An Unusual Successful Treatment of UGI Bleed (MWT)
Tanveer Hussain*, Muhammad Usman Javaid, Aqsa Naseer and Anum Abbas
1HOD/ Associate Professor Gastroenterology, HFH, Rawalpindi Medical University( RMU), Pakistan
2Post graduate resident, Gastroenterology, HFH, Pakistan
3Senior Registrar, Gastroenterology, HFH, Pakistan
4Senior Registrar, Gastroenterology, HFH, Pakistan
Received Date: 19/04/2023; Published Date: 28/07/2023
*Corresponding author: Tanveer Hussain, HOD/ Associate Professor Gastroenterology, HFH, Rawalpindi Medical University( RMU), Pakistan
Introduction
Mallory-Weiss Tear (MWT) or syndrome, is a longitudinal mucosal tear or laceration of mucous membrane in the region of the gastroesophageal junction and gastric cardia. They occur commonly at Gastro- Esophageal Junction (GEJ) and sometimes extending to lower or mid esophagus and rarely to distil portion of stomach , mostly single but multiple tears can be occurred. In 1929 Kenneth Mallory and Soma Weiss reported this as lower esophageal lacerations and not ulcerations, occuring secondary to recurrent forceful retching [1], but it can occur after a single incident [2]. Many risks factors can contribute to this tear like retching, excessive vomiting, chronic alcohol intake, hiatal hernia, inflammatory disease of gastric mucosa, excessive straining during defecation and peptic ulcer disease and sometimes iatrogenic [3-6]. It occurs in approximately 3-15 % of all the causes of upper GI bleed [7]. The exact reason of this tear is still unknown but proposed mechanism is, when intra-abdominal pressure suddenly rises; it causes forceful rushing of gastric contents into esophagus resulting into longitudinal tear of mucosa. When this tear reaches the sub -mucosal arterial or venous plexus, it causes GI bleed [5]. In mild case, patient remain asymptomatic but in severe cases hematemesis, melena, dizziness, syncope and epigastric pain can occur. Upper GI endoscopy is the gold standard diagnostic modality [8].
Case Report
A 48 years old patient with no co morbid presented in Emergency department, HFH with 3 episode of hematemesis for last 6 hours preceded by nausea and retching for two days. In ER, patient has an episode of haematemesis with pain in the epigastric region. Vital signs of the patients were BP:80 systolic mm/Hg,PR:131bpm, temperature 98.6 ⁰F, SPO2: 97% at room air, physical examination was unremarkable except pallor with mild epigastric tenderness.. Lab investigations- complete blood picture: Hemoglobin:8.4 g/dl, White blood count:12.1 x 109/L,HCT 32.1%, platelets count 144 x 109/L and MCV 79.5fl. Liver function tests and renal function tests were normal at the time of presentation, anti HCV positive. USG abdomen was also normal and there were no clinical stigmata of chronic liver disease. 2 pints of blood was transfused alongwith intravenous ( i.v) crystalloids :0.9% normal saline. He was started on continuous Infusion of omeprazole@8mg/hr alongwith Infusion sandostatin (octreotide) @50ug/hr. Patient vitals improved as BP: 110/70 mm/Hg, PR: 106bpm. After one hour, patient again has 2 episodes of hematemesis. He was actively bleeding with multiple episodes of hematemesis and melena were observed in emergency department. He became restless, irritable and BP was un- recordable, managed by giving blood and fluids. His Hemoglobin dropped to 4.4g/dl within 6 hours. Patient was stabilized vitally and an Urgent Upper Gastrointestinal endoscopy was done after 16 hours.. There was a longitudinal tear present between 4 and 5’ o clock position at Gastro-Esophageal (GEJ) junction. The tear was 5 cm in length and 1.5 cm in width. Adrenaline (1:10,000) was injected at multiple sites around the tear followed by placement of 10 cm fully covered metallic stent across the GEJ (7-8 cm above and 2 cm below the GEJ). Hemostasis was achieved. Patient was shifted in intensive care unit for observation. He was given, sucralfate 10ml x 8hrs with 3 pints blood transfusion next 48 hours, patient maintained his vitals sign after 4 hours. 24 hrs after, patient was allowed liquid diet and shifted to Gastroenterology ward after 72 hrs and discharged after 5 days. He visited hospital after 4 weeks for stent removal. Stent was migrated to stomach and removed with complete resolution of the tear.
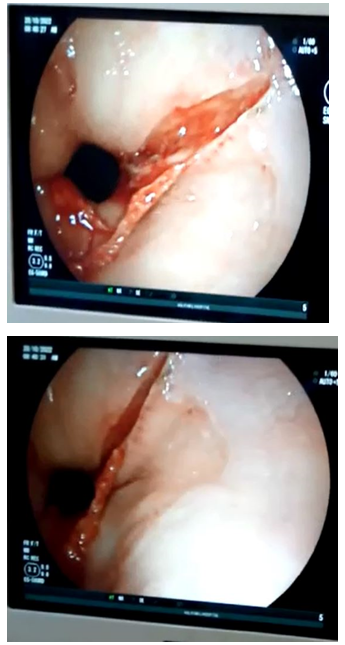
Figure 1: Pre treatment MWT.

Figure 2: Post treatment MWT.
MWT is a longitudinal mucosal or submucosal tear at gastroesophageal junction. It usually below GEJ along lesser curvature but can extend proximaly to mid esophagus. Commonly patient presents with haematemesis after an episode of forceful or recurrent retching, vomiting, coughing, or straining but epigastric or back pain can occure. Definitive diagnosis is by upper GI endoscopy but in active bleeding or if endoscopy not identified bleeding site, angiography can be diagnostic. Many factors which can predict recurrent bleed include [9], initial presentation of shock, liver cirrhosis, low hemoglobin and platelets count [10], needing blood transfusion, Intensive care unit management and active bleed at the time of endoscopy.
Mallory Weiss tear bleeding is self limiting in 80 to 90% of patients, so treatment is generally supportive in the form of antiemetic, acid suppression,sedation, fasting, blood transfusion and reversal of anticoagulation. Haemodynamically unstable patients can be manage with endoscopic intervention with adrenaline injection or fibrin sealant, electrocoagulation or argon plasma coagulation, endoscopic band ligation and mechanical hemoclip. Rarely, if endoscopic intervention failed, then interventional radiology or surgery may be required to control bleeding [11,12].
In our patient, tear was deep, around 5cm in length and 1.5cm in width , starting from GEJ (Fig) into lower esophagus with active bleeding. Patient has recurrent episodes of upper GI bleed and was haemodynamically unstable, so we decided to place covered stent. We injected adrenaline 1: 10000 at different sites folloed by placement of covered metallic stent.
Conclusion
Mallory Weiss tear is an important cause of non variceal upper gastrointestinal bleed and should be included in differential diagnosis. MWT is mostly self limiting, settled with supportive treatment but 10 to 15% patients need intervention to control bleeding. Majority bleeding controlled with endoscopic intervention.
References
- Rawla P, Devasahayam J. Mallory Weiss Syndrome. StatPearls: StatPearls Publishing, 2021.
- Graham DY, Schwartz JJM. The spectrum of the Mallory-Weiss tear, 1978; 57(4): 307-318.
- Dagradi AE, Broderick JT, Juler G, Wolinsky S, Stempien SJJTAJoDD. The Mallory-Weiss syndrome and lesion, 1966; 11(9): 710-721.
- Utzeri E, Usai PJWjog. Role of non-steroidal anti-inflammatory drugs on intestinal permeability and nonalcoholic fatty liver disease, 2017; 23(22): 3954.
- Cherednikov EF, Kunin AA, Cherednikov EE, Moiseeva NSJEJ. The role of etiopathogenetic aspects in prediction and prevention of discontinuous-hemorrhagic (Mallory-Weiss) syndrome, 2016; 7(1): 1-7.
- Na S, Ahn JY, Jung KW, Lee JH, Kim DH, Choi KD, et al. Risk factors for an iatrogenic Mallory-Weiss tear requiring bleeding control during a screening upper endoscopy, 2017; 2017.
- Yin A, Li Y, Jiang Y, Liu J, Luo HJEjoim. Mallory–Weiss syndrome: Clinical and endoscopic characteristics, 2012; 23(4): e92-e6.
- Countryman D, Norwood S, Andrassy RJSMJ. Mallory-Weiss syndrome in children, 1982; 75(11): 1426-1427.
- Kerlin P, Bassett D, Grant AK, Paull AJMJoA. The Mallory‐Weiss Lesion A Five‐Year Experience, 1978; 1(9): 471-473.
- Fujisawa N, Inamori M, Sekino Y, Akimoto K, Iida H, Takahata A, et al. Risk factors for mortality in patients with Mallory-Weiss syndrome, 2011; 58(106): 417-420.
- Terada R, Ito S, Akama F, Kidogawa H, Kashima K, Yamayoshi T, et al. Mallory-Weiss syndrome with severe bleeding: treatment by endoscopic ligation, 2000; 18(7): 812-815.
- Kortas DY, Haas LS, Simpson WG, Nickl III NJ, Gates Jr LKJTAjog. Mallory-Weiss tear: predisposing factors and predictors of a complicated course, 2001; 96(10): 2863-2865.

