Penis Necrosis, A Rare Complication of Fournier's Gangrene: Cause and Mangement
Mohamed Achraf Chadli, Mouad EL Badr, Mahmoud Alafifi*,Abderrahman Doumer, Amine Moataz, Mohammed Dakir, Adil Debbagh and Rachid Aboutaieb
Department of Urology, CHU Ibn Rochd, Casablanca, Morocco
Received Date: 08/05/2023; Published Date: 29/08/2023
*Corresponding author: Mahmoud Alafifi, Department of Urology, CHU Ibn Rochd, Casablanca, Morocco
Summary
Penile Fournier's gangrene is extremely rare due to the rich blood supply of the penis. It has only been reported in a few cases in the literature.
Prompt surgical exploration, antibiotic therapy, and meticulous postoperative care are the cornerstone in the successful mangement of this high-mortality emergency.
We present a rare case of penile Fournier's gangrene with total necrosis of the penis necessitating penectomy in a 70-year-old patient who is well advanced, with complete perineum healing.
The goal of this article is to illustrate this rare case, as well as to explain what causes it and how to manage it.
Keywords: Fournier’s gangrene; Necrosis; Penectomy; Urethritis; Cicatrization
Introduction
In 1863 JA Fournier, a French venereologist, described five cases of penis and scrotum gangrene. Sincethen more than 500 cases have been reported in the literature [1]. Penile Fournier’s gangrene is a rare rapidly progressing and potentially fatal soft tissue synergistic infection of the genitalia, perineum, perianal region, and abdominal wall [1]. Several comorbidity factors have been associated, as previous operation in the area or injury, diabetes mellitus, lupus erythematosus, and immunosuppression.
The most commonly isolated microorganisms are E. coli, Bacteroides and Streptococcus [1-3].
The mor-tality rate remains high and can reach up to 50% of the cases .Predisposing factors are diabetes, alcohol abuse, extremes of age, malignancy, chronic steroid use, cytotoxic drugs, lymphoproliferative diseases, malnutrition, and HIV infection [3].
Due to the rich vascular supply from the bulbourethral artery, isolated penile involvement in Fournier’s gangreneis not commonly seen. We present a case of Fournier’s gangrene isolated to the penis. In the light of this case, we review the predisposing factors and the management of this entity [2].

Figure 1-2: Preoperative image showedpenilnecrosis , extended to the scrotum.
Case Report
A 70-year-old man, without any particular pathological antecedents, presented for 6 days a sharp and stabbing pain located in the penis, associated with dysuria and mictional burns, without any notion of purulent urethral discharge, genitourinary trauma, urethral instrumentation, evolving in a context of feverish sensations.
The patient initially consulted a general practitioner who prescribed a non-steroidal anti-inflammatory drug. But in front of the accentuation of the symptomatology and the extension of the lesions, he consulted the emergency room and was referred to us for further treatment.
On admission his temperature was 38.8◦C and the vital signs were stable. Clinical examination revealed edema, necrosis and diffuse crepitus along the penis shaft. The scrotum was tumefied, with necrotic areas.
The rectal examination showed a prostate of firm consistency, estimated at 40g.
The patient submitted to urgent surgical intervention under general anesthesia.
Before the operation, a suprapubic cystostomy has been performed.
After a scrototomy on the medianraphe, opening of the different scrotal envelopes and liberation of the 2 testicles, all the scrotal walls were necrotic.
Several cavities were noted on the ventral, dorsal and lateral surfaces of the penis, up to its root, which were collapsed. The 2 corpora cavernosa and the urethra were totally necrotic.
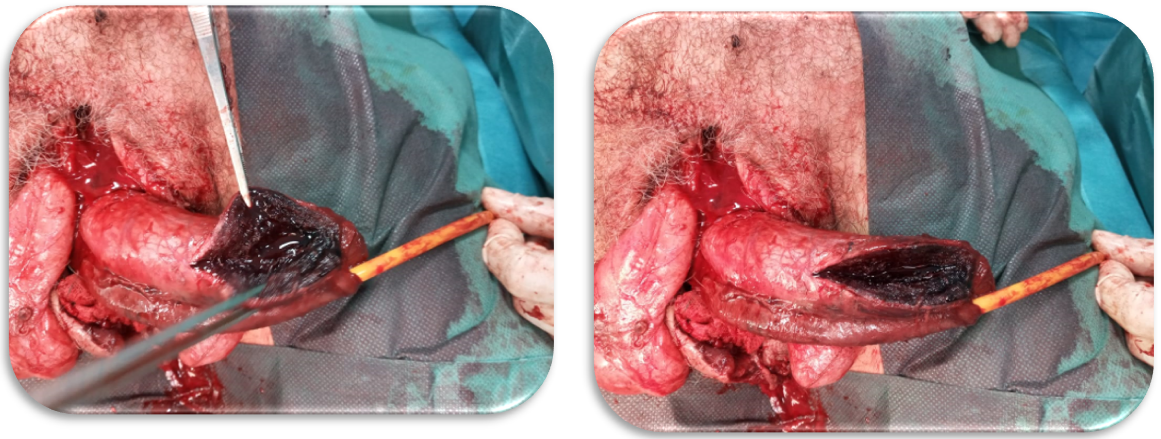
Figure 3-4: Non viable corporacavernosa and urethraplate.
A penectomy and necrosectomy of the necrotic tissues were performed, with control of hemostasis and a compression bandage

Figure 5: The operationpiece (penis).

Figure 6: Post penectomy and necrosectomy aspect.

Figure 7: Final aspect with a compression bandage.

Figure 8-9: Spontaneous re-epidermisation of defected perineal skin.
Discussion
Fournier’s gangrene is a rapid and fulminant polymicrobial infection of the fascia, with secondary necrosis of the subcutaneous tissues. Its mortality rate is high. FG affects the genital region, may affect perineal and perianal regions, and is rarely limited to the penis. It appears more frequently among males and elderly [1].
A number of the known predisposing factors for Fournier’s gangrene of the scrotum maybe present in penile Fournier’s gangrene, or it maybe idiopathic.
Some etiologic factors specific to the penis have been documented .These include penile abrasion during oral sex or following anal intercourse in homosexuals. Furthermore, penile trauma from penile self injection of cocaine has been documented .
In anterior urethral stricture, infection maybe introduced into the subcutaneous tissues from within by extravasation of infected urine into the periurethral tissues [4].
Furthermore, penile edema may predispose to infection of the subcutaneous tissues because of impaired venous and lymphatic drainage as seen in patients with congestive cardiac failure. It has also been reported to follow calciphylaxis of the penis . This is a rare condition in which there is calcium deposition in small and medium sized vessels of the skin causing ischemic necrosis associated with focal thrombosis, and intimal fibroblastic proliferation with luminal narrowing and occursmainly in patients with end-stage renal disease and diabetes [2,4].
Diagnosis is mainly based on history and clinical examination, but the physician should be experienced to suspect this rare pathology [1].
The clinical presentation of penile gangrene begins with a prodromal period of genital pain and fever followed by genitals welling, necrosis, ulceration and foulodor .
Examination reveals purulent discharge, area of necrosis and crepitus [2].
Treatment consists of rapid and aggressive surgical debridement of the necrotic tissue to bleeding edges (partial or total penectomy) under general or spinal anesthesia, suprapubic catheter insertion, removal of foreign bodies, and fluidre suscitation. Broad-spectrum antibiotics are given empirically and according to the result of the cultures [1].
Excisingdead and devitalized tissue has a very important role to play in halting the spread of infection. Care should be taken however to avoid excision of healthy tissue, especially on the penis.
This is to prevent excessive loss of tissue that could be used for reconstruction. An approach of serial debridement can be useful when in doubt. This allows time for tissues with doubt fulviability to be correctly identified as gangrenous or not [4].
Although the causes of penile ischemia and gangrene are numerous, treatment options are 2-fold—distal amputation and conservative management.
The problem with distal amputation in those patients with poor vascular supply is that poor healing of the stump may lead to more complications.
If conservative management is to be considered first, we suggest that circumcision be performed (if the patient is not circumcised) to allow better observation for disease progression as well as to allow for dry healing. This procedure may lead to sloughing of the eschar with better granulation beneath the surface. This result may be expedited by debridement of the necrotic tissue on the surface. However, if the disease progresses, either by necrotic skin on the shaft, persistent elevated white count, crepitus or induration of the shaft, then we would recommend partial or total penectomy. Since partial penectomy is technically easier and has fewer psychological consequences than total penectomy, the former is usually performed [5].
Adjuvant hyperbaricoxygen therapy can help in FG’s treatment postoperatively [1] and this through several mechanisms of action :
- Direct anaerobicactivity by tissue hyperoxygenation
- Increase in intracellular diffusion of antibiotics
- Potentiation of the phagocyticfunction
- Tissue regeneration by neoangiogenesis and fibroblastproliferation
Restoring cosmetically acceptable penile skin cover without compromising erectile function can be a major challenge after penile Fournier’s.
While remnant foreskin or scrotal skin may be used for penile skin losscoverage, most authorities prefer split thickness skin grafts for penile skin loss cover age because of the ease of use, versatility, and good take [4].
Conclusion
Isolated penile Fournier’sgangrene is a rare urological emergency. It is mostly idiopathic; however, some specific predisposing factors have been documented, particularly penile traumatism and calciphylaxis. Antibiotictherapy and debridement are the mainstay of the treatment. Split thickness skin graft is preferred to cover defected skin cosmetically.
References
- Antonios Katsimantas, Nikolaos Ferakis, Panagiotis Skandalakis, Dimitrios Filippou, "A Rare Case of Localised Isolated Penile Fournier’s Gangrene and a Short Review of the Literature", Case Reports in Urology, 2018. https://doi.org/10.1155/2018/5135616
- RayenLahouar, Sahbi Naouar, Badreddine Ben Khalifa, Wael Gazzah, Salem Braiek, Rafik El Kamel. Isolated Penile Fournier’s gangrene: A very rare entity Urology Case Reports, 2021; 37: 101608.
- Mohamad Moussaa, Mohamed Abou Chakrab. Isolated Penile Fournier’s gangrene: A case reportand literature review International Journal of Surgery Case Reports, 2019; 62: 65–68.
- Department of Surgery, Ebonyi State University, Urology Unit, Federal Teaching Hospital ; Isolated Fournier’s gangrene of the penis; Nigerian Journal of Clinical Practice, 2016.
- Constantine F Harris, Jack H. Mydlo, Ischemia and Gangrene of the Penis, The Journal of Urology, 2003; 169(5): Page 1795.

