The Aorto-Mesenteric Clamp Syndrome in the Young
Bouali Mounir, Azhari Fadwa*, Elbakouri Abdellilah, Elhattabi Khalid, Bensardi Fatimazahra, Khaliq Khalid, Fadil Abdelaziz
-Visceral Surgery Emergency Department P35 , University Hospital Center Ibn Rochd, Casablanca, Morocco
-Faculty of Medicine and Pharmacy, Hassan II University, Casablanca, Morocco
Received Date: 31/05/2023; Published Date: 09/10/2023
*Corresponding author: Fadwa Azhari, Visceral Surgery Emergency Department P35 , University Hospital Center Ibn Rochd, Casablanca, Morocco, Faculty of Medicine and Pharmacy, Hassan II University, Casablanca, Morocco
Abstract
Introduction and Importance: Wilkie's syndrome, also known as aorto-mesenteric clamp syndrome, is characterised by compression of the duodenum in its third portion due to narrowing of the space between the superior mesenteric artery and the aorta. Its presenting symptoms are consistent and include obstruction of the proximal small intestine. However, the physical and biological findings are not specific. Nevertheless, many imaging methods are useful for its diagnosis. The management of this condition is surgery. We report a case of SPAM in a 16-year-old patient with upper obstruction, senile dementia and anorexia, who consulted for repeated vomiting more than one week old.
Case presentation: A 16-year-old patient, without any particular pathological history, was brought in for emergency consultation for periumbilical abdominal pain with postprandial vomiting, and altered general condition with weight loss not quantified. The clinical examination revealed a conscious patient who was hemodynamically and respiratory stable. An abdominal CT scan with vascular reconstruction allowed the diagnosis of SPAM, the angulation between the AMS and the aorta being calculated at 15°. Medical treatment was first undertaken: placement of a nasogastric tube and parenteral fluid and metabolic intake. After three days of treatment, there was no significant clinical or biological improvement, with the gastric tube returning an average of 1000 ml per day. The decision was then made to operate on the patient.
Surgical exploration, under laparoscopy, revealed gastric and duodenal distension upstream of the AMS imprint, while downstream of it the small intestines were flat. A transmesocolic gastrojejunal anastomosis was performed.
Clinical Discussion: The aorto-mesenteric clamp syndrome is extremely low, with an incidence of 0.2% in 6,000 in radiological studies. Several an etiological factor have been described, the most important of which is a deformity of the lumbar spine, which contributes to this mechanism by projecting the aorta forward.
Conclusion: Wilkie's syndrome is a rare entity, which remains a little-known syndrome in a general practitioner, underdiagnosis can put a patient at risk and suffer serious complications, therefore the physician is obliged to be aware of this pathology for timely treatment
Keywords: Wilkie's Syndrome; Superior mesenteric artery syndrome; Duodenal obstruction
Introduction
Mesenteric clamp syndrome is defined as compression of the third portion of the duodenum (D3) between the superior mesenteric artery (SMA) anteriorly and the aorto-rachidian plane posteriorly [1].
Duodenal compression may be partial or complete, acute or chronic, with symptoms ranging from vague postprandial epigastric pain and nausea to recurrent postprandial vomiting with severe weight loss and electrolyte imbalances [2].
Surgical treatment (gastrojejunal or duodenojejunal bypass) is sometimes required, in which conservative treatment fails to alleviate the clinical picture and can be performed laparoscopically or by open surgery [3].
We report a case of aorto-mesenteric clamp syndrome and discuss the etiopathogenetic aspects, diagnostic and therapeutic means.
Clinical Case
A 16-year-old patient, without any particular pathological history, was brought in for emergency consultation for periombilical abdominal pain with postprandial vomiting, and altered general condition with weight loss not quantified. The clinical examination revealed a conscious patient who was hemodynamically and respiratory stable, with a BMI of 10.29 and a fasting limp. Biology showed uraemia: 0.42 g/l, creatinine: 7.9mg/l, natraemia: 140mmol/l. An abdominal CT scan with vascular reconstruction allowed the diagnosis of SPAM, the angulation between the AMS and the aorta being calculated at 15°, with gastroduodenal distension (Figure 1, 2). Medical treatment was first undertaken: placement of a nasogastric tube and parenteral fluid and metabolic intake. After three days of treatment, there was no significant clinical or biological improvement, with the gastric tube returning an average of 1000 ml per day. The decision was then made to operate on the patient.
Surgical exploration, under laparoscopy, revealed gastric and duodenal distension upstream of the AMS imprint, while downstream of it the small intestines were flat. A transmesocolic gastrojejunal anastomosis was performed. The evolution was marked by clinical improvement, the gastric tube did not return, transit was resumed on the second postoperative day and oral feeding was authorised on D5 and declared out on D6 postoperatively.

Figure 1: CT cross section through the third duodenal portion showing compression of the third duodenum by the superior mesenteric artery (SMA) on the aorta.
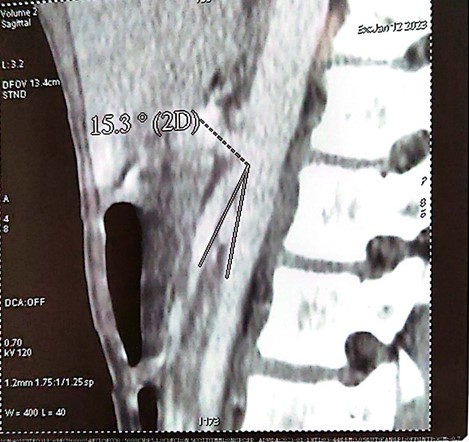
Figure 2: his aorto-mesenteric angle ranges 15, 3°.
Discussion
The aorto-mesenteric clamp syndrome was described by Rokitansky in 1861, its frequency is extremely low, with an incidence of 0.2% in 6,000 in radiological studies [4].
Aorto-mesenteric clamp syndrome most commonly affects women between the ages of 10 and 39 [5].
Several aetiological factors have been described, the most important of which is a deformity of the lumbar spine, which contributes to this mechanism by projecting the aorta forward [6]. Anatomical factors are also involved in the genesis of this syndrome: the low insertion of the AMS on the aorta, the shortness of the ligament of Treitz, which causes a high insertion of the duodeno-jejunal angle [7,8].
In our case, none of these abnormalities were found.
As with duodenal obstruction, SPAM manifests as early post prandial vomiting, abdominal pain and satiety, in other cases the symptomatology is more chronic with repeated post prandial fullness and intermittent vomiting [9-11].
Advances in imaging allow the diagnosis to be made preoperatively. Standard radiography confirms high obstruction, and CT calculates the angle between the AMS and the aorta which is reduced from 7° to 22°, whereas it is normally between 25° and 60°. The aorto-mesenteric distance is also reduced and measures 2-8 mm, whereas the normal distance is 10-28 mm [9,12,13]. In our patient the angle between the AMS and the aorta calculated on the CT images was 15°.
Currently, open and laparoscopic gastrojejunal or duodenojejunal bypass is considered the operation of choice in Wilkie syndrome, with a high success rate [14]. Nevertheless, it has several postoperative complications related to the intervention on the continuity of the gastrointestinal tract, such as anastomotic leakage, intraperitoneal abscess formation, dumping syndrome, stenosis of the anastomosis. SMA transposition surgery not only preserves the continuity of the gastrointestinal tract, but also permanently relieves compression of the 3rd part of the duodenum, as well as other structures such as the splanchnic nerves that innervate the duodenum [15].
Conclusion
Wilkie's syndrome is a rare entity, which remains a little-known syndrome in a general practitioner, underdiagnosis can put a patient at risk and suffer serious complications, therefore the physician is obliged to be aware of this pathology for timely treatment.
Consent Written: Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors; Contributions: This work was carried out in collaboration among all authors. All authors contributed to the conduct of this work. They also declare that they have read and approved the final version of the manuscript.
Provenance and Peer Review: Not commissioned, externally peer-reviewed
Conflicts of interest: None
Sources of funding: None
Ethical approval: As per international standard written ethical approval has been collected and preserved by the author(s).
Consent: Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution: This work was carried out in collaboration among all authors. All authors contributed to the conduct of this work. They also declare that they have read and approved the final version of the manuscript.
Research registration (for case reports detailing a new surgical technique or new equipment/technology): None
Guarantor: F A
References
- Molina Proaño GA, Cobo Andrade MM, Guadalupe Rodríguez RA, Gálvez Salazar PF, Cadena Aguirre DP, González Poma GV, et al. Wilkie’s syndrome, a missed opportunity. J Surg Case Rep, 2018; 2018(9): rjy246.
- Khemakhem R, Ben Dhaou M, Sarrai N, Ould Med Sghair Y, Nouira F, Chariag A, et al. [A rare cause of bowel obstruction in children: the superior mesenteric artery syndrome]. Tunis Med, 2011; 89(7): 653‑654.
- Güngörer V, Öztürk M, Arslan Ş. A rare cause of recurrent abdominal pain; the coexistence of Wilkie’s syndrome and nutcracker syndrome. Arch Argent Pediatr, 2022; e202102373.
- González Hermosillo-Cornejo D, Díaz Girón-Gidi A, Vélez-Pérez FM, Lemus-Ramírez RI, Andrade Martínez-Garza P. [Wilkie Syndrome. A case report]. Cir Cir, 2017; 85(1): 54‑59.
- Adame JD, Falconi G, Harberger S. A Case of Wilkie’s Syndrome: Consideration of Alternative Diagnosis in the Setting of Chronic Abdominal Pain. Cureus, 2019; 11(11): e6074.
- Oguz A, Uslukaya O, Ülger BV, Turkoglu A, Bahadır MV, Bozdag Z, et al. Superior mesenteric artery (Wilkie’s) syndrome: a rare cause of upper gastrointestinal system obstruction. Acta Chir Belg, 2016; 116(2): 81‑88.
- Fall M, Bâ PA, Touré FB, Mbaye PA, Ngom G. [Aorto-mesenteric compression syndrome in children: report of a case]. Pan Afr Med J, 2014; 19: 151.
- Fiorini S, Sáenz Tejeira MM, Tennina C, Tomezzoli S, Requejo N. [Superior mesenteric artery syndrome (Wilkie syndrome): case report]. Arch Argent Pediatr, 2008; 106(6): 546‑548.
- Tidjane A, Tabeti B, Benmaarouf N, Boudjenan N, Bouziane C, Kessai N. [Superior mesenteric artery syndrome: rare, but think about it]. Pan Afr Med J, 2014; 17: 47.
- Le Moigne F, Lamboley JL, Vitry T, Stoltz A, Galoo E, Salamand P, et al. Superior mesenteric artery syndrome: a rare etiology of upper intestinal obstruction in adults. Gastroenterol Clin Biol, 2010; 34(6‑7): 403‑406.
- Rodríguez Caraballo L, Carazo Palacios ME, Ibáñez Pradas V, Rodríguez Iglesias P. [Wilkie syndrome: A differential diagnosis of abdominal pain]. An Pediatr Barc Spain 2003, 2015; 82(6): 445‑446.
- Lima Silva A, Antunes D, Cordeiro E Cunha J, Nogueira R, Fernandes D, Salazar T, et al. Epigastric Pain and Weight Loss - A Case of Wilkie’s Syndrome. Eur J Case Rep Intern Med, 2020; 7(5): 001557.
- Pastén González A, Muñoz Araneda A, Peirano Bastías A, Rojas Castro S, Henríquez Alessandrini V. [Superior mesenteric artery syndrome. A case report and review of the literature]. Cirugia Pediatr Organo of Soc Espanola Cirugia Pediatr, 2016; 29(4): 180‑183.
- Ali T, Tomka J, Bakirli I, Bakirov I. Surgical Treatment of Wilkie’s Syndrome by Vascular Transposition. Cureus, 2022; 14(4): e24251.
- Requena-López AA, Mata-Samperio BK, Cuadra-Reyes LA, Casillas-Vargas R. Wilkie’s syndrome as a cause of bowel obstruction in adults: A case report. Cir Cir, 2020; 88(2): 185‑188.
- Agha RA, Franchi T, Sohrabi C, Mathew G, pour le groupe SCARE. La ligne directrice SCARE 2020: Updating Consensus Surgical CAse REport (SCARE) Guidelines, International Journal of Surgery, 2020; 84: 226-230.

