Fortuitous Discovery of Gerbode Defect During an Extension Evaluation of Behçet's Disease: About a Clinical Case and Review of the Literature
Nacocan Mango D, Hamissou I*, Raissouni R, Insumbo P, Bucal Nacocan D, Mehssani Z, Blata V, Pr. Oukerraj and Pr. Cherti M
Department of Cardiology B, CHU Ibn Sina, University Hospital Center, Mohammed V University, Rabat, Morocco
Received Date: 15/05/2023; Published Date: 05/09/2023
*Corresponding author: Hamissou I, Department of Cardiology B, CHU Ibn Sina, University Hospital Center, Mohammed V University, Rabat, Morocco
Abstract
Less than 1% of all congenital cardiac diseases are Gerbode defects, which are extremely rare. It involves a left to right shunt and consists of a communication between the left ventricle and the right atrium. Specifically, Gerbode distinguishes between two types: direct and indirect [1].
We report the case of a 56-year-old man who was incidentally found to have Gerbode's disease during a recent hospitalization at the Internal Medicine service. He had previously been in the hospital at the Vascular Surgery service after being admitted via the emergency room due to severe abdominal pain. A ruptured infra-renal abdominal aortic aneurysm was identified through clinical and radiological investigations, and it was surgically repaired with a prosthetic aorto-iliac shunt. He underwent an exhaustive examination in the internal medicine department following surgery because Behçet's illness was thought to be present. In light of the symptoms of unusual chest pain, our cardiology department was asked to provide an opinion. Cardiac examination indicated no symptoms of right heart failure or pulmonary edema, but there was an audible systolic murmur throughout the precordium and with posterior irradiation, as well as a fremitus along the left sternal boundary. The chest X-ray did not reveal cardiomegaly, and the electrocardiogram displayed a regular sinus rhythm with an incomplete right bundle branch block (RBBB); a 7 mm perimembranous septal defect was discovered during trans-thoracic ultrasonography (TTE). A few months from now is the anticipated timeframe for the defect's closure.
Keywords: Behçet; Gerbode; Congenital Heart Diseases; Ventricular Septal Defects; Echocardiography; Endocarditis; Subrenal Aneurysm
Introduction
The so-called Gerbode ventriculo-atrial defect is a rare ventricular septal defect that allows the left ventricle to shunt into the right atrium, characterized by communication between the left ventricle (LV) and the Right Atrium (RA), representing approximately 0.08% of intracardiac shunts and less than 1% of congenital heart defects [1,3]. Although it is classically of congenital etiology, secondary causes have been reported for infective endocarditis, myocardial infarction (MI) and iatrogenesis [4]. It was first described in 1857, but only in 1956 was the first successful surgery for this anomaly reported by Kirby at the Hospital of the University of Pennsylvania [1,5]. The most striking physical examination finding of a LV-AD shunt is a characteristic IVC-like murmur: loud, raspy, pansystolic, grade III-VI, invariable with breathing and often associated with a fremitus along the left sternal border. Among all Gerbode's patients with a heart murmur, about 72% have a systolic murmur, which is often audible throughout the precordium and radiates posteriorly [2]. Diagnosis is difficult being that it is often oligosymptomatic or asymptomatic. Its diagnosis is commonly performed with transthoracic and transesophageal echocardiography; as occurred in our patient.
The treatment is surgical and has a very good efficacy rate with few recurrences.
We report this case because of its rarity and the way it was diagnosed for the benefit of the scientific community and cardiologists in particular.
Case Report
A 56-year-old man, smoker, with no personal or family history of cardiovascular disease, admitted to the emergency department for acute abdominal pain consistent with acute rupture of an infrarenal abdominal aortic aneurysm, treated surgically. After surgery, he was then admitted to the internal medicine department for extensive examinations, since Behçet's disease was suspected.
During his hospitalization in the internal medicine department, he complained of atypical chest pain so we were asked for an opinion. During cardiac examination we found an audible systolic murmur throughout the precordium and with posterior irradiation, as well as a fremitus along the left sternal border, but with no signs of right heart failure and no signs of pulmonary edema.
The electrocardiogram followed a regular sinus rhythm with axis shifted to the right and a completely Right Bundle Branch Block (RBBB) (Figure 1), and the chest X-ray showed no cardiomegaly (Figure 2).
The patient had no fever, and blood laboratory tests revealed elevation of WBCs and C-reactive protein to 150 mg/L. Urine cytobacteriology revealed leukocyturia without bacteriuria and urine culture was negative. Antibiotic therapy was started with a decrease of CRP to 20 mg/L.
A Trans-Thoracic Ultrasound (TTE) was performed which revealed a 7 mm perimembranous septal defect with normal tricuspid septal leaflet (Figure 3.1), high-velocity systolic flow (4.6 m/s with a maximum gradient of 84 mmHg) originating in the superior membranous septum and directed to the right atrium (Figure 3.2), with RA dilation at 20 cm2 (Figure 4.2), normal pulmonary artery diastolic pressure estimated from the pulmonary regurgitant velocity. The interauricular septum was flat. Absence of vegetations or cardiac thrombi within the cavitary. After the patient had fully recovered from the surgical procedure to treat the abdominal aortic aneurysm, the defect was scheduled for surgical repair.
The patient is currently being monitored by the cardiovascular surgery service.
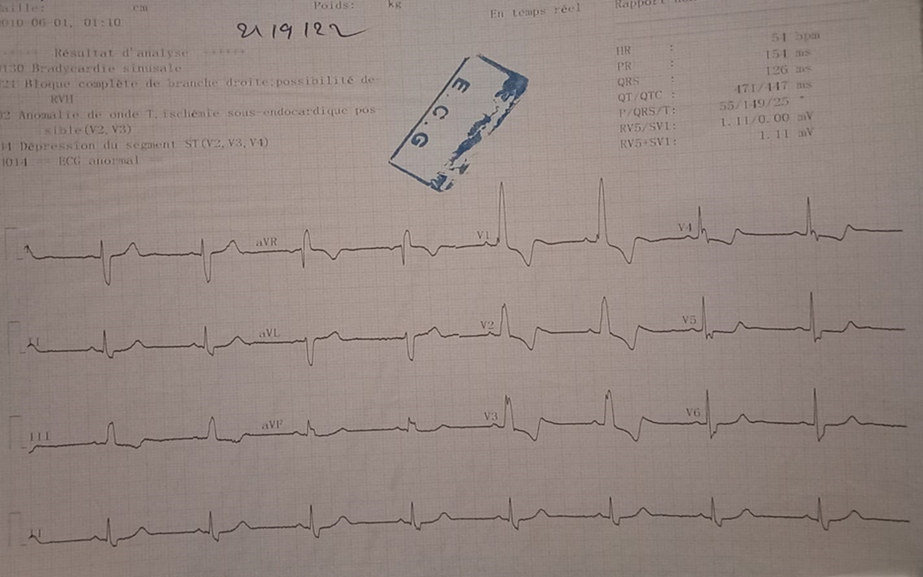
Figure1: The electrocardiogram followed a regular sinus rhythm with axis shifted to the right and a complete right bundle branch block (RBBB).

Figure2: Chest X-ray showed no cardiomegaly.

Figure 3: Transthoracic echocardiography images.
Figure 3.1: Apical four cavity in 2D mode showing a 7mm LV-RA communication.
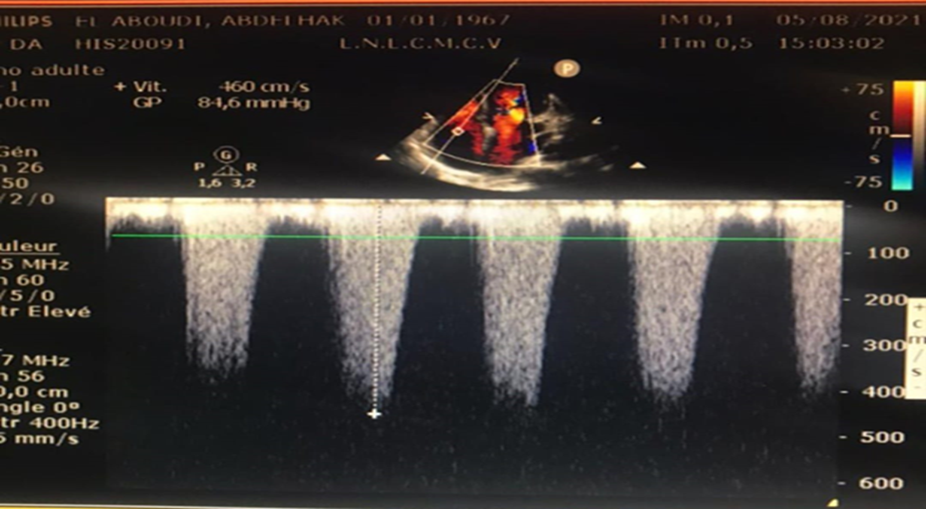
Figure 3.2: Continuous Doppler through the shunt from the left ventricle to the right atrium revealed a high-velocity systolic jet 4.6 m/s, with a maximum gradient of 84.6 mm Hg along it.
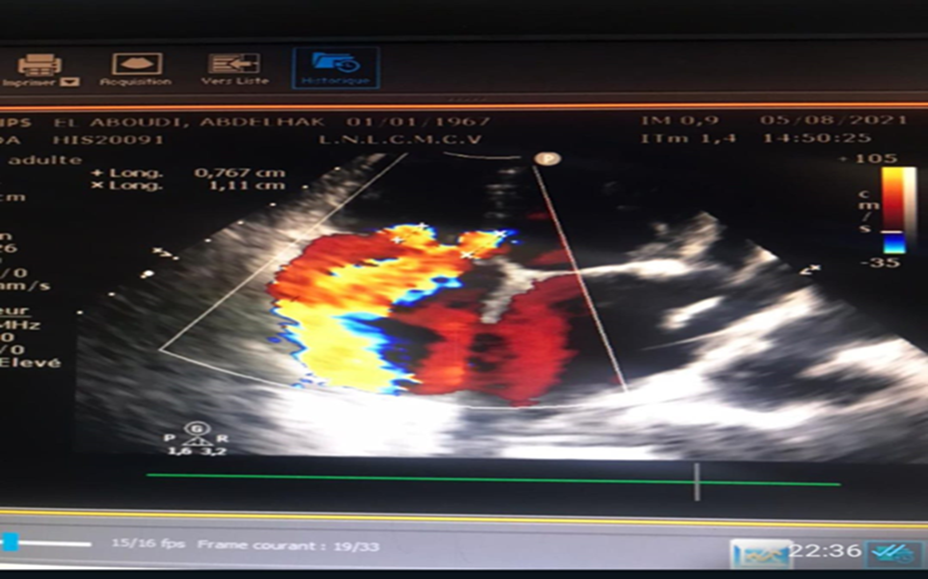
Figure 4: Transthoracic echocardiography images.
Figure 4.1: Apical four cavity in Doppler mode with color flow mapping showing flow from the left ventricle to the right atrium.

Figure 4.2: Apical four-chamber in 2D mode showing biatrial dilatation;
LA=left atrium; LV=left ventricl.
RA= rait atrium; RV= rait ventricl.
Discussion
The Gerbode defect is a ventriculo-atrial defect, causing the passage of oxygenated blood from the left ventricle to the right atrium at high velocity, as seen in our patient with a mean velocity of 4.6 m/sec and gradient of 84 mmHg.
The lesion is congenital or acquired from multiple causes: infectious, endocarditis, after heart surgery, traumatic. In a review by Yuan et al, congenital etiologies accounted for 26.4%, while the acquired form accounted for 72.7% of reports [4].
Gerbode defects are caused by anatomical deficiency of the membranous septum which is divided into two anatomical portions depending on the relationship with the septal leaflet of the tricuspid valve and two types are described: The direct Gerbode defect is rarer than the indirect and occurs in the membranous part of the ventricle, septum above the tricuspid valve and allows blood to be shunted from the left ventricle directly into the right atrium as seen in our patient. The indirect Gerbode defect though the most common form of the defect, in which there is a ventricular septal defect with blood moving from the left ventricle to the right ventricle and then through a tricuspid valve defect into the right atrium.
This terminology was later modified to infravalvular and supravalvular in order to describe the location of the shunt based on its relationship to the tricuspid valve [6]. Finally, Sakakibara and Konno included a third type called intermediate, with both infravalvular and supravalvular components [6].
In both defects, the communication of the outflow tract of the left ventricle with the right atrium allows detour of blood into the right atrium during systole. If this communication is large, it can lead to volume overload and chamber enlargement which were not observed in our patient.
Diagnosis of Gerbod's defect is difficult with echocardiography. There are a lot of pitfalls and if the defect is not seen in 2D four or five chambers, it can be mistaken for tricuspid regurgitation. If Gerbode is still suspected, ETO and MRI are indicated for evaluation and diagnosis of the defect [1,3].
Six individuals with congenital Gerbode-type ventricular direct atrial defects were included in a study between 1990 and 2008 at Children's Memorial Hospital. Of these patients, three had congestive heart failure, two had developmental delays, and two had exercise intolerance (like our patient) [7]. The ages of the participants ranged from 0.4 to 19; ours was older at 56. However, the etiology in our case was likely congenital due to the lack of a history of trauma, cardiac surgery, and apparent vegetation. The ventriculo-atrial defect ranged in size from 4 to 8 millimeters, with a mean size of 6.2 millimeters, in agreement with our result of 7 mm [7].
Spontaneous closure of these defects is very rare and surgical repair is the treatment of choice with excellent results.
Conclusion
The Gerbode shunt is a rare disorder that can be congenital or acquired. Gerbode named two types of communication between the Left Ventricle (LV) and the Right Atrium (RA). Less frequently occurring than the indirect type, the direct one develops in the membranous portion of the ventricular septum above the tricuspid valve and allows blood to be shifted from the left ventricle directly into the right atrium. On physical examination, the most prominent feature is the IVC-like murmur with a fremitus along the left sternal border. and it is frequently confused for tricuspid regurgitation in TTE.
Though the prognosis is good, it can cause infective endocarditis and heart failure, and the suggested course of action is the surgical repair with favourable outcome.
References
- Takagui ASM, et al. Left Ventricular-to-right Atrial Shunt (Gerbode Defect) Associated with Interventricular Communication in a 42-year-old Patient, 2020.
- Gerbode F, Hultgren H, Melrose D, Osborn J. Syndrome of left ventricular–right atrial shunt: successful surgical repair of defect in five cases, with observation of bradycardia on closure. Ann Surg, 1958; 148: 433–446. doi: 10.1097/00000658-195809000-00012(7)p
- Saker E, Bahri GN, Montalbano MJ, Johal J, Graham RA, Tardieu GG, et al. Gerbode defect: A comprehensive review of its history, anatomy, embryology, pathophysiology, diagnosis, and treatment. J Saudi Heart Assoc, 2017; 29: 283–292. doi: 10.1016/j.jsha.2017.01.006.(1)p
- Yuan SM. Left ventricular to right atrial shunt: congenital versus acquired. Postep Kardiol Inter, 2014; 10: 185-194. doi: 10.5114/pwki.2014.45146.(2)p
- Kelle AM, Young L, Kaushal S, Duffy CE, Anderson RH, Backer CL. The Gerbode defect: the significance of a left ventricular to right atrial shunt. Cardiol Young, 2009; 19 Suppl 2: 96-99. doi: 10.1017/S1047951109991685.(3)p
- Sakakibara S, Konno S. Congenital aneurysm of the sinus of Valsalva anatomy and classification. Am Heart J, 1962; 63: 405-424. doi: 10.1016/0002-8703(62)90287-9.(8)p.
- Angela M. Kelle The Significance of a Left Ventricular to Right Atrial Shunt* Cardiology in the Young, 2009; 19(Suppl. 2): 96–99 doi:10.1017/S1047951109991685.

