Tragedy After Conservative Treatment Choice, TAAAD Requiring Surgery Due to Progressive Dissection
Masuyama S*, Inoue T and Ichihara T
Department of Cardiovascular Surgery, Ohtakanomori Hospital, Japan
Received Date: 05/06/2023; Published Date: 27/10/2023
*Corresponding author: Shinji Masuyama, MD, Department of Cardiovascular Surgery, Ohtakanomori Hospital, 113 Toyoshiki, Kashiwa 277-0863, Chiba, Japan
Abstract
Type A Acute Aortic Dissection (TAAAD) is a serious disease that often has fatal consequences unless prompt surgical repair is performed. However, conservative treatment may be possible, depending on the morphology and circumstances of the dissected aorta. In such cases where conservative treatment is chosen, changes in the aortic lumen and re-expansion of the dissected thoracic aorta may progress to aortic rupture. In this report, we describe two cases in which patients were initially treated conservatively for TAAAD but subsequently underwent emergency surgery due to major changes in rapid TAAAD.
Keywords: TAAAD; Conservative Treatment; Progressive Dissection
Introduction
TAAAD is a serious disease that often results in fatal consequences unless prompt surgical repair is performed. However, depending on the morphology and condition of the dissected aorta, there are rare cases that can be treated conservatively. In such cases, even after conservative treatment is chosen, the situation may become dangerous due to changes in TAAAD with re-expansion. Patients with these changes may not show any outward symptoms, which increases the possibility of missing the optimal timing of surgery. We have performed more than 330 emergency surgeries for TAAAD during the past 8 years since 2014. In this report, we describe two patients with TAAAD who were initially treated conservatively but then underwent emergency surgery after sudden progression of TAAAD.
Case Report
This study was approved by the ethics committee of our institution on May 17th, 2022. The patients provided written informed consent for treatment and the publication of this case report.
Case 1
A 76-year-old woman developed chest pain. On arrival at the ER, CT showed a TAAAD of 41 mm with a false lumen (FL) of 14 mm with an intermural hematoma (IMH) (Figure 1A). However, the patient’s symptoms were alleviated, and the decision was made to monitor the TAAD without performing surgical intervention. One week later, CT showed that the sizes of the ascending aorta (ASA) and arch remained unchanged, and the FL had further decreased to 4 mm (Figure 1B); therefore, the patient was discharged. One week after discharge, the patient again developed chest pain and was brought to our hospital. Enhanced CT showed that the ASA had enlarged to 52 mm, and the FL was patent (Figure 1C). Because of the persistent symptoms, the patient was referred for emergency surgery.
Surgery was performed through a median sternotomy. Cardiopulmonary bypass (CPB) was started from the lt.FA to the RA. A LV vent was inserted, and the ASA was clamped and transected. Cardiac arrest was performed by selective cerebral perfusion (SCP). The aortic root dissection involved two-thirds of the aortic circumference, but the aortic valve was preserved. After cooling to 28°C, the head was lowered and the circulation was stopped. After retrograde cerebral perfusion (RCP), SCP was started through the basilar artery (BA) and left carotid artery. The aorta was separated just proximal to the first branch. An intimal tear of 4 cm was observed in the medial superior part of the ASA. Proximal arch transection was performed and an artificial graft was selected. After anastomosis of the distal graft and aortic transection, the proximal graft was also anastomosed. The operative time was 215 min, CPB time was 134 min, aortic clamping time was 97 min, circulatory arrest time was 32 min, and SCP time was 19 min. The patient had a good postoperative course and was discharged without complications 3 weeks after surgery.
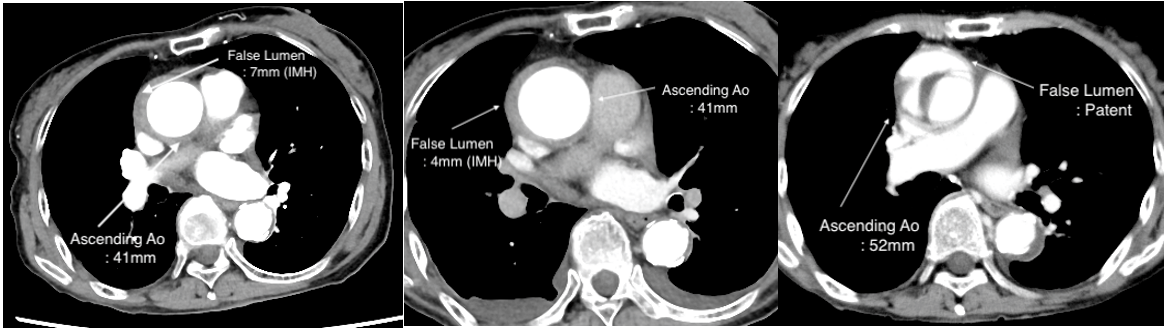
Figure 1: CT findings in Case 1.
A: At the time of presentation to the ER.
B: At 1 week after admission.
C: At 2 weeks after initial presentation.
Case 2
A 78-year-old man developed sudden back pain that subsequently radiated to his right scapula, causing him to present to the ER. CT revealed a TAAAD. However, the ASA diameter was only 40 mm, and the FL was 11 mm with an IMH (Figure 2A). As he had no symptoms at that time, he was temporarily admitted to the ICU for observation. The patient’s progress was good. One week later, CT showed that the diameter of the ASA had not changed, and the FL had almost disappeared (Figure 2B). However, at 2 weeks after admission, the ASA had enlarged to 47 mm and the FL was 14 mm with an IMH, indicating a re-dissection (Figure 2C). “Virtual angioscopy” revealed an intimal tear from the medial side of the descending aorta (Figure 3) [1]. In addition, the CT Hounsfield unit (HU) value of the FL was measured to confirm the dissection status of the ASA. The HU value of the FL was 47 HU, suggesting that blood from the true lumen of the ASA was flowing into the FL (Fig. 3B). Based on these findings, we diagnosed this patient as having a TAAAD with an IMH and determined that emergency surgery was indicated.
CPB was set up from the lt.FA to the RA. The ASA was opened, and SCP was performed. Cardioplegia was obtained. The greater curvature of the ASA before the BA was held while the lesser curvature side was cut up to the arch to create a peripheral anastomosis. The dissection was observed to involve half the aortic circumference. The peripheral side was anastomosed. Next, the central side was checked. Dissection was observed from the noncoronary cusp to the right coronary cusp. The proximal side was anastomosed. The operative time was 175 min, CPB time was 130 min, aortic clamping time was 78 min, circulatory arrest time was 39 min, and SCP time was 26 min. The patient had a good postoperative course and was discharged without complications 2 weeks after surgery.

Figure 2: CT findings in Case 2.
A: At the time of presentation to the ER.
B: At 1 week after admission.
C: At 2 weeks after initial presentation.
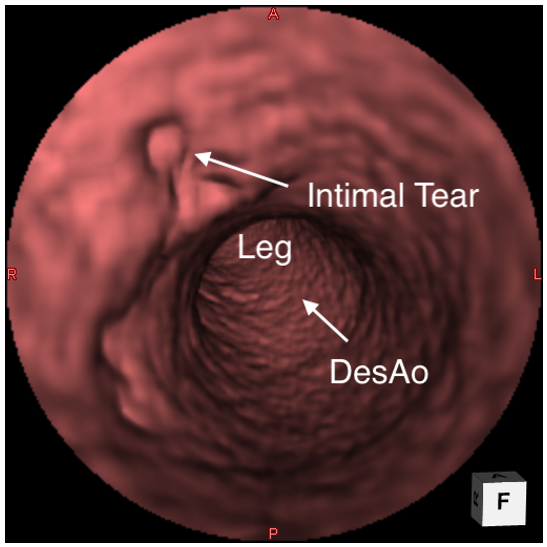
Figure 3: Virtual angioscopy in Case 2.
Discussion
The Japanese Registry of All Cardiac and Vascular Diseases reports that there were 6,788 emergency surgeries for TAAAD in Japan in 2020, with a mortality rate of 11.8%. The mortality rate of TAAAD increases as the time to surgery increases [2]. Furthermore, refusal to undergo surgery despite its necessity leads to a high mortality rate of 49.7%. In cases such as the present cases where the patient was diagnosed with TAAAD at the time of presentation but was treated conservatively because the condition was stable, rapid recurrence or deterioration is directly related to mortality and the patient’s emotional condition. In addition, aortic re-dissection may cause few symptoms, making it difficult to determine the optimal time to perform surgery. There is a reported case in which a patient receiving conservative treatment for TAAAD died due to worsening symptoms [3].
In general, emergency surgery is required for TAAAD in patients with an ASA diameter >50 mm, FL >10 mm, Aortic valve regurgitation (>3+), tamponade, and pain. For other patients with stable TAAAD, conservative treatment is possible. In most cases, the aortic diameter remains the same or the FL shrinks, and the patient is often discharged; however, in rare cases, re-dissection may occur. Generally, most patients with TAAAD with an IMH or PAU who are stable after dissection remain the same or become mildly ill; at our institution, such patients are discharged after 1 week if there are no changes in CT findings and symptoms. Most of these patients are still in good health even after several years, but a small percentage are in a dangerous state without being aware of it.
Stable TAAAD may be monitored by plain CT alone for fear of worsening renal function; however, plain CT is not sufficient for the evaluation of aortic dissection. In such cases, Virtual angioscopy can be used to determine changes in the intimal tear at the site of aortic dissection and determine when itis necessary [1]. It is important to monitor the progression of TAAAD and consider the need for contrast-enhanced CT or reoperation. In the present study, we described two cases of re-dissection after conservative follow-up of TAAAD.
Conclusion
Although TAAAD is a condition that often requires prompt surgical repair, conservative treatment may be possible depending on the morphology and circumstances of the dissected aorta.
Such conservative treatment has been observed in sporadic cases leading to aortic rupture due to re-expansion of the thoracic aorta. In this report, we discuss two cases in which initially, conservative treatment was given for TAAAD, followed by emergency surgery due to rapid and significant changes in the TAAAD.
Grant Information: The authors received no specific funding for this work.
Acknowledgments: We thank Kelly Zammit, BVSc, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
References
- Masuyama S, Nakajima H, Morishima M, Osada H. Virtual Angioscopy finds the intimal tear of an acute thoracic aortic dissection. European Journal of Cardio-Thoracic Surgery, 2012; 41: 454.
- Yamaguchi T, Nakai M, Sumita Y, et.al. Current status of the management and outcomes of acute aortic dissection in Japan Analyses of nationwide Japanese Registry of All Cardiac and Vascular Diseases-Diagnostic Procedure Combination data. European Heart Journal Acute Cardiovascular Care, 2020; 9(53): s21-31.
- Kanda T, Tawarahama K, Nakamura N, et.al. Difficulty Diagnosing Retrograde Type A Aortic Dissection with Intramural Hematoma and Risk of Re-dissection and Rupture A Report of Two Cases. Inten Med, 2021; 60: 3121-3124.

