Dehiscence of the Superior Semi-Circular Canal
Safaa Choayb*, Yahya El Harras, Amal Lahfidi, Firdaous Touarsa, Meriem Fikri, Najoua Ech-Cherif El Kettani and Mohamed Jiddane
Neuroradiology Department, Ibn Sina University Hospital Center, Morocco
Received Date: 22/05/2023; Published Date: 12/09/2023
*Corresponding author: Safaa Choayb, MD, Neuroradiology Department, Ibn Sina University Hospital Center, Rabat, Morocco
Abstract
Superior Semi-circular Canal Dehiscence (SSCD) can be found when the superior semi-circular canal is not covered by bone, which can cause vestibular or visual manifestations. A high-resolution CT scan permits the diagnosis with a low rate of false positives. We present the case of a 12-year-old female child with a 1-month history of dizziness secondary to SSCD of the left ear.
Keywords: Superior semi-circular canal; Superior semi-circular canal dehiscence; Vertigo; Tulio phenomena
Introduction
Superior semi-circular canal’s lack of bony covering defines SSCD. The dehiscence is responsible for the alteration of fluid dynamics, and patients often present vestibular manifestations triggered by exposure to loud noises [1]. CT scanning is a crucial diagnostic method, particularly if special reconstruction planes are used [2]. Our case involves a female child of 12 years old with a 1-month history of dizziness secondary to dehiscence of the bone covering the superior semi-circular canal of the left ear.
Case Presentation
We describe a case of a female child of 12 years, with no known comorbidities. She had a previous history of left middle ear otitis that required medical treatment 3 months ago and was well treated. The patient presented to the department of radiology with a 1-month history of dizziness. No otorrhea, hearing loss, or otalgia were reported. Her otologic examination was normal. A CT scan of the temporal bone was requested to rule out a recurrence or complication of her previous otitis episode. On CT there was no soft tissue density within the middle ear cavity, a thickened or perforated tympanic membrane, or bone erosion suggesting any infectious origin. On the other hand, it showed a dehiscence of the bone recovering the left SSC. The other internal middle ear structures were unremarkable. The patient had suffered from occasional dizziness episodes reported essentially after hearing loud noises, she was managed conservatively by avoiding the trigger. Surgery was not recommended as the patient showed noticeable improvement.
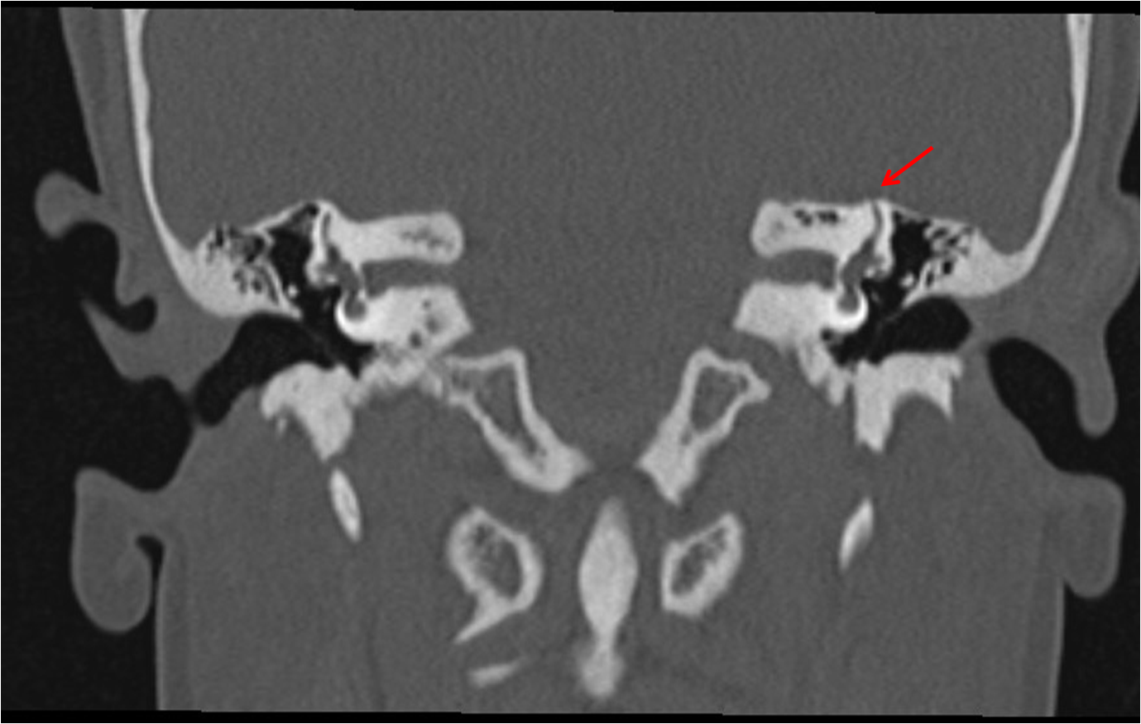
Figure 1: Coronal reconstruction of temporal bone CT scan revealing dehiscence of the bone recovering the left SSC (red arrow).

Figure 2: A CT scan obtained in both the parallel (A) and the perpendicular (B) planes to the SSC confirms dehiscence of the left SSC bone covering (red arrows).
Discussion
SSCD was first described in 1998 by Miner et al. [1,3]. It is secondary to the absence of the bone covering the membranous labyrinth of the SSC [4]. The dehiscence of SSC associated with clinical disequilibrium phenomena is referred to as the SSCD syndrome [1].
Cadaveric studies reported that SSCD was found in 0,5%, and SSC thinning (0.1mm) in 1.4% [3]. However, the radiologic prevalence is between 3 and 12% [1].
The lack of the bony coverage of the SSC creates an additional or third mobile window exposing the membranous semi-circular canal to the middle cranial fossa, creating abnormal fluid dynamics [1].
The cause of this condition is uncertain; it could be either acquired or congenital. It was proposed that SSCD may be secondary to the primitive otocysts’s malposition and disturbance of the mesenchymal cell migration amid the developing of the SSC’s apical cap. Karimnejad et al. have also proposed that the temporal-parietal lobe size disparity can increase intracranial pressure and cause bone erosion [5]. In addition, SSCD has been identified in patients with labyrinth or brainstem malformations [4]. The association of SSCD and other ear anomalies supports the congenital theory. Neurodevelopmental disorders can also be associated, such as Down syndrome, cerebral palsy and autism spectrum disorder. Children with these syndromes have lower bone mineral densities [5].
Another finding reported is an under pneumatized mastoid complex. This condition can lead to a thin SCC roof. In children, a small head injury or middle ear infection may result in complete dehiscence. On the other hand, in the adult population, chronic ear infections (such as cholesteatoma and granulation tissue) and low mastoid complex volume are considered risk factors [6].
SSCD is more common as people get older, and it may be linked to osteoporosis, which can lead to systemic bone demineralization [1].
In the paediatric population, the incidence of SSCD is approximately 10% and is higher before age 2, probably due to a congenital predisposition. In patients younger than 2, some false positives could result from a thinned tegmen tympani. Males are affected more than females, which is the opposite in adults. It is likely because of differences in how the temporal bones grow based on sex and growth hormone production [5].
The study by Lagman et al., including 122 patients, showed a preference for the right side, which is the opposite finding in adults. An associated dehiscence or thinning of the opposite side has also been reported [5].
Patients with SCCD may report vestibular and visual manifestations. The classic presentation is the Tullio phenomenon, defined by sound-induced vertigo, imbalance, and oscillopsia. The induced noise can be traffic noise, dental drills, or human screams. Pressure-induced nystagmus (the Hennenbert sign) can be seen in many vestibulopathies, but it could be suggestive of SSCD if the eye’s movement is in the same plane as the SSC’s plane. The other signs are conductive hearing loss, tinnitus, autophony, hyperacusis, aural fullness, oscillopsia, and headache. Some patients may only present a longstanding unbalance. Caution should be taken when interpreting these signs, as they can overlap with other pathologies such as perilymphatic fistula, osteosclerosis, and a patulous Eustachian tube. However, 10% of patients can be asymptomatic [1,3,5,6].
A high-resolution CT scan confirms this condition after audiometry and vestibular tests raise suspicions [3]. At the start, most studies demonstrated SSCD based on coronal slices. In 2003, according to Berden et al., the use of 0.5 mm slices that have been reformatted in the SSC’s plane provides a positive prediction value up to 95%. Using parallel and perpendicular reconstructions for SSC (also called Pöschl plane and Stenvers plane respectively) can improve detection and reduce partial volume [6].
SSCD is detected on MRI using thin (0.7mm-0.8mm) and heavily T2-weighted sequence slices on FIESTA (fast imaging employing steady-state acquisition) or CISS (constructive interference in steady-state). The absence of the bony hypointense signal that separates the high signal of CSF and labyrinth fluid defines the dehiscence [6].
MRI has a negative predictive value of 100%, confirmation by CT scan is not required to validate the roof’s integrity. However, if the examination is positive for SSCD, a CT scan is indicated given MRI’s low level of positive predictive value [6].
Treatment can be conservative by avoiding triggers, using medical management, tinnitus retraining therapy, hearing aids, and following-up with imaging. Patients who do not improve from non-operative measures or who have severe manifestations are candidates for operative treatment [5]. Surgery can include plugging or resurfacing the bone covering the canal [2].
Conclusion
SSCD can be seen in both children and adults. It can be congenital or acquired. Patients may present with Tullio phenomena, but other vestibular or visual manifestations are common. High-resolution CT scans using parallel and perpendicular planes permit the diagnosis with a low rate of false positives. Treatment is conservative, but surgery is recommended in cases of severe symptoms or failure of non-operative measures.
Acknowledgment: This research did not receive any specific subsidy from public, commercial or not-for-profit funding organizations
Conflict of interests: The authors declare that they have no links of interest.
Written informed patient consent for publication has been obtained
References
- Sood D, Rana L, Chauhan R, Shukla R, Nandolia K. Superior semicircular canal dehiscence: A new perspective. European Journal of Radiology Open, 2017; 4: 144–146. doi: 10.1016/j.ejro.2017.10.003.
- Ceylan N, Bayraktaroglu S, Alper H, Savaş R, Bilgen C, Kirazli T, et al. CT imaging of superior semicircular canal dehiscence: added value of reformatted images. Acta Otolaryngol, 2010; 130(9): 996-1001. doi: 10.3109/00016481003602108. PMID: 20205621.
- Berning AW, Arani K, Branstetter BF 4th. Prevalence of Superior Semicircular Canal Dehiscence on High-Resolution CT Imaging in Patients without Vestibular or Auditory Abnormalities. AJNR Am J Neuroradiol, 2019; 40(4): 709-712. doi: 10.3174/ajnr.A5999. Epub 2019 Feb 28. Erratum in: AJNR Am J Neuroradiol. 2019; 40(7): E39. PMID: 30819770; PMCID: PMC7048515.
- Gartrell BC, Gentry LR, Kennedy TA, Gubbels SP. Radiographic Features of Superior Semicircular Canal Dehiscence in the Setting of Chronic Ear Disease. Otology & neurotology : Official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology, 2014; 35(1): 91. https://doi.org/10.1097/MAO.0b013e3182a03522
- Lagman C, Ong V, Chung LK, Elhajjmoussa L, Fong C, Wang AC, et al. Pediatric superior semicircular canal dehiscence: illustrative case and systematic review. J Neurosurg Pediatr, 2017; 20(2): 196-203. doi: 10.3171/2017.3.PEDS1734. Epub 2017 May 26. PMID: 28548616.
- Bhatt AA, Lundy LB, Middlebrooks EH, Vibhute P, Gupta V, Rhyner PA. Superior Semicircular Canal Dehiscence : Covering Defects in Understanding from Clinical to Radiologic Evaluation. Clin Neuroradiol, 2021; 31(4): 933-941. doi: 10.1007/s00062-021-01037-x. Epub 2021 Jun 7. PMID: 34097081.

