Favourable Predictors of Rapid Recovery and Complete Healing in a Severe Case of Anorexia Nervosa
Federico Amianto1,*, Vanessa Leone1, Chiara Davico2, Federica Ricci2, Secondo Fassino1 and Benedetto Vitiello2
1Department of Neuroscience, University of Turin, Italy
2Department of Public Heath and Paediatric Sciences, University of Turin, Italy
Received Date: 05/04/2023; Published Date: 17/07/2023
*Corresponding author: Prof. Federico Amianto, MD, PhD, Department of Neurosciences, Via Cherasco, 11 - 10126, Turin, Italy
Abstract
Background Anorexia Nervosa (AN) typically onsets in adolescence. It displays high incidence, chronicity and mortality rates. Despite its clinical relevance and the well-known factors contributing to pathogenesis, the factors contributing to resistance to treatments are still poorly understood. As a consequence, the evidence-based treatments are still largely unsuccessful, with a substantial proportion of cases that are at high risk of developing severe and enduring AN.
Case Presentation: it is presented the history of an adult patient with AN treated with multimodal approach including: psychiatric engagement, re-nutrition, antipsychotic drug, psychotherapy, family counselling. The patients were treated in inpatient, day hospital and outpatient settings. She was followed-up until the complete and stable healing. The peculiarity of the case was that notwithstanding the initial negative prognostic elements some specific features permitted the rapid and sustained course of treatments until complete healing.
Conclusions: This case report evidences that neither the severity of denutrition, nor the lack of insight were consistent negative prognostic factors. Instead, the dependent personality traits which favoured the disease through unhealthy family dynamics, also granted a stable encouraging therapeutic relationship which promoted re-nutrition and acceptance of treatments. These permitted the substantial revision of family, relational and self-functioning dynamics through psychotherapy contributing to a rapid and sustained treatment response.
Keywords: Anorexia nervosa; Adolescence; Multimodal treatment; Therapeutic relationship; Acute phase; Follow up
Background
Anorexia Nervosa (AN) is a serious mental illness, with high mortality, but often ego-syntonic because of its psychosomatic and somatopsychic nature [1]. The pathogenesis of AN is multi factorial: genetic predisposition, biological factors, intra psychic deficit, dysfunctional attachment styles, family functioning, and social pressures are all factors that contribute to the manifestation of eating disorders but their reciprocal interactions are still object of exploration [2]. Because of the biological maintenance factors, resistance to treatments often occurs [3]; therefore, no therapeutic approaches with an acceptable remission rate exist, especially in severe forms of AN [4]. However, it is well-known that AN management requires a multi modal treatment, including psychiatric, psychotherapy, dietician and pharmacological components [5].
In severely malnourished AN patient, starvation can determine disturbances of both liver and pancreatic function, accompanied by electrolyte abnormalities and kidney injury [6,7]. Furthermore, in case of enduring and increasingly severe starvation, anaemia, severe neutropenia and thrombocytopenia until bone marrow aplasia can occur [8,9].
In addition, forced intravenous and parenteral nutritional supplementation can be complicated by metabolic syndrome known as refeeding syndrome [10], an adverse effect of nutritional treatment in AN, caused by a too rapid nutrition in an individual suffering from chronic starvation. It usually occurs within 4 days from the start of refeeding and it is shown by electrolyte disorders (especially hypophosphatemia), respiratory and cardiac failure, neurological and neuromuscular disorders.
Because of the serious consequences of malnutrition on brain tropism and dehydration, severe AN may be associated with impairment of cognitive and relational skills reaching the intensity of transient psychotic symptoms [11]. Levels of insight are often heavily compromised and accompanied by inability to build stable relationships [12]. Patients with AN often report an "emotional anaesthesia" with marked difficulty in perception and recognition of their emotions, presumably hindered by perception alterations and/or integration of bodily sensations and emotional experiences followed by the impossibility to work on such remedies consciously [13].
Malnutrition, associated with the basic structure of psychopathology, generates regressive defence mechanisms and exacerbation of relationship difficulties [14]. The medical team is experienced sometimes as a threat to the maintenance of “integrity of the disease” [15,16]. These experiences can also occur towards the family, exacerbating distortions of family relational dynamics and creating a disease reinforcement circuit [17]; in this light, family counselling could help reduce treatment duration and [18].
Despite the many pathogenic theories formulated for AN, the correlation between causative aspects of the disorder, trend of clinical condition, psychotherapeutic interventions and welfare and changes on the psychological and psychopathological plan is still very uncertain [19]. In-depth analysis in this way could allow an optimization of the interventions by improving outcomes, thus reducing chronic clinical conditions and entailing a better cost-benefit ratio.
The aim of our study is to describe a case of a hospitalized patient with extreme AN who reported an unusually positive outcome. The clinical case allowed us to highlight personality and relational contributors to the outburst of the disorder, and organic contributors to the resistance to treatment. On the other hand, it also supports a reflection on how patients’ characteristics which may have been unfavourable for the pathogenesis of the disorder could have been favourable hooks for the technical attitudes of the team. Altogether, these elements promoted the overcoming of resistance and the sustained process of remission.
Case Presentation
Patient information
The patient is a 27 years-old-woman suffering from AN restricting subtype (AN-R) (DSM 5) admitted in October 2017 at the Centre for Eating Disorders of San Giovanni Battista Hospital, University of Turin, Italy. Graduated in Business Administration with honours, waiting to achieve the qualifying examination as Auditor. At the time of onset, she was living with her family. The usual weight post menarche at the age of 16 years old was stable around 58 kg (BMI = 20.06).
Main Symptoms
When the patient was 17 years old, after a trip to America, she gained weight (about 10 kg), and she started a restrictive diet with a strict food selection achieving a weight loss of 16 kg within about 1 year (weight reached 52 kg, BMI = 17.5). From 18 to 21 years old the patient showed orthorexia tendencies. Since July 2012, following a discontinue but competitive physical activity triggered by work-related stress, an exacerbation of eating psychopathology occurred to the point of achieving a weight of 35-36 kg (BMI = 12.45) in September 2012. In October 2012, as suggested by her GP, the patient sought help as outpatient at the eating disorder centre of the University of Turin. Despite extreme emaciation (BMI was 11.25), the patient showed poor insight; blood tests revealed leukopenia, moderate anaemia, alteration of the hepatic-pancreatic values and severe hypoproteinaemia. Her mother, who attended the visit, seemed to be aware of her daughter’s disease, but did not fully recognize the need for an urgent hospitalization.
After a long motivational interview, the patient agreed to go to the Emergency Room. First the patient was admitted to an emergency medicine department because of her cardiovascular risks; after acute stabilization, she was transferred to the psychiatric unit of the Regional Pilot Centre for Eating Disorders.
Family History
Patient's mother was a 63 years old graduate in accounting, a woman with a strong sense of duty. She looked as an non-affective woman, unable to grasp patient’s emotional needs and, more in general, unable to support and direct her in facing the difficulties of life.
Patient’s 69-years-old father was working in a factory as a clerk. The patient described him as more affective but with a strong latent conflict against his wife, complaining her a lack of presence and reacting with a passive-aggressive behaviour. This situation bothered the patient who seemed intolerant towards her father's "disordered", "erratic" and "unreliable" personality traits. She also played such behaviours as a culpable neglect towards her mother, feeling that the family itself should have dealt with it. In fact, the patient felt a strong impulse to go along, protecting and serving her own mother, strongly identifying herself with the position of sacrifice and sense of duty, occupied by the mother.
Patient’s 39- year-old brother was married. He was completely independent from his family. He had his own family and a happy life even if it did not sacrifice himself as the patients did; that situation was seen in an ambivalent way by the patient. On one hand, because of his personality traits (emotional, playful, not perfectionist, ambitious) he had always been unruly, but on the other hand he had been able to interact with their parents, in particular his father, and to convey more attention on himself. This relationship led the patient to unconsciously experience an intense envy against him. She was living in a totally opposite way of life, characterized by perfectionism, ambition and lack of dedication to pleasure and emotions. Nevertheless, the patient considered his brother a landmark, because of their emotional connection.
Clinical findings
When the physician examined the patient, she showed a poor health condition, with a situation of multiple organ impairment, caused by malnutrition. She was 32.5 kg of weight (BMI = 11.1 Kg/m2). She presented peripheral edema, severe hepato-pancreatitis, severe hemodynamic instability and thrombocytopenia. From the nephrologic point of view albuminuria (20 mg /dL), phosphaturia and proteinuria were detected. Eating behaviour was characterized by severe food restriction and hyperactivity (21 hours/week). There was no illness awareness and a severe body-image distortion.
Timeline
Important dates and times in this case are summarized in Table 1.
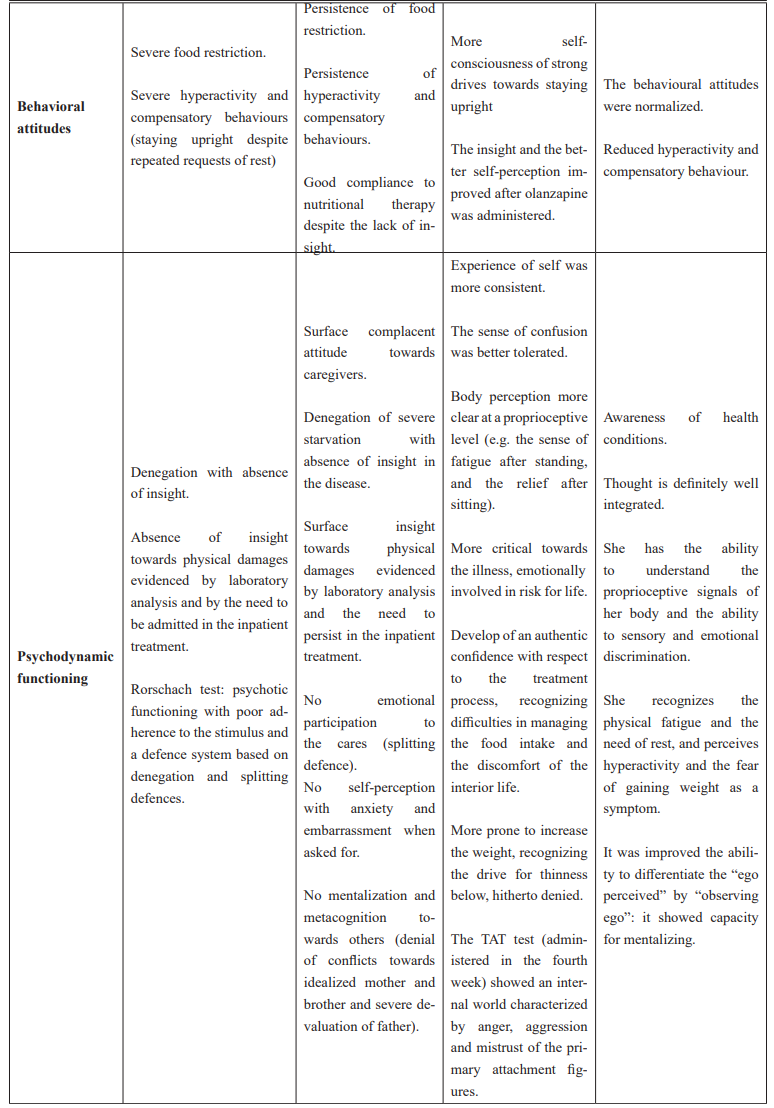
Table 1: Synoptic description of the clinical, psychological, behavioral evolution of the patient and applied psychodynamic interventions during inpatient treatment.


Diagnostic Assessment
Diagnostic Methods
-The Temperament and Character Inventory (TCI: [20]) is summarized in seven dimensions. Four dimensions are related to temperament (Novelty Seeking [NS], Harm Avoidance [HA], Reward Dependence [RD], and Persistence [P]), and three dimensions are related to character (Self-Directedness [SD], cooperativeness [C], and Self-Transcendence [ST])
- The Beck Depression Inventory (BDI; [21]) is a self-report questionnaire used to evaluate the severity of depressive symptoms; scores from 0 to 4 represent minimal depressive symptoms, scores of 5 to 7 indicate mild depression, scores of 8 to 15 indicate moderate depression and scores of 16 to 39 indicate severe depression.
-The Eating Disorder Inventory 2 (EDI – 2; [22]), a self-report inventory that measures disordered eating attitudes, behaviours and personality traits common to individuals diagnosed with ED.
-The State-Trait Anger Expression Inventory (STAXI; [23]) is used to measure the different dimensions of the feeling of anger, including the intensity, the disposition to this feeling, the temperament and the reaction to the criticism, the frequency and inhibition of expression of the same as well as the attempt to control it. The scale also provides a general index of anger expression.
In view of the severity of the clinical picture also interview-based tests were administered at different times of the hospital stay in order to evaluate the dynamic behaviour of patient's personality:
-The Rorschach test [24] is a test used upon hospital admission to assess the functioning of thoughts, to evaluate mood, and to steer the structural diagnosis of personality.
-Thematic Apperception Test (TAT; [25]) is a projective test for the study of personality. The internal consistency of the stories and the table - stimulus adequacy, the richness of verbal production, the predominant colour of the stories are emotional elements that can give clues to the patient's relational operation. The test was administered during the fourth week of hospitalization in order to clarify with greater depth the family and relationship dynamics related to the pathogenesis and maintenance of the disorder.
Prognostic characteristics
Negative prognostic features. Since its presentation the case of this patient displayed peculiar negative characteristics: a) extremely low BMI; b) extreme deterioration of the organic conditions with a progressive multi-organ failure; c) complete unawareness and denial of the disease which reached almost delusional features at the first visit; d) initial refusal of the inpatient treatment despite the evidence of life-threatening conditions; e) unawareness of the clinical severity by the family members which underestimated the life risk for months; f) complete unawareness of the relational/familial conflicts involved in the outburst of the symptoms.
Positive prognostic factors. Positive prognostic factors were: a) high intellective skills as shown by her academic achievement; b) good social adaptation and the need for a deep affective relationship; c) low score at psychopathology measures; d) a passive-dependent temperament profile with good self-directedness and cooperativeness.
Therapeutic intervention
Hospitalization at the Eating Disorders Centre of the Turin University provides an integrated interdisciplinary treatment, consisting of psychiatric care, psychodynamic therapy, nutritional assistance, dietician support, nursing and specialist's advice when required, in order to manage a multi-organ impairment condition.
The CPR DCA guarantees a daily departmental visit by the team of physicians, a psychiatric interview of psychodynamic orientation, carried by specialized professionals, dieticians’ interviews, assisted meals by trainees of the school of medicine, trained in the management of emerging issues, according with cognitive behavioural strategies. During the week two psychological-clinical interviews are also delivered with trainer and senior clinicians, clinical cognitive psychological interviews with family members, 3 dietary visits, 1 psycho educational group, an art-therapy group. According to the clinical severity during the first three weeks, the dietetic control was implemented to a daily one.
Follow-Up and Outcomes
Psychometric results
- TCI: low NS (raw score = 16; 20º percentile), medium HA (rs = 18; 45º p), high RD (rs = 19; 80º p), low P (rs = 5; 15º p); high S (rs = 25; 80º p), high C (rs = 35; 85º p), low ST (rs = 17; 25º p): personality profile compatible with passive-dependent, cyclothymic traits and an adequate character development;
- EDI-2: high levels of Body Dissatisfaction (IC = 15);
- BDI: total score = 14, no depression-related traits were detected;
- STAXI: State-Anger (S-Rab; raw score = 16; 42° percentile), Trait-Anger (T-Rab; raw score= 34; 82° percentile), Temperamental Trait Anger (T-Rab/T; raw score = 0; 7° percentile), Reactive Trait Anger (T-Rab/R; raw score= 24; 96° percentile), Introverted Anger Expression (Ax/In; raw score= 36; 99° percentile), Extraverted Anger Expression (Ax/out; raw score = 15; 54° percentile), Control of Anger Expression (Ax/Con; raw score = 17; 35° percentile), Overall Anger Expression (Ax/Ex; raw score = 80;= 93° percentile).
- The dynamic features supported by the Rorschach test (administered a week after hospital admission) consisted in a severely compromised personality functioning, identifying a bordering organization of psychotic personality. Her thoughts were characterized by abstract and dissociative mechanisms. Emotional impulses had the upper hand on intellectual functioning; her answers were often not well defined and ambivalent, with separating content, border impressions; patient’s dramatizations emphasized the vagueness of the boundaries of the self.
- The TAT test (administered in the fourth week) showed an internal world characterized by negative emotions: prevailed anger, aggression and mistrust of the primary attachment figures, responsible for splitting defence mechanisms in order to maintain a coherent sense of Self without abandoning its relational objects. Compared to the Rorschach test, patient’s thought was more adherent to the stimulus, properly supporting the hypothesis of a strong organic component in the psychotic-like attitudes of the previous weeks.
Clinical evolution
The progression of the case is presented in Table 1 which shows the parallel evolution from admission to discharge of the inpatient treatment seen from different therapeutic perspectives: the physical conditions, the nutritional approaches, the eating psychopathology and attitudes, the dynamic and relational functioning of personality. The psychodynamic interventions followed the technical indications of the B-APP [26]. For the analysis of the dynamic of personality functioning was taken as a reference the Gabbard model [27] which integrates the psychodynamic theories with the attachment theory and the implications of mentalization processes.
Treatment and follow up
After hospitalization, the patient was stepped down to the psychiatric day hospital of the same institution. The DH treatment lasted six months, and patient’s weight increased (BMI 19); while partially hospitalized she continued the exploration from the intra-psychic and relational point of view, she kept working on her father trying to consider him as more affective, more responsive to her needs and strongly challenging the mother, felt as intrusive, neglecting and highly disturbing.
After the DH treatment, the patient started a weekly individual psychodynamic psychotherapy that allowed her to continue the separation process from her mother, experiencing the anger towards her family members. The patient once again expressed the most primitive aspects of splitting defences and acting out mechanisms through a destructive aggression against the objects and injuring herself, but she never fell down in the AN psychopathology again. The patient became aware of the extreme need for emotional recognition, gaining the awareness that she had never been able to get enough reassurance to allow her to walk the pursuit of emotional independence. The patient has taken on a growing awareness that these needs were especially built by mother's personality, within family dynamics, dominated by the unresolved issues of submission and dependence of the patient's mother towards her mother herself. Finally, the patient perceived a greater integration of personal ambition and satisfaction aspects, the pursuit of pleasure and the search for a rewarding love.
The patient was discharged from the ED centre in the spring of 2017. She had a new work, a new boyfriend, new relationships with her family members and she felt that she was completely recovered by her eating disorder symptoms.
Discussion
The relevance of the present clinical case is based on five elements: 1. rapid and sustained response to treatment in a case of very extreme AN; 2. parallel evolution of both physical and psycho-pathological features with a significant shift of defence mechanisms from very low-level psychological functioning, nearly psychotic, to upper psychological functioning; 3. highly dependent personality traits which produced unfavourable relational dynamics favouring the outburst of the disorder coupled with good character development; 4. rapid change of the relational attitudes towards the components of the family with a parallel evolution in psychological and psycho-pathological functioning; 5. univocal progression towards improvement and definitive remission from symptoms at follow-up.
Multidisciplinary personalized management
The model of care applied to the patient was multidisciplinary and multimodal [28] for commissioning contemporary work of several intensive and specific therapeutic strategies [29], according to the 2004 NICE guidelines for the AN. The treatment was individualized assuming the patient in her individual uniqueness [1], i.e., considering her attachment skills and personality traits along with the physical conditions, nutrition, psychopathology, and family background. The pathogenic interweaving of biological causative nodes with psychological and socio-familiar dynamics led to a therapeutic strategy that included a non-adversarial and non-iatrogenic way the nutritional, pharmacological, psychotherapeutic, family counselling and socio-rehabilitative treatments [3]. The clinical approach thus progressively and hierarchically addressed each critical point to produce an harmonic progression overcoming the negative prognostic aspects.
Malnutrition as maintaining factor
The serious state of malnutrition reached by the patient may have resulted in a severe impairment of brain functioning [30,31]. This was accompanied by a severe alteration of perceptual skills, of the emotional and cognitive discrimination of her states of mind, and body misperception which could be described by a de-structuration of the self [32]. This involution of the functioning of the self was underlined by the regression of personality functioning that has moved on a psychotic slope, as evidenced by the Rorschach test [11,14]. This may have connected into a loop the very severe malnutrition to the defensive mechanisms of denial maintaining and worsening both the clinical and the psychological functioning [33,34].
Re-nutrition as a (partial) re-integration of the functioning of the self
Re-nutrition allowed recovery of cerebral functions along with nervous system functions [35]. According to the definition of the self as an integrative structure of integration of affective, cognitive, social, sensorimotor, and vegetative functions [32], the recovery of these aspects allowed patient to recover the "internal" sense that informs the individual of what is happening inside of her body and progressively allowed her to access to a psycho-body awareness and body-mind integration. This allowed her to experience progressively the fatigue (which was denied at intake), and the severely starved image of her body. This clinical evolution supports the theory that starvation is an attempt of self-regulation suppressing the most unfavourable emotions and affects [36]. According to the theories which relate the AN to an alteration of the development of the self [1, 37-39] these painful affects are related to attachment within family relationships. The brain malfunctioning of subjects affected with AN display’s alterations in the attachment and empathy circuits [30, 40]. According to some research [41] the process of re-nutrition progressively may have changed the functioning of the brain areas involved in the social self-perception and this may have influenced the changes in AN symptoms and psychopathology in relation to attachment dynamics.
The initial psychotic functioning of personality (i.e., the psychotic-like illness denial and bodily dysperception), confirmed by the Rorschach test, has gradually given way to a more mature operation mode which was also detected by the TAT. The thought of the patient was progressive closer to the stimulus, sleeker and more formally correct. The physical improvement also leaded to a significant reduction of the risk for liver and heart side effects, and this permitted the use of a low dose of olanzapine, which probably contributed to the reduction of anguish and to the improvement of thought [42,43].
The attachment with the therapist and the re-activation of the functioning of the self
Over the past 10 years some studies shown that emotions are a body experience [44] and that the attachment relationships are the context in which each person learns to regulate emotions [45,46]. The patient, as the other AN patient, use their symptom to regulate their emotions since their poor attachment to early caregivers did not provide instruments to regulate them adequately [37]. Parallel to the organic recovery the construction of an attachment relationship with the therapist provided a secure relational base in which the patient was able to indulge in a deep and authentic emotional listening, to re-contact parts her own self, even in the aspects of bodily awareness [1].
From a neurobiological point of view the mirror-neurons activation patterns of embodied simulation are a fundamental biological basis for understanding the other's mind and for the constitution of own self [47]. In a therapeutic relationship there is an implicitly embodied imitation which is unconscious and mutual between doctor and patient. It appears responsible for a process of change more substantial than the verbal interventions [48]. The patient, due to her dependent and cooperative attitudes permitted at relatively early phase of the treatment (in the moment in which still denying her disease she accepted the inpatient treatment) the construction of an emotional attunement with the physicians which, on turn, progressively helped her to re-experience her feelings and emotions.
Psychotherapeutic work on family relationships
The mere re-activation of the functioning of the self as concerns the integration of body perceptions (e.g., fatigue) and emotions (e.g., anger) possibly it is not sufficient to produce stable changes in the patient’s functioning and to permit a course of the disease straightforward to recovery. The therapeutic work on the emotional dynamics underlying the disorder passed through the recognition of emotional relationships with the patient family members. The progressive awareness of conflicts, ambivalence and repressed anger feelings towards the objects of attachment (mother in particular, but also father and brother) has gone in parallel because was progressively helped by the improvement of the organic component. Parallel to the physical recovery the patient progressively reduced the splitting mechanisms gaining access to greater contact with her feelings of anger.
On the other hand, the counselling to the family members produced slight but progressive changes in relatives’ attitudes towards the patient and, even more important, it helped them to accept the changes of the patient attitudes towards them which gradually arose from the new awareness of conflicting areas.
This change was also encouraged by her relatives’ positive attitudes helped by family counselling [49]. This permitted to the patient to avoid the somatization in the ED symptoms as “concretized metaphors” of her unexpressed suffering [39].
Research failed to demonstrate a linear correlation between specific behavioural patterns of family members and the outburst of the ED symptoms [30,50,51]. The emerging hypothesis is that dysfunctional family dynamics, besides being responsible for the patient insecure attachment and its consequences for the development of the self in the infancy, may have hampered the further development of the self in adolescence by the intrapsychic conflicts with attachment figures and related anger feelings. Both the fragility of the self and the repressed anger feelings are liable of a deep discomfort which leaded to the outburst of the eating disorder [1,38,39].
Patient perspective
Despite the initial extreme opposition to the inpatient treatment and the denial of the physical status the re-nutrition program, the patient was convinced by the therapeutic alliance which was favoured by personality traits and by therapists' attitudes [16]. Since the first assessment visit the therapists activated their empathic and supportive attitudes towards the patient asking her minimal efforts to verify (performing emergency exams) and stabilize the clinical conditions. Therapists avoided to speak about weight restoration as a goal of the treatment and also avoided the stigmatization of the patient because of her severe health status (e.g., “you are severely ill and thus you are not able to think correctly”), but offered an empathic participation to her life-threatening condition. They also involved the mother to reassure and support patient’s decisions. Definitely they maintained an authoritative and firm attitude towards the need of a therapeutic approach which progressively overcome the anxiety of the patient and allowed her participation in the therapeutic project.
Conclusion
The management of a severe case of anorexia nervosa should take into account a variety of clinical aspects such as: psycho-organic aspects, attachment, temperament and character features, and intra-psychic along with relational dynamics [52]. In the case of this patient all these aspects have changed with time in close connection with each other. This suggests that more than initial severity of the underweight or physical conditions or the initially immature defence mechanisms, other factors concerning attachment, dependent and relatively mature personality traits and family affective availability were more relevant in determining the course of the therapy [53,54].
This clinical case does not report the success of innovative therapeutic strategies which will overcome the resistances of any patient with AN [3]. Nevertheless, the reconstruction of patient’s therapeutic course delineates the crucial phases of a possible “ideal” evolution of the therapeutic approach to these subjects, according to both psychodynamic and enhanced-CBT models [55]. Whether supported by further studies on large samples, this therapeutic pattern may guide the treatment of any patient, even though with a different timing and technical arrangements. It would be also desirable that future clinical trials supported by neuroimaging assessment may more directly demonstrate how the relational and psychodynamic therapy coupled with nutritional interventions can rehabilitate dysfunctional brain areas associated with attachment circuits [32,37].
Declarations
Ethics approval and consent to participate
The present is a clinical case report derived from ordinary management thus no request of approval was submitted to the ethic committee of the AOU City of Health and Science of Turin. Nevertheless, it was requested to the patient and to her family the written informed consent to use this clinical case (including individuals’ details, images or videos) for anonymous publication in a scientific report.
Consent for publication
All the authors give their consent for publication in BMC Psychiatry Journal
Availability of data and material
Data and material are available from the corresponding author on reasonable request.
Competing interests
The authors have no competing interests to declare
Funding
The authors did not receive any specific funding for the treatment of this patient
Authors' contributions
All the authors contributed to the paper. FA contributed in the clinical management of the case and in the ideation, data collection, writing and revision of the paper. AS contributed in the data collection, writing and revision of the paper. VL contributed in the clinical management, data collection, drafting the paper. AG contributed in the data collection, writing and revision of the paper. GAD and SF contributed in the clinical management of the case and in the ideation, revision of the paper.
Acknowledgements
We thank the patient and her family for giving us the possibility to publish this case report. We thank Dr. Ambra Galia for her help in the preparation of the manuscript. We thank Dr. Enrica Marzola for the final language revision of the text.
References
- Fassino S. Psychosomatic approach is the new medicine tailored for patient personality with a focus on ethics, economy, and quality. Panminerva Medica, 2010; 52: 249-264.
- Bakalar JL, Shank LM, Vannucci A, Radin RM, Tanofsky-Kraff M. Recent Advances in Developmental and Risk Factor Research on Eating Disorders. Curr Psychiatry Rep, 2015; 17: 42.
- Fassino S, Abbate Daga G. Resistance to treatment in eating disorders: a critical challenge. BMC Psychiatry, 2013; 13: 282.
- Hay PJ, Touyz S, Sud R. Treatment for severe and enduring anorexia nervosa: a review. Australian and New Zeland Journal of Psychiatry, 2012; 46: 1136-1144.
- Watson HJ, Fursland A, Byrne S. Treatment engagement in eating disorders: who exits before treatment? International Journal of Eating Disorders, 2013; 46: 553-559.
- Tomita K, Haga H, Ishii G, Katsumi T, Sato C, Aso R, et al. Clinical manifestations of liver injury in patients with anorexia nervosa. Hepatology Research, 2014; 44: E26-31.
- Bouquegneau A, Dubois BE, Krzesinski JM, Delanaye P. Anorexia nervosa and the kidney. American Journal of Kidney Disease, 2012; 60: 299-307.
- Rafiullah H, Islam R, Mahmood R, Sitwala KV. Gelatinous bone marrow transformation secondary to unusual eating habits and drastic weight loss. BMJ Case Report, 2013; 16: 2013.
- Rivière E, Pillot J, Saghi T, Clouzeau B, Castaing Y, Gruson D, et al. Gelatinous transformation of the bone marrow and acute hepatitis in a woman suffering from anorexia nervosa. Revue de Medecine Interne, 2012; 33: e38-40.
- O'Connor G, Nicholls D. Re-feeding hypophosphatemia in adolescents with anorexia nervosa: a systematic review. Nutrition clinical practice, 2013; 28: 358-364.
- Delsedime N, Nicotra B, Giovannone MC, Marech L, Barosio M, Marzola E, et al. Psychotic symptoms in a woman with severe Anorexia Nervosa: psychotic symptoms in Anorexia Nervosa. Eating Weight Disorders, 2013; 18: 95-98.
- Konstantakopoulos G, Tchanturia K, Surguladze SA, David AS. Insight in eating disorders: clinical and cognitive correlates. Psychological Medicine, 2011; 41: 1951-1961.
- López-Ibor JJ, Ortiz T, López-Ibor MI. Perception, experience and body identity. Actas Espanolas de Psiquiatrìa, 2011; 3: 3-118.
- Sarró S. Transient psychosis in anorexia nervosa: review and case report. Eating and Weight Disorders, 2009; 14: e139-143.
- Mander J, Teufel M, Keifenheim K, Zipfel S, Giel KE. Stages of change, treatment outcome and therapeutic alliance in adult in patients with chronic anorexia nervosa. BMC Psychiatry, 2013; 9: 13-111.
- Vitousek K, Watson S, Wilson GT. Enhancing motivation for change in treatment-resistant eating disorders. Clinical Psychological Review, 1998; 18: 391-420.
- Treasure J, Murphy T, Szmukler G, Todd G, Gavan K, Joyce J. The experience of care giving for severe mental illness: a comparison between anorexia nervosa and psychosis. Social Psychiatry and Psychiatric Epidemiology, 2001; 36: 343-347.
- Haas L, Stargardt T, Schreyoegg J, Schlösser R, Danzer G, Klapp BF. Inpatient costsand predictors of costs in the psychosomatic treatment of anorexia nervosa. Int J Eat Disord, 2012; 45: 214-221.
- Halmi KA. Perplexities of treatment resistance in eating disorders. BMC Psychiatry, 2013; 7; 13-292.
- Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Archives of General Psychiatry, 1993; 50: 975-990.
- Beck AT. A systematic investigation of depression. Comprehensive Psychiatry, 1961; 2: 163-170.
- Garner DM. Eating Disorder Inventory 2, Professional Manual. Odessa, FL: Psychological Assessment Resources; 1993.
- Spielberger CD. Manual for the state-trait anger expression inventory (STAXI). Odessa FL: Psychological Assessment Resources; 1988.
- Rorschach H. Bern: Birker; 1981, 1921.
- Cramer P. Defence Mechanism Card Pull in TAT Stories. J Pers Assess, 2016.
- Fassino S, Amianto F, Ferrero A. Brief Adlerian psychodynamic psychotherapy: theoretical issues and process indicators. Panminerva Medica, 2008; 50: 165-175.
- Gabbard GO. Psichiatria psicodinamica, Ed. Cortina Raffaello Collana Psichiatria, psicoterapia e neuroscienze, 2015.
- Halmi The multimodal treatment of eating disorders. World Psychiatry, 2005; 4: 69-73.
- Halmi KA. Salient components of a comprehensive service for eating disorders. World Psychiatry, 2009; 8: 150-155.
- Amianto F, Abbate Daga G, Bertorello A, Fassino S. Exploring personality clusters among parents of ED subjects. Relationship with parents' psychopathology, attachment, and family dynamics. Comprehensive Psychiatry, 2013; 54: 797-811.
- Amianto F, Caroppo P, D'Agata F, Spalatro A, Lavagnino L, Caglio M, et al. Brain volumetric abnormalities in patients with anorexia and bulimia nervosa: a voxel-based morphometry study. Psychiatry Research, 2013; 30: 210-216.
- Northoff G. Brain and self - a neurophilosophical account. Child and Adolescent Psychiatry and Mental Health, 2013; 7: 28.
- Hasan TF, Hasan H. Anorexianervosa: a unified neurological perspective. Int J Med Sci, 2011; 8: 679-703.
- Hay PJ, Sachdev P. Braindysfunction in anorexia nervosa: cause or consequence of under-nutrition? Curr Opin Psychiatry, 2011; 3: 251-256.
- Riva G. Neurobiology of AnorexiaNervosa: Serotonin Dysfunctions Link Self-Starvation with Body Image Disturbances through an Impaired Body Memory. Front Hum Neurosci, 2016; 24: 10.
- Kaye WH, Fudge JL, Paulus M. New insights into symptoms and neurocircuit function of anorexia nervosa. Nat Rev Neurosci, 2009; 10: 573-584.
- Amianto F, Northoff G, Abbate Daga G, Fassino S, Tasca GA. Is Anorexia Nervosa a Disorder of the Self? A Psychological Approach. Frontiers in Psychology, 2016; 14; 7-849.
- Bruch H. Anorexia Nervosa: therapy and theory. American Journal of Psychiatry, 1982; 139: 1531-1538.
- Skårderud F. Bruch revisited and revised. Eur Eat Disord Rev, 2009; 17: 83-88.
- Cicerale A, Settanta C, D’Agata F, Caglio M, Caroppo P, Coriasco M, et al. Neuroanatomical correlates of state of mind with respect to attachment in patients with anorexia nervosa. Clinical Neuropsychiatry, 2016; 13: 41-49.
- McAdams CJ, Jeon-Slaughter H, Evans S, Lohrenz T, Montague PR, Krawczyk DC. Neural differences in self-perception during illness and after weight-recovery in anorexia nervosa. Soc Cogn Affect Neurosci, 2016; 11: 1823-1831.
- Marzola E, Delsedime N, Giovannone C, Amianto F, Fassino S, Abbate-Daga G. Atypical anti-psychotics as augmentation therapy in anorexia nervosa. PLoS One, 2015.
- Klenotich SJ, Ho EV, McMurray MS, Server CH, Dulawa SC. Dopamine D2/3 receptor antagonism reduces activity-based anorexia. Transl Psychiatry, 2015; 4: 5.
- Preston C, Ehrsson HH. Illusory changes in body size modulate body satisfaction in a way that is related to non-clinical eating disorder psychopathology. PLOS ONE, 2014.
- Fonagy P, Target M. The mentalization-focused approach to self-pathology. Journal of Personality Disorder, 2006; 20: 544-576.
- Schore AN. Early interpersonal neurobiological assessment of attachment and autistic spectrum disorders. Frontiers in Psychology, 2014; 5: 1049.
- Gallese V, Migone P, Morris N, Eagle C. La simulazione incarnata: i neuroni specchio, le basi neurofisiologiche dell'intersoggettività e alcune implicazioni per la psicoanalisi. Psicoterapia e Scienze Umane, 2006.
- Williams R, Fulford KW. Evidence-based and values-based policy, management and practice in child and adolescent mental health services. Clin Child Psychol Psychiatry, 2007;12: 223-242.
- AmiantoF, Bertorello A, Spalatro A, Milazzo M, Signa C, Cavarero S, et al. Adlerian parental counseling in eating disorders: preliminary data of a controlled clinical trial. Eat Weight Disord, 2014; 19: 303-314.
- Le GrangeD, Lock J, Loeb K, Nicholls D. Academy for Eating Disorders position paper: the role of the family in eating disorders. Int J Eat Disord, 2010; 43: 1-5.
- Amianto F, Ercole R, Marzola E, Abbate Daga G, Fassino S. Parents' personality clusters and eating disordered daughters' personality and psychopathology. Psychiatry Research, 2015; 230: 19-27.
- AmiantoF, Spalatro A, Ottone L, Abbate Daga G, Fassino S. Naturalistic follow-up of subjects affected with anorexia nervosa 8 years after multimodal treatment: Personality and psychopathology changes and predictors of outcome. Eur Psychiatry, 2017; 45: 198-206.
- Illing V, TascaGA, Balfour L, Bissada H. Attachment insecurity predicts eating disorder symptoms and treatment outcomes in a clinical sample of women. J Nerv Ment Dis, 2010; 198: 653-659.
- Zerwas S, Lund BC, Von Holle A, Thornton LM, Berrettini WH, Brandt H, et al. Factors associated with recovery from anorexia nervosa. J Psychiatr Res,2013; 47: 972-979.
- Zipfel S, Wild B, Groß G, Friederich HC, Teufel M, Schellberg D, et al. Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatients with anorexia nervosa (ANTOP study): randomised controlled trial. Lancet, 2014; 383: 127-137.

