Spontaneous Dissection of the Internal Carotid Artery
Targhi H1, Khalil M2,*, Fadoul-Tahir A2, Noël M2, Habboub M2, Arous S2, Benouna Gh2, Drighil A2, Azouzzi L2 and Habbal R2
1Institute of Legal Medicine, IBN Rochd University Hospital, Morocco
2Cardiology Department, IBN Rochd University Hospital, Morocco
Received Date: 08/04/2023; Published Date: 19/07/2023
*Corresponding author: Khalil Maria, Institute of Legal Medicine, IBN Rochd University Hospital, Casablanca, Morocco
Summary
Dissection of the internal carotid artery represents a cause of cerebrovascular accident in young subjects. We report a clinical case of a 33-year-old young woman who presented with spontaneous dissection of the right internal carotid artery, diagnosed by MRI angiography, after the sudden onset of clinical symptoms consisting of headaches, neck pain right and persistent ipsilateral pulsatile tinnitus. Anticoagulant treatment was started as soon as he was diagnosed. The subsequent evolution is favorable with repermeabilization of the wall of the right internal carotid artery without residual stenosis.
Introduction
Carotid dissection results from cleavage of the arterial wall by a hematoma. Depending on the location of the hematoma in the arterial wall, a distinction is made between subintimal and subadventitial dissections. Intra parietal hematoma can cause carotid stenosis or occlusion which may be complicated by more or less extensive thrombosis and embolisms responsible for established or transient ischemic attacks. The pathogenesis of supra-aortic trunk dissections is poorly understood. Dissection can occur after microtrauma following a banal activity resulting in a brutal or forced movement of the cervical spine (for example: lifting a heavy load), but the etiologies reported are multiple (sport without trauma or violent movement , coughing or vomiting, sexual activity,[1; 2].We report here a case of spontaneous internal carotid dissection without neurological manifestation.
Clinical Case
A 33-year-old patient consulted urgently for the appearance for 10 days of a picture made up of headaches, right neck pain and persistent ipsilateral pulsatile tinnitus. The only element found during the interrogation was the carrying of a heavy load 15 days earlier, there is no other element that could suggest a trauma. The clinical examination found right neck pain without previously described neurological disorders as well as pulsatile tinnitus synchronous to the pulse. A cerebral scanner was performed, no parenchymal abnormality was found. Cerebral MRI with gadolinium injection performed on day 10 revealed dissection of the right internal carotid and on the angio sections: absence of visualization of the internal carotid (Figure 1). The patient left the hospital the next day with an indication of strict rest in dorsal decubitus, a flexible neck brace, a start of low molecular weight heparin twice a day with a baldness by AVK after 04 days, a laxative and an analgesic if needed. Control cerebral imaging performed one month later shows a marked improvement in the visualization of the right internal carotid artery.
For an etiological purpose, a Doppler ultrasound of the renal arteries was performed and which revealed itself to be unremarkable.
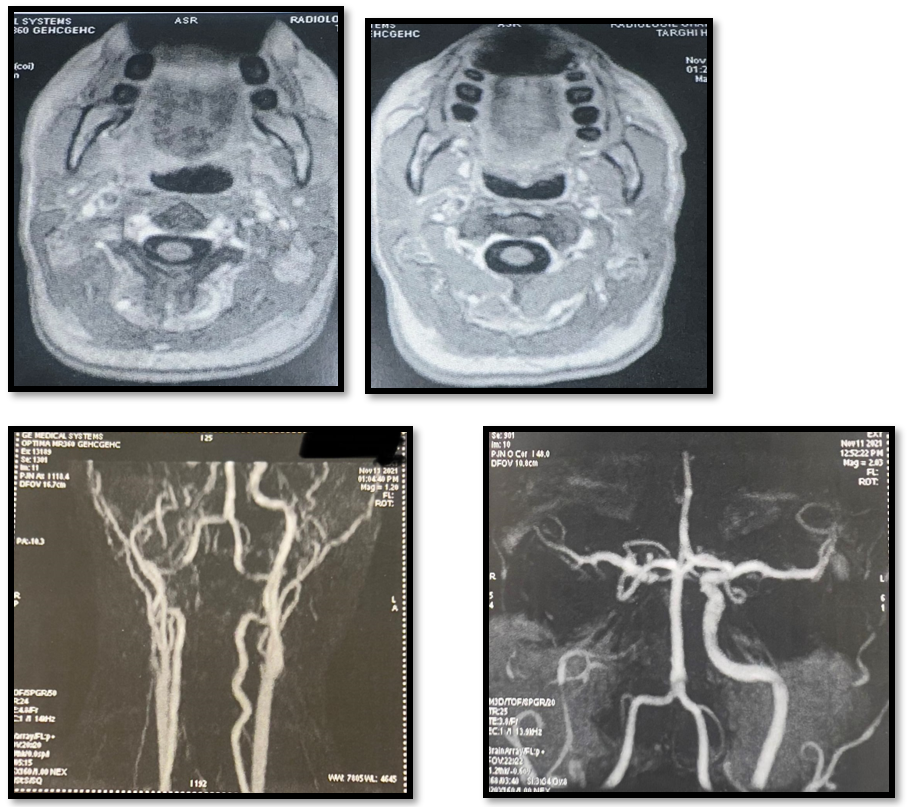
Figure 1: Neck MRI.
MRI shows no visualization of the right internal carotid
Discussion
This patient presented an acute dissection of the right internal carotid artery in its extracranial portion, without neurological consequences.
In the observation that we report, the diagnosis of fibrodysplasia is unlikely in view of the agiographic aspect of the supra-aortic trunks and the normality of the Doppler ultrasound of the renal arteries which does not highlight fibrodysplasia of the renal arteries. Frequently associated with that of the supra-aortic trunks.
According to data from the literature, the pathogenetic mechanism of spontaneous dissections of the cervical arteries appears unequivocal, although arterial hypertension poses a real problem since it has a significantly increased frequency in a population victim of spontaneous arterial dissection compared to a population witness. This mechanism boils down to a compression phenomenon of the vascular elements on the bony structures. Forced extension rotational movements of the head and neck apply by stretching the internal carotid artery on the transverse processes of the 2nd and 3rd cervical vertebrae or on the lateral masses of the atlas causing an intimal tear while the movements of forced flexion lead to compression of the internal carotid artery between the mandibular angle and the first cervical vertebra [3].
The typical clinical presentation includes a triad associating neck pain, Claude Bernard-Horner syndrome and signs of cerebral or ocular ischemia ranging from transient ischemic attack to constituted ischemic attack, but one can also find, a symptomatology frustrating, even non-existent, as we report. In all cases, the diagnosis is based on complementary examinations, the first of which is Doppler ultrasound of the supra-aortic trunks. It often confirms the diagnosis of extracranial dissection by showing stenosis or occlusion of the artery, hematoma in the arterial wall and widening of the external caliber of the artery even if the Doppler hemodynamic signs do not appear. Have no specific character. MRI, on the other hand, currently occupies a prominent place. Non-traumatic, she visualizes, on Tl-weighted axial slices, the parietal hematoma by a semi-lunar hypersignal surrounding an eccentric hyposignal corresponding to the residual arterial lumen. This characteristic aspect seems to be frequently observed in stenosing forms, but it may be lacking in occluded or aneurysmal forms [04]. In an emergency, CT angiography of ASD with 3D reconstruction, the specificity of which approaches that of conventional angiography and which is easier to access [4]. The prognosis is variable and unpredictable. The potential danger arises from the ischemic grave.
Therapeutically, there is controversy regarding either the use of anticoagulant treatments such as heparin and vitamin K antagonists, or the use of antiplatelet agents A randomized CADISS study involving 250 patients with carotid or vertebral dissection receiving either treatment with antiplatelet agents (n = 126), or treatment with anticoagulants (n = 124, unfractionated heparin or low molecular weight heparin then treatment with AVK) for three months did not show any significant difference on the occurrence of a stroke or on mortality between the two groups [5]. In practice, in the event of carotid dissection, the use of antiplatelet agents can be considered first-line.
Conclusion
Dissections of the cervical arteries represent approximately 15 to 20% of ischemic cerebral accidents in young adults. This diagnosis should be considered in the presence of any persistent and unusual neck pain and/or hemicrania. Early recognition and initiation of preventive treatment are absolutely decisive. Diagnosis is best established using MRI, which makes it possible to objectify the wall hematoma, and treatment includes anticoagulant or antiplatelet agents.
References
- Duverger V, Szymszyczin P, Singland J-D, Clement R, Vergos M. Spontaneous dissection of the internal carotid artery - 03/20/08. Doi: JMV-10-2000-25-4-0398-0499-101019-ART9.
- Sereir A-S, Bourgeois B, Incagnoli P. Cervical pain with paresthesia revealing spontaneous carotid dissection. Ann. Fr. Med. Emergency, 2020; 10: 43-45. DOI 10.3166/afmu-2019-0189
- Ngonde Sende C, Ibrahima F, Fewou A, Motah M, Njock R, Belley Priso E, et al. Post-traumatic dissections of the cervical arteries: about three cases. Health Sci. Say, 2011; 12(2).
- Goodwin R, Beery P, Dorbish R, et al. Computed tomographic angiography versus conventional angiography for the diagnosis of blunt cerebrovascular injury in trauma patients. J Trauma, 2009; 67: 1046–1050.
- Markus H, Hayter E, Levi C, et al. Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): a randomized trial. Lancet Neurol, 2015; 14: 361–367.

