Spontaneous Rupture of Spleen in Pregnancy- A Rare Case Report and Review of Literature
Amit Sharma* and Rakesh Gupta
Department of Forensic Medicine, Government Institute of Medical Sciences, India
Received Date: 07/05/2023; Published Date: 25/08/2023
*Corresponding author: Dr. Amit Sharma, Professor & Head, Department of Forensic Medicine, Government Institute of Medical Sciences, Greater Noida, UP, India
Abstract
Splenic hemorrhage is commonly seen after blunt abdominal trauma. Rarely, splenic hemorrhage is not associated with trauma and is termed “spontaneous” rupture. A variety of underlying conditions predispose to splenic rupture. Spontaneous splenic rupture in pregnancy is rare and occurs most commonly in the third trimester or puerperium. In addition, rheumatoid diseases, neoplasms, hematologic conditions, and some anticoagulant and antiplatelet drugs also predispose to rupture. Atraumatic hemorrhage from a nondiseased spleen, the controversial “true spontaneous rupture,” is an extremely rare and debated process. We present a rare case of spontaneous rupture of spleen in a second trimester pregnant young woman.
Keywords: Spontaneous rupture; Spleen; Pregnancy
Case Report
A 23-year-old, primigravida female in second trimester of pregnancy suddenly collapsed at her home while cooking food. She was shifted to hospital where she was declared dead on arrival. There was no history of trauma or any disease. Rupture ectopic pregnancy was provisionally suspected as cause of death and the dead body sent to the mortuary for autopsy. During postmortem examination, it was a body of a young female in early 20’s of average built showing generelized pallor. There was no evidence of any externel injuries. Stria gravidarum noted over front of abdomen. On opening of the abdominal cavity, a sudden gush of blood was noted. There was no evidence of any trauma on the anterior wall of the abdomen. All internal organs were pale. The uterus measures 26cm*12cm with no evidence of any rupture or ectopic pregnancy. The uterine cavity contains a 3-4 months dead foetus. On further exploration of the abdominal cavity, ruptured spleen of normal size and consistency was observed. The peritoneal cavity contains about 3 litres of blood. The cause of death was given as haemorrhagic shock due to spontaneous rupture of spleen (Figure 1-3).

Figure 1: Sudden gush of blood on opening the abdominal cavity.
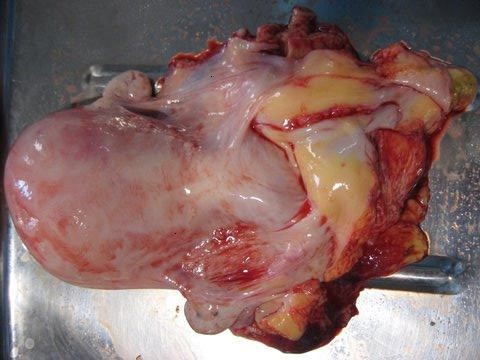
Figure 2: Normal pregnant uterus with appendages.
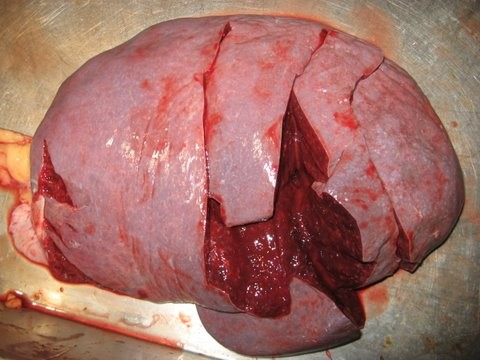
Figure 3: Rupture spleen. (The linear cuts were accidentally made during dissection).
Discussion and Review of Literature
Spontaneous rupture of the spleen in pregnancy or postpartum is an extremely rare and frequently misdiagnosed occurrence. A pubmed search could reveal only 26 cases in past 47 years. Splenic hemorrhage is commonly seen after blunt abdominal trauma. Injury to the spleen is seen in an estimated 30% of blunt abdominal trauma [1]. Spontaneous splenic rupture in pregnancy is rare and occurs most commonly in the third trimester or puerperium. The last decade has seen a dramatic shift toward successful nonoperative management of hemodynamically stable patients diagnosed with a splenic injury after blunt trauma [2]. Rarely, splenic hemorrhage is not associated with trauma and is termed “spontaneous” rupture. Spontaneous splenic rupture is a misleading term because hemorrhage actually occurs in a diseased spleen or secondary to a pathologic process [3]. A variety of underlying conditions predispose to splenic rupture. Bacterial, viral, and protozoan infections, including infectious mononucleosis and malaria, have been documented as the most common causes of atraumatic rupture [3-5].
In addition, rheumatoid diseases, neoplasms, pregnancy, hematologic conditions, and some anticoagulant and antiplatelet drugs also predispose to rupture. Atraumatic hemorrhage from a nondiseased spleen, the controversial “true spontaneous rupture,” is an extremely rare and debated process [3,6]. However, spontaneous rupture in pregnancy without antecedent trauma is rare and occurs most commonly in the third trimester or puerperium [7]. Denehy et al [8] reviewed 89 cases of splenic rupture in pregnancy, only two (2.2%) of which were documented to be spontaneous in the puerperium. To be labeled as spontaneous, the splenic rupture should not be associated with a history of antecedent trauma, any systemic disease, or evidence of gross pathology at the time of exploration, and the spleen parenchyma, vasculature, and capsule should be normal macroscopically and histologically [9]. The etiology of spontaneous postpartum splenic rupture remains speculative at best. It has been suggested that splenic enlargement and increased blood volume normally seen in pregnancy in addition to the trauma of parturition could be implicated in the pathogenesis of some cases of splenic rupture, but this is controversial. Traction with undue force with sharp- or blunt-edged instruments during cesarean delivery and insertion of packs could theoretically cause abrasive injuries to an already congested organ such as the spleen. Excessive force in exploring the upper abdomen and manual expression of the fetus by forceful pushing on the upper abdomen at the time of cesarean delivery or even while removing clots from the paracolic gutters might lead to splenic injury. Another study suggested a short splenic pedicle or deeply recessed location of the spleen as congenital factors that might contribute to rupture by compressing the diaphragm during coughing, sneezing, or vomiting [10]. The only reported case of splenic rupture in association with severe preeclampsia after the 1960s had a macroscopically and microscopically abnormal spleen; thus, it did not meet the criteria for a spontaneous rupture [11].
The differential diagnosis of spontaneous splenic rupture in the general, nonpregnant population includes local splenic disorders, such as splenic cysts and diffuse angiomatosis; hematologic diseases, such as hemophilia, congenital afibrinogenemia, and hemolytic anemia; metabolic disorders, such as amyloidosis, Wilson’s disease, Gaucher’s and Niemann-Pick disease; drug-induced, such as intravenous heparin, warfarin, and streptokinase; iatrogenic causes, such as extracorporeal shock wave lithotripsy and clamping of the portal triad; and miscellaneous, such as vomiting, uremia, systemic lupus erythematosus and other connective tissue disease. Most notable in the differential diagnosis are the infectious causes, such as infectious mononucleosis, which is considered the most common cause of spontaneous splenic rupture, as well as malaria. Patients with splenic rupture usually present with severe abdominal pain that can be localized to the left upper quadrant in the early stages and associated with chest and shoulder pain. This pain can then become generalized, with distention and rigidity in later stages. Eventually more than half of the patients will suffer hemorrhagic shock if the condition is left untreated. In this case, a picture of hemorrhagic shock was noted. Abdominal ultrasound is an inexpensive and practical way to obtain a quick diagnosis of intraperitoneal fluid accumulation or hematoma, which can be performed at the patient’s bedside or in the emergency unit [12].
This can aid in the initial workup of a patient with hemodynamic instability and abdominal distention, especially if exploration is contemplated or if computed tomography is not feasible. The reported maternal mortality of splenic rupture ranges between 0% and 45%, with a 47–82% risk of fetal wastage. This underscores the need for prompt diagnosis and management. The standard of care for patients with spontaneous postpartum splenic rupture remains emergency splenectomy. Of the 66 patients reviewed by Denehy et al [8] who underwent splenectomy, 63 survived (95.4% survival), compared with a 100% mortality rate in the 20 patients who did not undergo splenectomy. Therefore, the survival of patients with spontaneous postpartum splenic rupture rests on several factors, including aggressivetransfusion management, early diagnosis, and splenectomy. In the literature, a more conservative approach with close hemodynamic monitoring has been advocated in well-selected cases, most of which are traumatic in origin. To be eligible for nonoperative management, patients should meet several criteria, including hemodynamic stability and absence of peritoneal signs or other abdominal injuries requiring surgery. Factors that predict failure of conservative measures include preexisting splenic disease, age older than 55 years, high-grade injury, significant hemoperitoneum, and contrast blush in the spleen (suggesting false aneurysms) on computed tomography scan [13]. Splenic artery angiography followed by embolization has been described, with a reported success rate of 85% [14]. However, its role in the assessment and management of patients with hemoperitoneum is still unclear. In conclusion, spontaneous splenic rupture is a rare condition that requires immediate recognition because delay in the diagnosis can lead to catastrophic consequences. The differential diagnosis of a woman presenting in the pregnangy or during postpartum period with severe abdominal pain and distention with or without vaginal bleeding should include splenic rupture.
References
- Gorg C, Colle J, Gorg K, Prinz H, Zumaier G. Spontaneous rupture of the spleen: ultrasound patterns, diagnosis, and follow-up. Br J Radiol, 2003; 76: 704–711.
- Alonso M, Brathwaite C, Garcia V, et al. Practice Management Guidelines for the Non-operative Management of Blunt Injury to the Liver and Spleen. Eastern Association for the Surgery of Trauma; 2003.
- Debnath D, Valerio D. Atraumatic rupture of the spleen in adults. J R Coll Surg Edinb, 2002; 47: 437–445.
- Yusuf Y, Kara IH, Aldemir M, et al. Spontaneous rupture of malarial spleen: two case reports and review of literature. Crit Care, 2000; 4: 309–313.
- Kinderknecht JJ. Infectious mononucleosis and the spleen. Curr Sports Med Rep, 2002; 4: 116–120.
- Orloff M, Peskin G. Spontaneous rupture of the normal spleen: A surgical enigma. Int Abst Surg, 1958; 106: 1–11.
- McCormick GM, Young DB. Spontaneous rupture of the spleen. A fatal complication of pregnancy. Am J Forensic Med Pathol, 1995; 16: 132–134.
- Denehy T, McGrath EW, Breen JL. Splenic torsion and rupture in pregnancy. Obstet Gynecol Surv, 1988; 43: 123–131.
- Sparkman RS. Rupture of the spleen in pregnancy: Report of two cases and review of the literature. Am J Obstet Gynecol, 1958; 76: 587–598.
- Orloff M, Peskin G. Spontaneous rupture of the normal spleen: A surgical enigma. Int Abst Surg, 1958; 106: 1–5.
- Barrilleaux PS, Adair D, Johnson G, Lewis DF. Splenicrupture associated with severe preeclampsia. J Reprod Med, 1999; 44: 899–901.
- Klinkert P, Kluit AB, de Vries AC, Puylaert JBCM. Spontaneous rupture of the spleen: Role of ultrasound in diagnosis, treatment, and monitoring. Eur J Surg, 1999; 165: 712–713.
- Ochsner MG. Factors of failure for nonoperative management of blunt liver and splenic injuries. World J Surg, 2001; 25: 1393–1396.
- Firstenberg MS, Plaisier B, Newman JS, Malangoni MA. Successful treatment of delayed splenic rupture with splenic artery embolisation. Surgery, 1998; 123: 584–586.

