A Rare Case: Bilateral Tuberositas Tibia Avulsion
Mehmet Utku Çiftçi*
Department of Orthopedics and Traumatology, University of Health Sciences, Bakırköy Dr. Sadi Konuk Training and Research Hospital, Istanbul, Turkey
Received Date: 30/05/2023; Published Date: 10/10/2023
*Corresponding author: Mehmet Utku Çiftçi, MD, Department of Orthopedics and Traumatology, University of Health Sciences, Bakırköy Dr. Sadi Konuk Training and Research Hospital, Istanbul, Turkey
Introduction
Fractures involving the proximal tibial epiphysis constitute 0.5% of all epiphyseal fractures [1]. These are extremely rare fractures. These fractures are usually classified according to the Salter-Harris classification or the classification system specific to the proximal tibial epiphysis developed by Watson-Jones [2] and modified by Ryuve Debenham [3]. Avulsion fractures of the tuberositas tibia in adolescents are a rare injury to the proximal tibial physis and the fracture line may extend toward the proximal tibial articular surface [4].
In this article, we present a rare case of bilateral tuberositas tibia avulsion and patellar tendon rupture, which occurred spontaneously after sportive activity in an adolescent patient who did not have any systemic disease and did not use steroids or any other drugs.
Case
A 13-year-old male patient was admitted to our emergency outpatient clinic with complaints of falling and inability to walk after sudden ejaculation, accompanied by noise from both knees while running in the gym without trauma. Physical examination revealed swelling, tenderness, and limitation of motion in both the knees. The patient could not perform straight leg raise. Both the knee flexion and extension movements are limited and painful. Radiographs showed avulsions in the bilateral tuberositas tibia, and the patellar tendon and patella were displaced proximally due to the quadriceps pull. The patient was diagnosed with bilateral tuberotis tibial avulsion, a long leg splint was applied, and he was admitted to the ward for surgery. Under general anesthesia, both knees were entered with an anterior incision. Both tuberositas tibias were completely avulsed together with the patellar tendon. The tibial fragment was reduced and repaired with one scaly cannulated screw and one suture anchor. The stabilization of the fragments was checked with per-op flexion and extension movements. It was found to be stable and the operation was completed. The patient, who was followed up in the service, had no wound problems and was discharged on the 4th day with a bilateral long leg cast. In the 6th week of follow-up, the cast was removed and physical therapy was initiated. Joint range of motion and quadriceps strengthening exercises were used in physical therapy. Full range of motion was achieved in the post-op 3rd month. From the sixth month, he was allowed to return to normal activities.
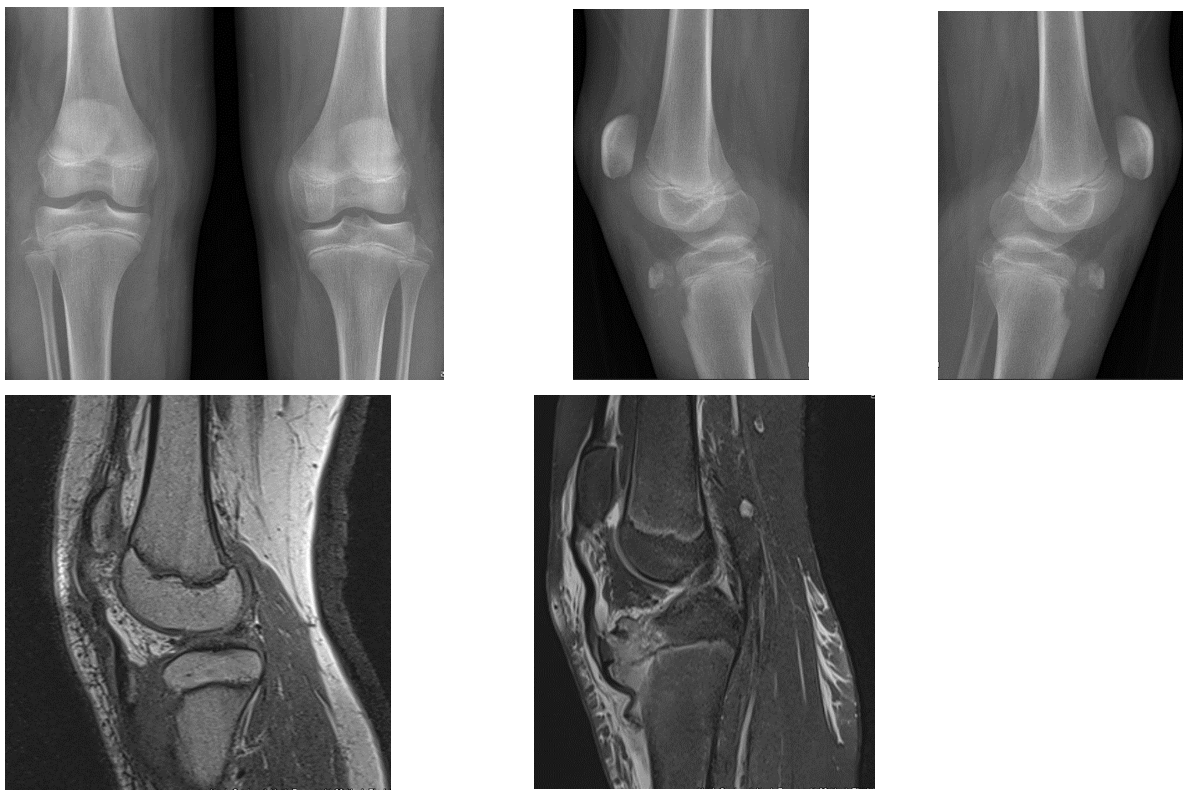
Figure 1: Preoperative X-rays and MRI images of the patient.
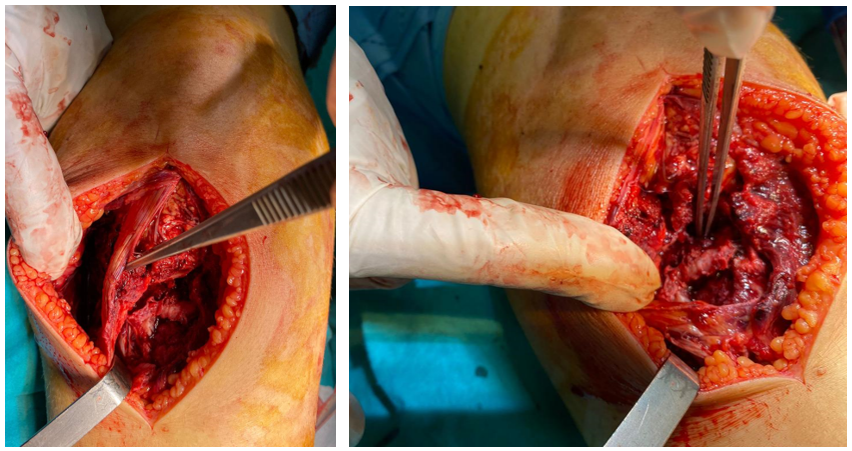
Figure 2: Peroperative images of the patient.
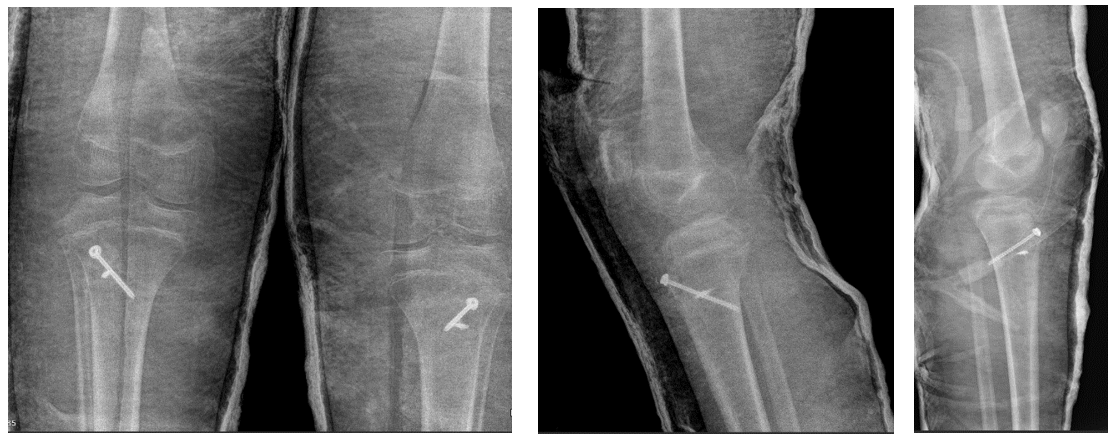
Figure 3: Postoperative X-ray images of the patient.

Figure 4: 12-month clinical images of the patient.
Discussion
Proximal tibial physeal injuries are rare and are thought to be due to the inherent stability afforded by the anatomical arrangement of the epiphysis [1]. Disruption of this anatomy limits knee extension and function. In tuberositas tibia avulsion, which is mostly seen in young adults, this anatomical integrity is disrupted, knee movements cannot be performed and disability occurs. Tuberositas may be an underlying metabolic or skeletal system pathology in tibial avulsions or may be seen without any predisposing factors. Although proximal tibial epiphyseal fractures have rarely been reported in children and adolescents, there is a cumulative incidence of bilateral occurrence, and physiological changes during closure preparation of the physis may guide epiphyseal separation [5].
Harb et al. reported that there were 7 cases previously presented in their literature review and stated that 1 of these cases had concomitant osteogenesis imperfecta disease and the others were healthy young adolescents. In their case, they presented a case of bilateral tuberositas tibia avulsion fracture in a 14-year-old patient with vitamin D deficiency [1]. Ryu et al. reported clinically asymptomatic Os-good-Schlatter in the radiographs of the adolescent patient in their case report [3]. When the old radiographs in our case were also examined, Os-good-Schlatter findings were observed. In addition, there was no vitamin D deficiency or systemic disease in this case.
The treatment of these fractures depends on several factors, including the degree of displacement of the fragments. [1] A clear distinction between transitional fractures and open epiphyseal fractures is strongly recommended. Since the partially closed epiphysis is an indicator of high skeletal maturity, limb length discrepancies and angular deformities are not expected after trauma [6]. Many methods for the treatment of proximal tibial avulsions have been reported in the literature. These include cannulated screws [7], plate screws [8], and tension band fixation [9]. Harb et al. stated that they applied conservative treatment with plaster in their cases [1]. In our case, necessary fixation was achieved using scaly cannulated screws and suture anchors in accordance with the literature. After fixation and sufficient immobilization, no treatment-related complications were observed.
Conclusion
Tuberositas tibia avulsion and concomitant patellar tendon rupture, which are frequently seen in young adults, are extremely rare. We believe that these types of injuries can be treated without any problems after the diagnosis is made by anamnesis, physical examination, and appropriate imaging techniques by choosing the appropriate treatment method for the fracture type.
Declaration of conflicting interests: The authors declared no conflicts of interest concerning the authorship and/or publication of this article.
Funding: The authors received no financial support for the research and/or authorship of this article.
References
- Harb Z, Malhi A. Bilateral Simultaneous Avulsion Fractures of the Proximal Tibia in a 14-Year-Old Athlete with Vitamin-D Deficiency. Case Rep Orthop, 2015; 2015: 783046. doi: 10.1155/2015/783046. Epub 2015 Sep 6. PMID: 26425381; PMCID: PMC4575729.
- Watson-Jones R. “Injuries of the knee,” in Fractures and Joint Injuries, J. Wilson, Ed., Churchill Livingstone, Edinburgh, UK, 5th edition, 1976; pp. 1047–1050.
- Ryu RKN, Debenham JO. “An unusual avulsion fracture of the proximal tibial epiphysis. Case report and proposed addition to the Watson-Jones classification,” Clinical Orthopaedics and Related Research, 1985; 194: pp. 181–184.
- Christie MJ, Dvonch VM. Tibial tuberosity avulsion fracture in adolescents. J Pediatr Orthop, 1981; 1(4): 391-394. doi: 10.1097/01241398-198112000-00006. PMID: 7334117.
- Omar M, Petri M, Ettinger M, Decker S, Krettek C, Gaulke R. Simultaneous bilateral transitional fractures of the proximal tibia after minor sports trauma. Case Rep Orthop, 2013; 2013: 724802. doi: 10.1155/2013/724802. Epub 2013 Sep 28. PMID: 24191212; PMCID: PMC3804443.
- Ruffing T, Muhm M, Winkler H. The mature twoplane and triplane fracture : transitional fractures of the distal tibia combined with typical fracture patterns of adults. Unfallchirurg, 2011; 114(8): 730–735.
- Potenza V, Caterini R, Maglione P, Bisicchia S, Farsetti P. “Simultaneous bilateral flexion-type salter-harris ii fractures of the proximal tibia: a case report and review of the literature,”
- Omar M, Petri M, Ettinger M, Decker S, Krettek C, Gaulke R. “Simultaneous bilateral transitional fractures of the proximal tibia after minor sports trauma,” Case Reports in Orthopedics, 2013; 2013. Article ID 724802, 5 pages, 2013.
- Yoshino N, Watanabe N, Fukuda Y, et al., “Simultaneous bilateral Salter-Harris type II injuries followed by unilateral Salter- Harris type III injury of the proximal tibia in an adolescent with osteogenesis imperfecta,” Journal of Orthopaedic Science, 2010; 15(1): pp. 153–158.

