Two Interesting Presentations of Rare Penile Vascular Lymphatic Malformations
Hamish Walker*, Gemma Sutton, Mushfique Alam and Charlotte Victoria Melling
Department of Paediatric Surgery, Alder Hey Children's NHS Foundation Trust, Eaton Rd, Liverpool, L12 2AP, UK
Received Date: 12/06/2023; Published Date: 30/10/2023
*Corresponding author: Hamish Walker, Department of Paediatric Surgery, Alder Hey Children's NHS Foundation Trust, Eaton Rd, Liverpool, L12 2AP, UK
Abstract
In this article we discuss two cases of rare penile vascular lymphatic malformations presenting as atypical variants of established urological conditions. In the first case a 14-year-old boy presents with penile swelling. Initial ultrasound imaging suggested priapism but subsequent magnetic resonant imaging confirmed a lympho-venous malformation of the superficial penile connective tissue. In the second case a 4-month-old boy presented with ballooning of his excessive foreskin. A venous malformation had caused a mega prepuce like appearance.
Keywords: Pediatric urology; Penile vascular lymphatic malformation
Case 1: Penile Swelling
An 11-year-old attended A&E with a 1-week history of painless penile swelling predominately on the right side. He was having regular erections that would spontaneously resolve. The swelling was over the mid shaft of the penis and there was no history of trauma or bites. There were no difficulties in passing urine although tight foreskin sometimes gave him discomfort. Mum reported that his penis has always looked large. He was otherwise fit and well.
On examination the meatus and glans looked normal although the foreskin was not fully retractable. A small cutaneous vascular birthmark was noted separate from the swelling on the ventral shaft (Figure 1). Peisis sign was not present with no resolution of swelling seen on perineal compression. Both testes were felt in the scrotum with no abnormality.

Figure 1: Initial presentation, birthmark and swelling visible.
Initial ultrasound scan (USS) suggested priapism with marked focal enlargement on the right side of the distal shaft of the penis. Vessels throughout the corpora cavernosa were engorged with oedema of subcutaneous tissue. Following this magnetic resonant imaging (MRI) was obtained which suggested an underlying lymphatic or veno-lymphatic malformation with healthy underlying corpora (Figure 2). These images were then discussed with the local adult urology unit who advised to treat as partial high flow priapism secondary to underlying lymphovascular anomaly. The possibility of embolization was discussed with the local interventional radiologist who felt that there was a risk of impotence or skin necrosis and because there was no clear evidence of AV shunting there was no indication for embolization.

Figure 2: T2 weighted MRI.
Overall, the imaging is all consistent with a lympho-venous malformation of the superficial penile connective tissue. Follow up in clinic revealed that he continues to get normal morning erections which resolve spontaneously. On examination, the penis is unchanged with an approximate 50p size swelling on the right shaft that fluctuates and is non-tender with no overlying erythema.
It was explained that there does not appear to be any danger of damage to the important internal structures of the penis and his erectile function. The difficulty is likely to be encountered with mobility of the foreskin in the future. However, surgery is not a straightforward option for these problems. The underlying abnormality of the lymphatics often leads to recurrence, poor wound healing and chronic weeping.
It is difficult to say if the lesion will change significantly or not in the future. We have advised protective garments for contact sport and further follow up will ensue.
Case 2: Ballooning
A 4-month-old boy presented with large ballooning of the foreskin which parents have to squeeze urine out of in a very fine stream. Parents felt that he often feels in pain when he is full of urine. There was no history of UTI or any other medical concerns. Examination revealed a very large and stretched foreskin, not in the classical megaprepuce cone-shaped configuration with normal attachments at base of the penis (Figure 3). Urine was expressed through the very tight phimotic opening. There was a normal feeling glans penis within the empty enlarged foreskin and a midline penile raphe ascending in a spiral around to the left. Both testes were well descended and the child was otherwise fit and well.
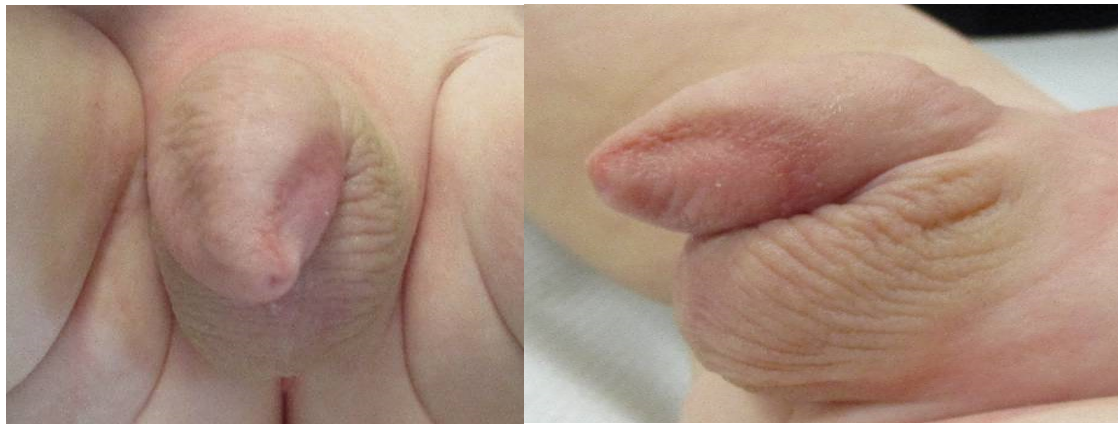
Figure 3: a) Frontal and lateral views b) T2 weighted MRI.
USS was performed and suggested normal corpora, excessive foreskin and pinhole exit. Prominent veins were noted consistent with a venous malformation. Both testes were normal and renal USS was unremarkable. A dorsal slit was performed for symptomatic relief. At operation excessive outer and inner prepuce were both noted not in the classical mega prepuce cone shape and this was felt to be a mega prepuce variant.
Discussion
Penile vascular lymphatic malformations are rare and consequently are subject to misdiagnosis. Vascular malformations occur during embryological development and are typically caused due to congenital errors in vessel morphogenesis, resulting in ectatic venous channels1,2. They are often diagnosed at birth or noticed by parents/ children as the lesions grow. The patient commonly presents with swelling that may or may not have overlying skin discolouration, associated bleeding, thrombosis, or ulceration. Lesions may be asymptomatic or have associated pain if exerting pressure on nearby structures, or effect functionality (difficulty passing urine, foreskin mobility, erection function).
Depending on the nature of the malformation, the lesion may be slow or rapidly growing, contributing factors to rapid growth include hormonal stimulation, trauma, and infection. Vascular malformations that occur in childhood are benign; it is thought that there is potential for malignant transformation, but this has not yet been reported3. Accurate diagnosis through thorough history taking, examination and cross-sectional imaging including Doppler USS and MRI is vital to an ensure an appropriate diagnosis and to rule out more sinister pathologies.
Both cases discussed presented as atypical variants of established conditions. The first case presented as a partial high flow priapism and the second as a mega prepuce variant. In both cases imaging was vital for diagnosis and formulation of management plan. Treatment options for vascular malformations include conservative management, sclerotherapy, embolization and surgery4. Before commencing treatment, it is important to review the lesions pathophysiology, etiology and consequence of procedure, a multi-disciplinary team approach is always recommended. Consideration of surgery needs to be balanced against the risk of exacerbation, recurrence, cosmetic disfigurement and poor wound healing associated with lymphatic malformations. Sclerotherapy has been found to be a successful treatment for macrocystis vascular malformations5, however the cases discussed in this article were not amenable to sclerotherapy.
Conclusion
- Vascular malformations of the penis are rare.
- Both cases presented as atypical presentations/ variants of established conditions. The first case presented as a partial high flow priapism and the second as a mega prepuce variant.
- Consideration of surgery needs to be balanced against risk of exacerbation, recurrence and poor wound healing. Treatments including sclerotherapy and embolization should be explored when suitable.
With thanks to both children and their parents for consenting to images and Alder Hey radiology department for identifying key images.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Highlights
- Penile vascular lymphatic malformations are rare
- Presentation may mimic other urological conditions
- Management requires multi-disciplinary input
Surgery for such lesions needs to be carefully balanced against risks
References
- Behravesh S, et al. Venous malformations: clinical diagnosis and treatment. Cardiovascular Diagnosis and Therapy, 2016; 6(6): 557.
- Kulungowski AM, et al. Vascular anomalies of the male genitalia. Journal of Paediatric surgery, 2011; 46(6): P1214-1221.
- Akin Y, et al. Rare malformation of glans penis: Arteriovenous malformation, Nigerian Journal of Clinical practice, 2013; 16(3).
- Merrow AC, et al. Revised Classification of Vascular Lesions from the International Society for the Study of Vascular Anomalies: Radiologic-Pathologic Update. Paediatric Imaging, 2014; 36(5).
- Marrocco-Trischitta MM, et al. Sclerotherapy for venous malformations of the glans penis. Adult Urology, 2001; 57(2): P310-313.

