, Unit of General and Emergency Surgery, Vittorio Veneto Hospital. Via C. Forlanini 71, 31029 Vittorio Veneto (TV), Italy
Abstract
Laparoscopic surrenalectomy is now considered a standardized and safe procedure especially for lesions less than 10 cm. However, the patient position during surgery can be uncomfortable and, also in cases of mini-invasive approach, post-operative pain can be present.
A 50-year-old-woman with a large right adrenal mass discovered accidentally with only abdominal discomfort and without clinical signs of hormonal hypersecretion was candidate for a laparoscopic surrenalectomy with Erector Spinae Plane (ESP) block and general anesthesia technique, to decrease significantly postoperative pain.
In this case we aimed to combine the mini-invasive approach in expert hand with the use of ESP block associated with general anesthesia, to decrease post-operative discomfort and pain.
Keywords: Laparoscopic adrenalectomy; Laparoscopic surrenalectomy; Erector Spinae Plane (ESP) Block; Ganglioneuroma
Introduction
Since the first laparoscopic transabdominal adrenalectomy performed in 1992, the efforts to ensure a mini-invasive approach to improve patient’s outcome, decreasing pain and discomfort, achieving better cosmetic results and faster recovery of normal daily activity, are increasing [1].
These efforts have always been directed to the search for an equivalent advantage in terms of safety, with the aim of reaching the same oncological outcomes as in open surgery.
Literature reports that laparoscopic adrenalectomy can be safely performed for masses less than 10 cm, but in expert hand also larger ones may be managed, if oncologic parameters were maintained [2].
This is the first case report combining ESP block with general anesthesia in a laparoscopic surrenalectomy.
In our opinion, the perioperative outcomes in terms of pain and analgesic consumption were very promising.
Case Description
A 50-year-old-woman with abdominal discomfort and sense of wight performed a contrast enhancement CT scan in the suspicion of a gallstone in the gallbladder. The CT showed a right disomogeneous adrenal mass with 76 for 64 mm dimension (Figure 1), without clear cleavage planes with surrounding organs. No venous and arterial anomalies were found, except for a little enhancement in arterial and venous contrast phase with disomogenous enhancement in late phase. No evidence of metastases and only two indefinite liver nodules were found.
After this radiological finding, the patient was referred to the endocrinologist. Any hormonal hypersecretion by dosing 24 hours urinary metanephrine/normetanephrine was excluded and the morning serum cortisol after 1 mg overnight dexamethasone suppression test, was within the normal range. No renin, aldosterone, dehydroepiandrosterone-sulfate (DHEA-S) or testosterone blood sample was collected because the patient was neither hypertensive, nor affected by hirsutism and she reported regular menstrual cycle [3].
After CT scan, an 18 fluorodeoxyglucose positron emission tomography (FDG PET) was performed to evaluate the range of mass activity: no augmented activity was present in adrenal mass, however an increased uptake was evident in a solid uterine mass compatible with uterine myoma (Figure 2).
After a multidisciplinary meeting with endocrinologist, surgeon, radiologist and anesthesiologist, the indication for surgical removal of the mass was given.
Surgical approach was discussed with the patient, and due to our center expertise in laparoscopic approach, even in presence of a non-secretory mass at the higher dimensional limits, laparoscopic approach was suggested. The woman had extensively been informed of the possibility of a conversion to laparotomy.
A general anesthesia associated with Erector Spinae Plane (ESP) block was planned. For the execution of the block the patient was positioned seated and the T7 spinous process was scored; the transducer probe was moved from midline 3 cm lateral to visualize the T7 transverse process and the erector spinae muscle (Figure 3A). A 21 G needle and 50 mm long was inserted, in plane to the transducer, in the cranio-caudal direction until the needle tip has reached the plane fascia between the erector spinae muscle and the transverse process. The needle tip position was checked by hydrodissection with 2 mL of normal saline. Subsequently a total of 20 ml of was injected ropivacaine 0.33% with the addition of 4 mg dexamethasone as adjuvant. The diffusion of the local anesthetic was observed sonographically (Figure 3B). At the same way, the same locking procedure was performed on the other side.
After the ESP block, induction and maintenance of anesthesia with propofol and remifentanil using a Target Controlled Infusion (TCI), using Eleveld algorithm according with bispectral index (BIS) monitoring, was performed. Endotracheal intubation was achieved with rocuronium 50 mg and fentanyl 200 mcg. During surgery continuous monitoring of invasive pressure, through a radial arterial catheter, was associated to routine monitoring of ECG, SpO2, etCO2, and ventilation parameters.
A first 10 mm trocar (Figure 4A) in right subcostal position was insert, along the right midclavicular line, with a direct trocar insertion technique (DTI). Others three 5 mm trocars were insert in epigastric, right flank and right subcostal position. After the mobilization of right colonic angle, the duodenum, and the liver, the right adrenal mass was identified. The mass appeared well capsulated, and no intraoperative infiltration or metastasis were found. The mass detachment was carefully performed with help of the radiofrequency high energy device (Figure 4B-4D). The laparoscopic right surrenalectomy was performed, the mass was removed with a mini-Pfannestiel in the lower abdomen, caching into an endobag, to avoid sealing. Surgical procedure was uneventful and no hemodynamic or ventilatory complications occurred during anesthesia. Before awakening, 30 mg of ketorolac and 1 gram of paracetamol were administered.
There were no early post-operative complications. In the 1nd post-operative day the nasogastric tube was removed and the patient was slowly refed. In 2rd day intestinal gas was performed and the abdominal drain was removed. Postoperative blood samples were normal. Pain control was performed using the Visual Analogue Score (VAS) at 6, 12, 24 and 48 hours. VAS remains 0 for all post-operative hospitalization, except for the 2nd post-operative days in which the patients referred a VAS of 2. In 3rd post-operative day, the woman was discharged.
Hystopathological report showed a ganglioneuroma (11x6x3 cm), a benign tumor, completely removed.
One month later at the follow up no morbidity or late complications were found (no incisional site infection, no residual abdominal pain, oral intake, and the intestinal transit was normal). The patient was satisfied for her complete clinical recovery.
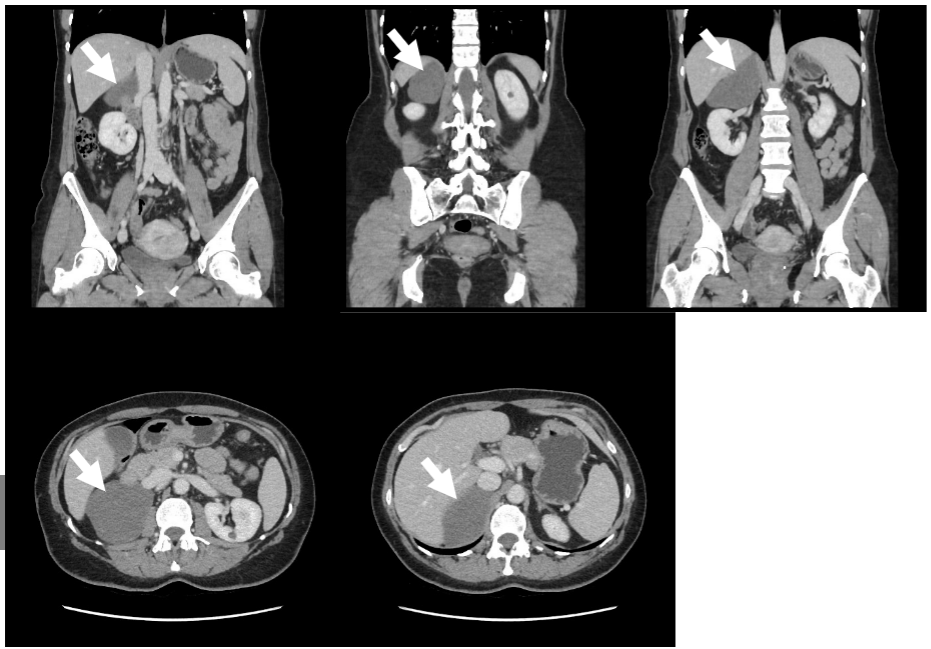
Figure 1: Pre-operative CT scan: CTscan images in sagittal and coronal plane showing the right adrenal mass (white arrow).

Figure 2: Pre-operative PET scan: no mass activity in the right adrenal gland (white arrow).
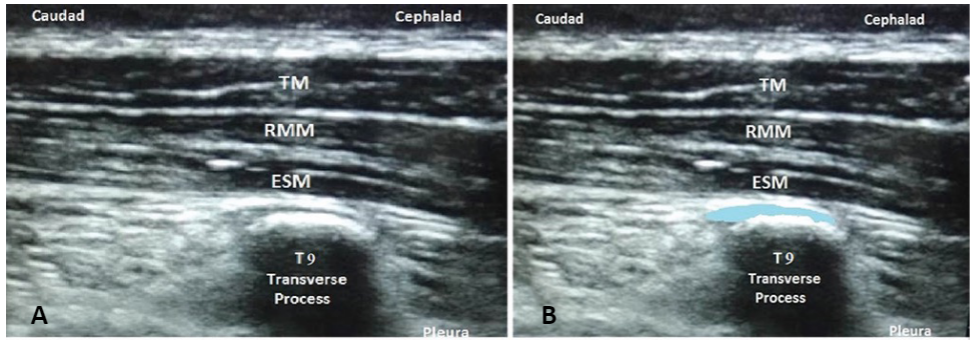
Figure 3: Erector spinae muscles (ESP) block: A. US view of the 7th transversus vertebral process (T7) with the three muscles above (TM: trapezius muscle, RMM: rhomboid major muscle, ESM: Erector spinae muscles). B. Space of the local anesthetic diffusion (blue line).
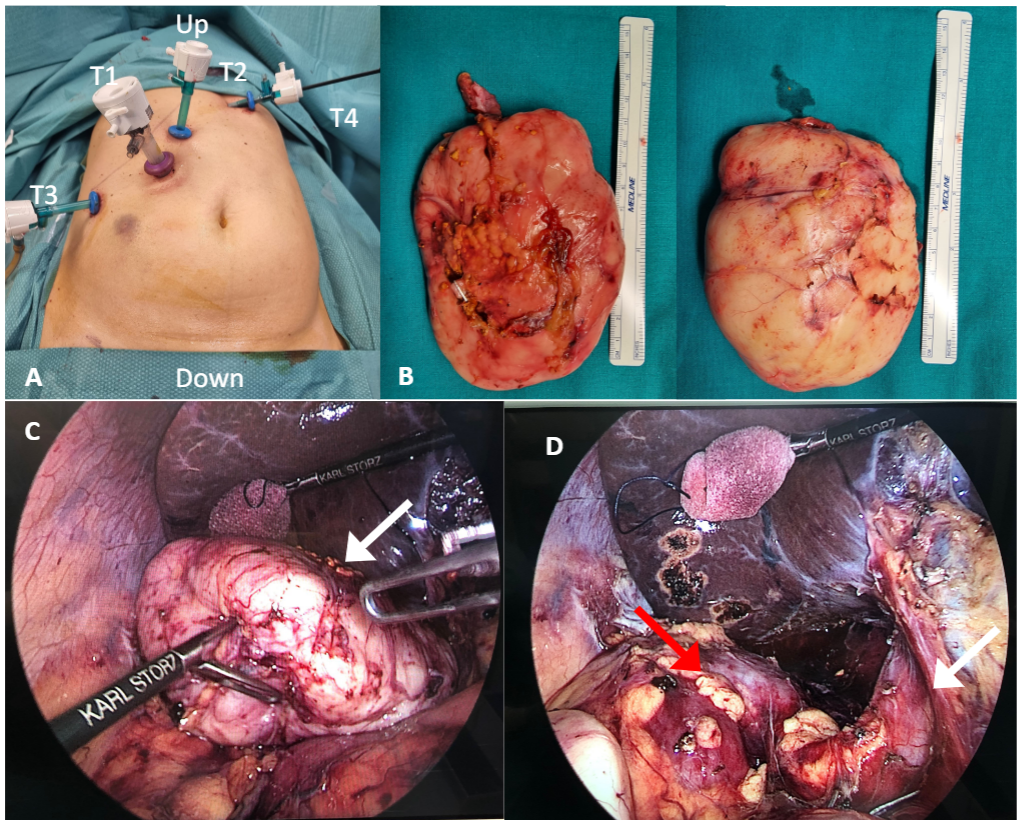
Figure 4: Intraoperative trocar positioning and intraoperative findings:
A. Patient’s operative positioning with the four trocars.
B. Macroscopic vision of the right adrenal mass.
C. Intraoperative view of the right adrenal mass (white arrow) near to the liver (in the upper part) and the right kidney (in the down part).
D. Intraoperative view after gland removal: the vein cave (white arrow) and the right kidney (the red arrow).
Discussion
This case was interesting from many sides. Firstly, the combination of ESP block with the mini-invasive approach allowed to reduce postoperative pain with a complete patient’s satisfaction. Secondly, the role of multidisciplinary team favored the correct timing, the correct indication and the correct approach to this pathology.
The ESP block is an interfascial block which allows for the dispersion of the local anesthetic in the interfascial plane between the process transversus and erector spinae muscles. This block achieves a paravertebral spread of three and four vertebral levels cranially and caudally, respectively, covering the ventral and dorsal rami of spinal cord thus inhibiting both visceral pain than the somatic one.
Ultrasound guided ESP block may be considered as an alternative technique to epidural anesthesia because it provides an effective postoperative analgesic coverage for breast and thoracic surgery when performed at T4-T5 level or for abdominal surgery at T7-T8 level [4]. Althought, epidural anesthesia generally considered a safe technique, it is not free of possible complications: epidural hematoma and postoperative neurologic deficit are rare, but post dural puncture headache is not. Moreover, introduction of enhanced recovery after surgery (ERAS) protocols and a shift from open to laparoscopic surgery have diminished the advantage of epidural anesthesia. In a recent review on this topic, the authors suggested that epidural anesthesia in abdominal surgery has become less preferred and limited to surgical procedures with difficult pain management [16].
In this case we wanted to assess the effectiveness of the ESP block on postoperative pain, with the purpose also of limiting opioid administration and then possibly reducing postoperative nausea and vomiting. We also wanted to observe the response of the patient in terms of satisfaction and postoperative recovery. No analgesics were required in the first 48 hours after surgery, except for 1 g of Paracetamol in 2nd post-operative day. Recovery was fast and the patient was discharged satisfied after three days. ESP block is currently used in various types of abdominal surgery (cholecystectomy, ventral hernioplasty, hysterectomy, nephrectomy) but as regards adrenalectomy no studies were found [1- 9].
Laparoscopic andrenalectomy (LA) has rapidly become the gold standard in management of adrenal tumors, especially for better outcomes in terms of cosmesis, hospital stay, less operative time and blood loss and rapid activity restoration [1]. Despite that, the mass dimension can be a relative contraindication for the mini-invasive approach, especially due to the malignant potential and the risk of intraoperative rupture. Moreover, the dimensional cut off is the main subject of discussion [2].
We decided to approach this case with a mini-invasive approach due to our center expertise in laparoscopic surgery, because at the preoperative CT scan the mass was less than 10 cm with no clear signs of malignancy, and because we are extremely clear with patient explaining that we will have converted in any case of intraoperative need. In any case, the intraoperative findings were comforting because we didn't find any neighboring organs invasions and no difficulties in mass detachment, as also no mass rupture. Moreover, to avoid sealing, the mass was carefully removed with an endobag from the Pfannestiel incision.
Literature reported cases successfully performed in laparoscopy also for non-functional mass near to 18 cm [1,2]. However, the center expertise in minimally invasive surgery should always be considered [2]. In case of local invasion or vascular infiltration open approach is more suitable and indicated [2].
Some studies compared different mini-invasive approaches: the laparoscopic or retroperitoneal adrenalectomy [10]. In a recent systematic review comparing these two techniques, no differences were found in terms of blood loss, hospitalization, pain score, operative time, complications, and return to normal activity. However, the lack of high-quality data in literature makes still difficult to make definitive conclusions [11]. The surgeon expertise and comfort in one technique should rather guide the choice.
The pre-operative and intra-operative findings deposed for a non-functioning and probably benign mass; however, the definitive confirmation came only with the result of the histological examination.
In our case, the final histopathological result of the adrenal mass deposed for a benign ganglioneuromas. Ganglioneuromas (GN) account for less than 5% of adrenal masses, with a slight female prevalence, and occurs more frequently in children and young adults [12]. However, some recent studies have shown they may also be found over 40 years old [13]. GN originates from the autonomous sympathetic nervous system, either central or peripheral, and presents the least aggressive profile among the neural crest‑derived tumor, so the prognosis is excellent after surgical resection, in contrast to other less differentiated neuroblastic tumors (ganglioneuroblastoma and neuroblastoma) [12]. GNs are detected mostly by accident, being usually asymptomatic and endocrinologically inactive; however, they can grow and become large enough to cause symptoms due to mass effect. Hormone hypersecretion is infrequent: cathecholamines in a minority of cases, rarely dopamine [14]. It remains difficult to discriminate a GN from other adrenal masses according to radiological features, thus histology has a central role.
Adrenal masses presenting characteristics of malignancy should undergo PET scan because that may help to differentiate malignant from benign lesions with 100% sensitivity and 98% specificity [15]. Our patient underwent to a 18FDG PET/TC, presenting a large adrenal lesion, coupled with two indefinite liver nodules.
Conclusion
This case has shown that the combination of ESP block with the recognized efficacy of the minimally invasive approach may have a synergistic effect on postoperative pain. Moreover, the multidisciplinary approach has permitted an optimal result in terms of clinical outcomes and patient’s satisfaction, with a very fast daily activity restauration.
Conflict of Interest: All authors declare no source of funding or conflict of interest
References
- Al-Jalabneh T, Al-Shawabkeh O, Al-Gwairy I, et al. Laparoscopic Versus Open Adrenalectomy: a Retrospective Comparative Study. Med Arch, 2021; 75(1): 41-44.
- Agrusa A, Romano G, Frazzetta G, et al. Laparoscopic adrenalectomy for large adrenal masses: single team experience. Int J Surg, 2014;12 Suppl 1: S72-74.
- Fassnacht M, Arlt W, Bancos I, et al. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol, 175(2): G1-G34. doi: 10.1530/EJE-16-0467.
- Tulgar S, Selvi O, Senturk O, et al. Ultrasound-guided erector spinae plane block: Indication, complication, and effects on acute and chronic pain based on a single-center experience. Cureus, 2019; 11: e3815.
- McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: A critical review. Psychol Med, 1988; 18: 1007-1019.
- Chin KJ, Malhas L, Perlas A. The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: A report of 3 cases. Reg Anesth Pain Med, 2017; 42: 372-376.
- Luis-Navarro JC, Seda-Guzman M, Luis- Moreno C, et al. Erector spinae plane block in abdominal surgery: Case series. Indian J Anaesth, 2018; 62: 549-554.
- Watcha FM, White PF. Postoperative nausea and vomiting. Its etiology, treatment and prevention. Anesthesiology, 1992; 77: 162-184.
- Napolitano LM, Iacovetta D, Cellini C, et al. Chirurgia laparoscopica dei tumori del surrene: indicazioni e tecniche. G Chir Vol. 31 - n. 6/7 - pp. 336-338 Giugno-Luglio 2010 Actas Urol Esp, 2006; 30(9): 926-932.
- Conzo G, Tartaglia E, Gambardella C, et al. Minimally invasive approach for adrenal lesions: Systematic review of laparoscopic versus retroperitoneoscopic adrenalectomy and assessment of risk factors for complications. Int J Surg, 2016; 28 Suppl 1: S118-123.
- Arezzo A, Bullano A, Cochetti G, et al. Transperitoneal versus retroperitoneal laparoscopic adrenalectomy for adrenal tumours in adults. Cochrane Database Syst Rev, 2018; 12(12): CD011668.
- Lee JH, Chai YJ, Kim TH, et al. Clinicopathological features of ganglioneuroma originating from the adrenal glands. World J Surg, 2016; 40: 2970-2975. 10.1007/s00268-016-3630-y
- Linos D, Tsirlis T, Kapralou A, et al. Adrenal ganglioneuromas: incidentalomas with misleading clinical and imaging features. Surgery, 2011; 149: 99-105. DOI: 10.1016/j.surg.2010.03.016
- Geoerger B, Hero B, Harms D, et al. Metabolic activity and clinical features of primary ganglioneuromas. Cancer, 2001; 91: 1905-1913.
- Mackie GC, Shulkin BL, Ribeiro RC, et al. Use of [18F] fluorodeoxyglucose positron emission tomography in evaluating locally recurrent and metastatic adrenocortical carcinoma. J Clin Endocrinol Metab, 2006; 91: 2665-2671.
- Wagemans MF, Scholten WK, Hollmann MW, et al. Epidural anesthesia is no longer the standard of care in abdominal surgery with ERAS. What are the alternatives? Minerva Anestesiol, 2020; 86(10): 1079-1088.

